Accessing Help for Self-Harm and Suicidal Behaviour in the Emergency Department: the Experiences of Service Users Acknowledgements
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tion on the Internet. but Convincing Fans to Actually Buy Their Music Is
FEBRUARY 2005 OK Go records its While on tour in Toronto with the Kaiser Chiefs, the members of OK Go- second album, lead singer/guitarist Damian Kulash, bassist Tim Nordwind, drummer Dan "Oh No," in Malmö, Konopka and guitar/keyboard player Andy Ross -give a video copy of a Sweden, with dance routine for the song "A Million Ways" from their new album to a fan. Tore Johansson. They had teamed with Kulash's sister Trish Sie, a former professional ballroom dancer, to choreograph the number and intended to perform the dance at the end of live shows. In mid -May, the band had filmed one of the rehearsal sessions in the backyard of Kulash's Los Angeles home. OCTOBER 25 2005 The "A Million . Ways" video is featured on VH1's "Best Week Ever" as online views top 1 million. A week later, the band and a Running handful of its fans perform the dance on The band performs "A Million Ways" on "The Tonight Show With Jay "Good Morning Leno," kicking off a media blitz in connection with the album release America," and "A in which they next do the song Sept. 9 on "Mad TV." But despite the Million Ways" tops surging viewership for "A Million Ways," the video is never formally MTVu's countdown Start submitted to MTV or VH1. "We never got a giant push from them to show "The OK Go Jogs Some Serious Digital Sales On Back Of Web Buzz BY BRIAN GARRITY play it. There was just all this hoopla around the Internet activity," says Dean's List." Rick Krim, executive VP of music and talent for VH1. -

Brynn Almli Resume 09-2017
BRYNN ALMLI COSTUME DESIGN [email protected] / brynnalmli.com COSTUME DESIGN – THEATER – FILM – DANCE Sagittarius Ponderosa NAATCO dir. Ken Rus Schmoll 2016 Birdbath Kitchen Table Works dir. Gisela Cardenas 2016 Gilgamesh Columbia University dir. Peter Petkovsek 2015 Plenty NYU Grad Acting dir. Ken Rus Schmoll 2015 Peaches and Tea Discovery Hill Productions dir. David Rey 2014 Gregory and Jane NYU Tisch Grad Film dir. Clare Sackler 2014 Alphabetical Columbia University dir. Chris Murrah 2014 Harm of Will Second Ave Dance Comp, NYU chor. Kendra Portie 2013 Landscape of the Body NYU Grad Acting dir. Pamela Berlin 2013 Midnight Circus Grounded Aerial chor. Karen Fuhrman 2013 Divergent Strands Second Ave Dance Comp, NYU chor. Callie Lyons 2013 Orange Alert Algonquin Seaport Theater dir. Leslie Silva 2011 The Classroom Slant Theatre Project dir. Lori Wolter Hudson 2011 Buddy: The Buddy Holly Story Millbrook Playhouse dir. Tiffany Green 2011 Love, Sex, and The IRS Millbrook Playhouse dir. Adam Knight 2011 Annie Millbrook Playhouse dir. Stefanie Sertich 2011 The Little Prinsinn Brooklyn Lyceum dir. Dhira Rauch 2011 ASSISTANT COSTUME DESIGN Anastasia Broadhurst Theatre des. Linda Cho 2017 Lincoln in the Bardo VR video New York Times des. Olga Mill 2016 Das Rheingold (swatcher) Minnesota Opera des. Matt LeFebvre 2016 Nutcracker Charlotte Ballet des. Holly Hynes 2016 The Get Down (PA & Coordinator) Netflix des. Jeriana San Juan 2016 Cartier private event sales & gala Van Wyck & Van Wyck des. Erin Schultz 2016 Anastasia Hartford Stage des. Linda Cho 2016 Salome Shakespeare Theatre Company des. Susan Hilferty 2015 Veils Barrington Stage Company des. Arnulfo Maldonado 2015 Damascus Square Axelrod Performing Arts Center des. -
“Rube Goldberg Machine”!
Worksheet No.1 – Build a “Rube Goldberg Machine”! A Rube Goldberg device is a machine that completes a simple task in an extraordinarily complicated way. Building one is a great way for you to explore many different ideas in physics, and to put those ideas all together to make something fun! This short worksheet is meant to help you design your machine! Check off all the ideas you’ve included in your machine, and explain how they work. You can also add physics ideas to your machine that aren’t in this list! This worksheet should be used with reference to “Challenge No. 1: Build a “Rube Goldberg Machine”, part of the “Physics & Astronomy at Home” series on the UBC Physics & Astronomy Outreach website at https://bit.ly/2Vtg8y5. ❏ Levers In the “How to Pass the Salt…” video, how are levers used around 0:36? Can you find other examples of levers in the same video? How have you used levers in your Rube-Goldberg machine? Physics & Astronomy at Home: Challenge No.1 – Build a “Rube Goldberg Machine”! https://bit.ly/2Vtg8y5 Worksheet created by Alex May, Holden Jones, and Theresa Liao page 1 ❏ Pulleys How was a pulley used in the “Simple Machine and Rube-Goldberg” video around 0:07? How is a pulley used in your Rube-Goldberg machine? ❏ Potential energy Besides the lemon at the start of the video, what’s another example where Potential Energy was used in the “Lemonade Machine” video? (Look for objects falling downwards!) Physics & Astronomy at Home: Challenge No.1 – Build a “Rube Goldberg Machine”! https://bit.ly/2Vtg8y5 Worksheet created -
Art in Space!
Art in Space Contest Digital Package: Website messaging: Art in Space! OK Go is holding a contest to send student art projects into space! Rock band OK Go is inviting elementary, middle and high school students to use their creative art and science minds to dream up cool experiments that can be sent into actual space onboard Blue Origin’s New Shepard spacecraft. The students come up with the project, and OK Go will help them make it a reality! The Art in Space contest is for students age 11-18, with the assistance of an adult mentor. No technical expertise needed -- this is a contest for great ideas. Submissions are due by May 6, 2019, and two winners will be chosen. Get more info and contest rules at https://okgosandbox.org/art-in-space Newsletter messaging: OK Go is holding a contest to send student art projects into space! Because gravity can’t hold down your creativity. Rock band OK Go filmed a video in microgravity in an airplane. Now they’re inviting students to create their own art in actual space. The band is inviting elementary, middle and high school students to use their creative art and science minds to dream up cool experiments that can be sent into actual space onboard Blue Origin’s New Shepard spacecraft. You don’t have to be an engineer -- students come up with the project, and OK Go will bring the technical expertise to help make it a reality! The Art in Space contest is for students age 11-18, with the assistance of an adult mentor. -

Surrounding Sounds
SURROUNDING SOUNDS ABOUT THIS CHALLENGE The world is full of sounds to explore. Indeed, anything can be a musical instrument with a little bit of creativity. This challenge is designed to encourage students to discover the musical qualities of various everyday objects and put them to use. Note, we chose to highlight the set of topics and standards below as a list that closely connects with this challenge. TOPICS STANDARDS Sound Science Standards (NGSS): Pitch 4-PS3-2 Make observations to provide evidence that energy Amplitude can be transferred from place to place by, sound, light, heat and electric currents. Music 4-PS4-3 Generate and compare multiple solutions that use Analysis patterns to transfer information. Using Tools to Record Data Categorizing Data Organizing Data PAGE 1 www.OKGoSandbox.org EXPLORE INSTRUMENTAL QUALITIES IN ORDINARY OBJECTS LEARNING OBJECTIVES Students will be able to: Observe and record information about the qualities of various objects. Organize that information in a convenient way. Collect and interpret data in order to help operationally define what an instrument is. Experiment with different methods and new ideas in order to determine if an object will fit their desired purpose. GETTING STARTED Show the “Needing/Getting” music video Get students excited about the STEAM concepts in this video. Go to OKGoSandbox.org and play the “Surrounding Sounds” videos. These videos will outline the challenge and explain OK Go's creative thinking behind the music video “Needing/Getting.” Go to OKGoSandbox.org and play the “Needing/Getting Q&A” video In this Q&A, OK Go explains the creative and scientific processes they went through to create the music video “Needing/Getting.” The Q&A can be shown before the challenge to inspire students, or after to answer any lingering questions they have. -

Math of OK Go
Paper ID #29943 Math of OK Go MiKyla Jean Harjamaki, Playful Learning Lab MiKyla is an undergraduate student studying mechanical engineering and math and the University of St. Thomas. She is also a student researcher in the Playful Learning Lab. Dr. AnnMarie Thomas, University of St. Thomas AnnMarie Thomas is a professor in the School of Engineering and the Opus Colluege of Business at the University of St. Thomas where she is the director of the UST Center for Engineering Education. Her research group, the Playful Learning Lab, focuses on engineering and design education for learners of all ages. Ms. Krista Schumacher, University of St. Thomas Krista is an undergraduate Elementary Education and STEM Education major at the University of St. Thomas. Abby Bensen, University of St. Thomas Ms. Emma Michelle Monson, University of St. Thomas Emma Monson is an undergraduate studying Elementary Education with a STEM co-major at the Univer- sity of St. Thomas. c American Society for Engineering Education, 2020 Math of OK Go Introduction Grammy Award-winning rock band OK Go places mathematics concepts at the heart of its exciting music videos. Through the OK Go Sandbox project, the band has partnered with the Playful Learning Lab at the University of St. Thomas to create several education guides, based on Common Core standards, that explore topics including parabolas, spreadsheets, and frame rates in engaging ways. OK Go Sandbox is a resource for teachers to access and implement in their classrooms. These guides and videos introduce educational topics, then allow students to practice and develop an understanding of them by replicating the processes used within the music videos. -

Band Hero™ Brings the Most Exciting Event of the Season to Living Rooms Around the World with Chart-Topping Hits from a Variety of Popular Acts
Band Hero™ Brings the Most Exciting Event of the Season To Living Rooms Around the World With Chart-Topping Hits From a Variety of Popular Acts First E10+ Rated Console Guitar Hero(R) Game Offers Fun for Friends and Families with Music from Taylor Swift, Nelly Furtado, Lily Allen, The All-American Rejects and Jackson 5 and many more SANTA MONICA, Calif., Oct 19, 2009 /PRNewswire-FirstCall via COMTEX News Network/ -- The most popular bands from yesterday and today will be coming to living rooms this Fall as Activision Publishing, Inc.'s (Nasdaq: ATVI) Band Hero(TM) delivers the most exciting and accessible music collection ever assembled for the entire family. The game's set list is packed with No. 1 hits, including Jackson 5's "ABC," Don McLean's "American Pie," KT Tunstall's "Black Horse and the Cherry Tree," The Turtles' "Happy Together" and Taylor Swift's "Love Story." Music fans will enjoy all of the critically-acclaimed innovations from Guitar Hero(R) 5, such as Party Play, RockFest and various Nintendo exclusive modes, in the most social music gaming experience ever as they strum, drum and sing along to their favorite, popular tunes as a full band with any combination of four singers, guitarists, bassists and drummers or simply sing together in the all-new karaoke-style Sing-Along Mode. Band Hero also offers a great value to owners of multiple Guitar Hero(R) games by allowing players to import songs from Guitar Hero 5, Guitar Hero(R) Smash Hits and Guitar Hero(R) World Tour. The week Band Hero hits store shelves, 69 tracks from the acclaimed Guitar Hero 5 will be available to importfor Xbox 360(R) video game and entertainment system from Microsoft for 480 Microsoft Points, on the PlayStation(R)3 computer entertainment system for $5.99, and Wii(TM) for 600 Wii Points(TM). -

Resource Exchange)
Paper ID #26288 Creating Instruments from Found Objects and Sensors (Resource Exchange) Dr. AnnMarie Thomas, University of St. Thomas AnnMarie Thomas is a professor in the School of Engineering at the University of St. Thomas where she is the director of the UST Center for Engineering Education. Her research group, the Playful Learning Lab, focuses on engineering and design education for learners of all ages. Dr. Deborah Besser P.E., University of St. Thomas Dr. Besser, PE, ENV SP, holds a PhD in education and MS and BS in civil engineering. Currently, she is civil engineering chair and Center for Engineering Education director. Previous experience includes fac- ulty positions in diverse universities where she has taught a variety of coursework including steel, timber, concrete and masonry design, construction, engineering economy, engineering graphics and engineering education. Prior to teaching, Dr. Besser, a licensed engineer, was a design engineer with HNTB-CA, where she worked on seismic retrofits and new design of high profile transportation structures. Ms. Paige Huschka, Playful Learning Lab Hannah French MiKyla Jean Harjamaki, Playful Learning Lab I am an undergraduate student studying mechanical engineering and math and the University of St. Thomas. I am the lab operations manager at the Playful Learning Lab Maria Baklund, University of St. Thomas Undergraduate Research Assistant for the Playful Learning Lab at St. Thomas under the direction of Dr. Annmarie Thomas. Second-year Mechanical Engineering major with a Peace Engineering minor. Has led many STEM activities and is interested in using engineering to encourage peoples’ interests and collaborate with developing countries. Esmee´ Verschoor, Playful Learning Lab Esmee´ Verschoor is a Communications and Journalism major at the University of St. -

Songs by Title
Sound Master Entertainment Songs by Title smedenver.com Title Artist Title Artist #thatPower Will.I.Am & Justin Bieber 1994 Jason Aldean (Come On Ride) The Train Quad City DJ's 1999 Prince (Everything I Do) I Do It For Bryan Adams 1st Of Tha Month Bone Thugs-N-Harmony You 2 Become 1 Spice Girls Bryan Adams 2 Legit 2 Quit MC Hammer (Four) 4 Minutes Madonna & Justin Timberlake 2 Step Unk & Timbaland Unk (Get Up I Feel Like Being A) James Brown 2.Oh Golf Boys Sex Machine 21 Guns Green Day (God Must Have Spent) A N Sync 21 Questions 50 Cent & Nate Dogg Little More Time On You 22 Taylor Swift N Sync 23 Mike Will Made-It & Miley (Hot St) Country Grammar Nelly Cyrus' Wiz Khalifa & Juicy J (I Just) Died In Your Arms Cutting Crew 23 (Exp) Mike Will Made-It & Miley (I Wanna Take) Forever Peter Cetera & Crystal Cyrus' Wiz Khalifa & Juicy J Tonight Bernard 25 Or 6 To 4 Chicago (I've Had) The Time Of My Bill Medley & Jennifer Warnes 3 Britney Spears Life Britney Spears (Oh) Pretty Woman Van Halen 3 A.M. Matchbox Twenty (One) #1 Nelly 3 A.M. Eternal KLF (Rock) Superstar Cypress Hill 3 Way (Exp) Lonely Island & Justin (Shake, Shake, Shake) Shake KC & The Sunshine Band Timberlake & Lady Gaga Your Booty 4 Minutes Madonna & Justin Timberlake (She's) Sexy + 17 Stray Cats & Timbaland (There's Gotta Be) More To Stacie Orrico 4 My People Missy Elliott Life 4 Seasons Of Loneliness Boyz II Men (They Long To Be) Close To Carpenters You 5 O'Clock T-Pain Carpenters 5 1 5 0 Dierks Bentley (This Ain't) No Thinkin Thing Trace Adkins 50 Ways To Say Goodbye Train (You Can Still) Rock In Night Ranger 50's 2 Step Disco Break Party Break America 6 Underground Sneaker Pimps (You Drive Me) Crazy Britney Spears 6th Avenue Heartache Wallflowers (You Want To) Make A Bon Jovi 7 Prince & The New Power Memory Generation 03 Bonnie & Clyde Jay-Z & Beyonce 8 Days Of Christmas Destiny's Child Jay-Z & Beyonce 80's Flashback Mix (John Cha Various 1 Thing Amerie Mix)) 1, 2 Step Ciara & Missy Elliott 9 P.M. -

Karaoke with a Message – September 29, 2018 a Project of Angel Nevarez & Valerie Tevere at Interference Archive (314 7Th St
Another Protest Song: karaoke with a message – September 29, 2018 a project of Angel Nevarez & Valerie Tevere at Interference Archive (314 7th St. Brooklyn, NY 11215) karaoke provided by All American Karaoke, songbook edited by Angel Nevarez & Valerie Tevere ( ) 18840 (Ghost) Riders In The Sky Johnny Cash 10274 (I Am Not A) Robot Marina & Diamonds 00005 (I Can't Get No) Satisfaction Rolling Stones 17636 (I Hate) Everything About You Three Days Grace 15910 (I Want To) Thank You Freddie Jackson 05545 (I'm Not Your) Steppin' Stone Monkees 06305 (It's) A Beautiful Mornin' Rascals 19116 (Just Like) Starting Over John Lennon 15128 (Keep Feeling) Fascination Human League 04132 (Reach Up For The) Sunrise Duran Duran 05241 (Sittin' On) The Dock Of The Bay Otis Redding 17305 (Taking My) Life Away Default 15437 (Who Says) You Can't Have It All Alan Jackson # 07630 18 'til I Die Bryan Adams 20759 1994 Jason Aldean 03370 1999 Prince 07147 2 Legit 2 Quit MC Hammer 18961 21 Guns Green Day 004-m 21st Century Digital Boy Bad Religion 08057 21 Questions 50 Cent & Nate Dogg 00714 24 Hours At A Time Marshall Tucker Band 01379 25 Or 6 To 4 Chicago 14375 3 Strange Days School Of Fish 08711 4 Minutes Madonna 08867 4 Minutes Madonna & Justin Timberlake 09981 4 Minutes Avant 18883 5 Miles To Empty Brownstone 13317 500 Miles Peter Paul & Mary 00082 59th Street Bridge Song Simon & Garfunkel 00384 9 To 5 Dolly Parton 08937 99 Luftballons Nena 03637 99 Problems Jay-Z 03855 99 Red Balloons Nena 22405 1-800-273-8255 Logic/Alessia Cara/Khalid A 614 A Beautiful Life Ace -
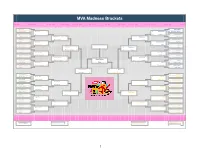
MVA Madness Brackets Final
MVA Madness Brackets First Round Second Round Sweet 16 Elite 8 Final Four Championship Final Four Elite 8 Sweet 16 Second Round First Round 1 Beyoncé 27 14 Kanye West 1 16 Paula Abdul 11 Beyoncé 9 4 Kanye West 11 The White Stripes 16 8 Sia 28 Sia 8 13 Radiohead 19 Radiohead 8 9 Jennifer Lopez. 9 Beyoncé 10 9 Radiohead 6 Weezer 9 5 Madonna 28 Missy Elliott 6 7 M.I.A. 18 Kendrick Lamar 5 12 Usher 10 Madonna 6 6 Kendrick Lamar 7 Outkast 12 4 Britney Spears 10 Missy Elliott 11 11 M.I.A. 1 Korn 4 13 Missy Elliott 25 Beyoncé 13 11 Radiohead 24 M.I.A. 13 6 Janet Jackson 33 Michael Jackson 15 17 Bjork 16 Foo Fighters 6 11 Ciara 5 Janet Jackson 11 7 Foo Fighters 8 Kylie Minogue 11 3 Justin Timberlake 24 Justin Timberlake 6 9 St. Vincent 11 Coldplay 3 14 Ne-Yo 13 Janet Jackson 8 7 St. Vincent 14 St. Vincent 14 Michael Jackson 7 Bruno Mars 36 Michael Jackson 9 10 Bjork 20 Bjork 7 10 Chris Brown 1 Bruno Mars 0 Bjork 9 Bjork 4 Fatboy Slim 10 2 Michael Jackson 34 Michael Jackson 17 8 Peter Gabriel 16 Peter Gabriel 2 15 Robyn 4 9 FKA Twigs 15 Michael Jackson 17 12 Bjork David Bowie 5 10 Janelle Monáe 1 Guns n’ Roses 5 16 Rihanna 1 16 Arcade Fire 14 Arcade Fire 9 10 Rihanna 0 Vulfpeck 16 8 Troye Sivan 6 Hayley Kiyoko 5 4 Mariah Carey 5 Ariana Grande 8 9 Hayley Kiyoko 11 Arcade Fire 7 5 Rihanna 10 Mariah Carey 9 5 LL Cool J 4 David Bowie 8 11 Lady Gaga 15 Lady Gaga 5 12 Beastie Boys 11 Beastie Boys 8 10 Lady Gaga 1 Backstreet Boys 12 4 David Bowie 14 David Bowie 9 4 Busta Rhymes 7 Talking Heads 4 13 Mary J. -

Songs by Artist
Sound Master Entertianment Songs by Artist smedenver.com Title Title Title .38 Special 2Pac 4 Him Caught Up In You California Love (Original Version) For Future Generations Hold On Loosely Changes 4 Non Blondes If I'd Been The One Dear Mama What's Up Rockin' Onto The Night Thugz Mansion 4 P.M. Second Chance Until The End Of Time Lay Down Your Love Wild Eyed Southern Boys 2Pac & Eminem Sukiyaki 10 Years One Day At A Time 4 Runner Beautiful 2Pac & Notorious B.I.G. Cain's Blood Through The Iris Runnin' Ripples 100 Proof Aged In Soul 3 Doors Down That Was Him (This Is Now) Somebody's Been Sleeping Away From The Sun 4 Seasons 10000 Maniacs Be Like That Rag Doll Because The Night Citizen Soldier 42nd Street Candy Everybody Wants Duck & Run 42nd Street More Than This Here Without You Lullaby Of Broadway These Are Days It's Not My Time We're In The Money Trouble Me Kryptonite 5 Stairsteps 10CC Landing In London Ooh Child Let Me Be Myself I'm Not In Love 50 Cent We Do For Love Let Me Go 21 Questions 112 Loser Disco Inferno Come See Me Road I'm On When I'm Gone In Da Club Dance With Me P.I.M.P. It's Over Now When You're Young 3 Of Hearts Wanksta Only You What Up Gangsta Arizona Rain Peaches & Cream Window Shopper Love Is Enough Right Here For You 50 Cent & Eminem 112 & Ludacris 30 Seconds To Mars Patiently Waiting Kill Hot & Wet 50 Cent & Nate Dogg 112 & Super Cat 311 21 Questions All Mixed Up Na Na Na 50 Cent & Olivia 12 Gauge Amber Beyond The Grey Sky Best Friend Dunkie Butt 5th Dimension 12 Stones Creatures (For A While) Down Aquarius (Let The Sun Shine In) Far Away First Straw AquariusLet The Sun Shine In 1910 Fruitgum Co.