Thesis Approval
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Palestinian Authority (PA) Fight Against COVID-19 (Updated to March 31, 2020)
רמה כ ז מל ו תשר מה ו ד י ע י ן ( למ מ" ) כרמ ז מה י עד מל ו ד י ע י ן ול רט ו ר רמה כ ז מל ו תשר מה ו ד י ע י ן ( למ מ" ) כרמ ז מה י עד מל ו ד י ע י ן ול רט ו ר רמה כ ז מל ו תשר מה ו ד י ע י ן ( למ מ" ) כרמ ז מה י עד מל ו ד י ע י ן ול רט ו ר רמה כ ז מל ו תשר מה ו ד י ע י ן ( למ מ" ) כרמ ז מה י עד מל ו ד י ע י ן ול רט ו רור The Palestinian Authority (PA) Fight Against COVID-19 (Updated to March 31, 2020) March 31, 2020 Data of the Spread of COVID-19 in the PA Territories On March 31, 2020, the number of Palestinian COVID-19 cases rose to 117, 107 in Judea and Samaria and 10 in the Gaza Strip.1 The cases most recently detected in the PA were a Palestinian worker who returned from Israel and seven Palestinians in the village of Qatanna, northwest of Jerusalem. The village and the Bethlehem area are focal points for the spread of the disease: there are 39 COVID-19 cases in Qatanna and 46 in the Bethlehem area. So far 18 Palestinians have recovered and one has died (Wafa, March 31, 2020; Palestinian TV, QudsN Facebook page, March 30, 2020). Dr. Ghassan Nimr, spokesman for the Palestinian ministry of the interior, briefed journalists on March 30 and 31 about the geographic distribution of COVID-19 in the PA territories. -

Protection of Civilians Weekly Report
U N I TOCHA E D Weekly N A Report: T I O 28N FebruaryS – 6 March 2007 N A T I O N S| 1 U N I E S OFFICE FOR THE COORDINATION OF HUMANITARIAN AFFAIRS P.O. Box 38712, East Jerusalem, Phone: (+972) 2-582 9962 / 582 5853, Fax: (+972) 2-582 5841 [email protected], www.ochaopt.org Protection of Civilians Weekly Report 28 February – 6 March 2007 Of note this week The IDF imposed a total closure on the West Bank during the Jewish holiday of Purim between 2 – 5 March. The closure prevented Palestinians, including workers, with valid permits, from accessing East Jerusalem and Israel during the four days. It is a year – the start of the 2006 Purim holiday – since Palestinian workers from the Gaza Strip have been prevented from accessing jobs in Israel. West Bank: − On 28 February, the IDF re-entered Nablus for one day to continue its largest scale operation for three years, codenamed ‘Hot Winter’. This second phase of the operation again saw a curfew imposed on the Old City, the occupation of schools and homes and house-to-house searches. The IDF also surrounded the three major hospitals in the area and checked all Palestinians entering and leaving. According to the Nablus Municipality 284 shops were damaged during the course of the operation. − Israeli Security Forces were on high alert in and around the Old city of Jerusalem in anticipation of further demonstrations and clashes following Friday Prayers at Al Aqsa mosque. Due to the Jewish holiday of Purim over the weekend, the Israeli authorities declared a blanket closure from Friday 2 March until the morning of Tuesday 6 March and all major roads leading to the Old City were blocked. -
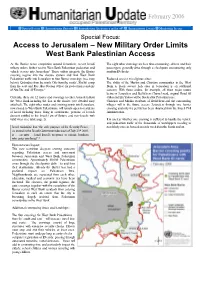
Access to Jerusalem – New Military Order Limits West Bank Palestinian Access
February 2006 Special Focus Humanitarian Reports Humanitarian Assistance in the oPt Humanitarian Events Monitoring Issues Special Focus: Access to Jerusalem – New Military Order Limits West Bank Palestinian Access As the Barrier nears completion around Jerusalem, recent Israeli The eight other crossings are less time-consuming - drivers and their military orders further restrict West Bank Palestinian pedestrian and passengers generally drive through a checkpoint encountering only vehicle access into Jerusalem.1 These orders integrate the Barrier random ID checks. crossing regime into the closure system and limit West Bank Palestinian traffic into Jerusalem to four Barrier crossings (see map Reduced access to religious sites: below): Qalandiya from the north, Gilo from the south2, Shu’fat camp The ability of the Muslim and Christian communities in the West from the east and Ras Abu Sbeitan (Olive) for pedestrian residents Bank to freely access holy sites in Jerusalem is an additional of Abu Dis, and Al ‘Eizariya.3 concern. With these orders, for example, all three major routes between Jerusalem and Bethlehem (Tunnel road, original Road 60 Currently, there are 12 routes and crossings to enter Jerusalem from (Gilo) and Ein Yalow) will be blocked for Palestinian use. the West Bank including the four in the Barrier (see detailed map Christian and Muslim residents of Bethlehem and the surrounding attached). The eight other routes and crossing points into Jerusalem, villages will in the future access Jerusalem through one barrier now closed to West Bank Palestinians, will remain open to residents crossing and only if a permit has been obtained from the Israeli Civil of Israel including those living in settlements, persons of Jewish Administration. -

The Palestinian Economy in East Jerusalem, Some Pertinent Aspects of Social Conditions Are Reviewed Below
UNITED N A TIONS CONFERENC E ON T RADE A ND D EVELOPMENT Enduring annexation, isolation and disintegration UNITED NATIONS CONFERENCE ON TRADE AND DEVELOPMENT Enduring annexation, isolation and disintegration New York and Geneva, 2013 Notes The designations employed and the presentation of the material do not imply the expression of any opinion on the part of the United Nations concerning the legal status of any country, territory, city or area, or of authorities or concerning the delimitation of its frontiers or boundaries. ______________________________________________________________________________ Symbols of United Nations documents are composed of capital letters combined with figures. Mention of such a symbol indicates a reference to a United Nations document. ______________________________________________________________________________ Material in this publication may be freely quoted or reprinted, but acknowledgement is requested, together with a copy of the publication containing the quotation or reprint to be sent to the UNCTAD secretariat: Palais des Nations, CH-1211 Geneva 10, Switzerland. ______________________________________________________________________________ The preparation of this report by the UNCTAD secretariat was led by Mr. Raja Khalidi (Division on Globalization and Development Strategies), with research contributions by the Assistance to the Palestinian People Unit and consultant Mr. Ibrahim Shikaki (Al-Quds University, Jerusalem), and statistical advice by Mr. Mustafa Khawaja (Palestinian Central Bureau of Statistics, Ramallah). ______________________________________________________________________________ Cover photo: Copyright 2007, Gugganij. Creative Commons, http://commons.wikimedia.org (accessed 11 March 2013). (Photo taken from the roof terrace of the Austrian Hospice of the Holy Family on Al-Wad Street in the Old City of Jerusalem, looking towards the south. In the foreground is the silver dome of the Armenian Catholic church “Our Lady of the Spasm”. -

Metropolitan Jerusalem - August 2006
Metropolitan Jerusalem - August 2006 Jalazun OFRA BET TALMON EL . RIMMONIM 60 Rd Bil'in Surda n llo Beitin Rammun A DOLEV Ramallah Deir Deir Ain DCO Dibwan Ibzi Al Chpt. Arik Ramallah Bireh G.ASSAF Beit Ur 80 Thta. Beituniya Burka 443 Beit Ur PSAGOT Fqa. MIGRON MA'ALE KOCHAV MIKHMAS BET YA'ACOV HORON Kufr Aqab Tira Rafat Mukhmas GIV'AT Kalandiya Beit Chpt. Liqya ZE'EV Beit Jaba GEVA Dukku BINYAMIN Jib Bir Ram Beit Nabala Inan Beit Ijza G.HAHADASHA B. N.YA'ACOV Qubeibe Hanina ALMON/ Bld. Beit Hizma ANATOT Biddu N.Samwil Hanina Qatanna Beit 45 HARADAR Beit P.ZE'EV Iksa Shuafat KFAR Surik ADUMIM RAMOT 1 R.SHLOMO Anata 1 FR. E 1 R.ESHKOL HILL Isawiya Zayim WEST East Jerusalem OLD Tur CITY I S R A E L Azarya MA'ALE Silwan ADUMIM Abu Thuri Dis Container Chpt. KEDAR Sawahra EAST Beit TALPIOT Safafa G. Sh.Sa'ad HAMATOS Sur GILO Walaja Bahir HAR HAR Battir GILO HOMA Ubaydiya Numan Mazmuriya Husan B.Jala Chpt. Wadi Al Kh.Juhzum 5 Km Fukin Bethlehem Khas Khadr B.Sahur BETAR ILLIT Um Shawawra NEVE Rukba Irtas Hindaza Nahhalin DANIEL GEVA'OT 60 Jaba ROSH TZURIM Za'atara Kht. EFRATA W.Rahhal BAT ELAZAR AYIN Zakarya Harmala ALLON W.an Nis SHVUT Jurat KFAR ELDAD Surif KFAR ash Shama TEKOA ETZION NOKDIM Tuku' Safa MIGDAL W e s t B a n k Beit OZ Beit Ummar Fajjar Map : © Jan de Jong Palestinian Village, Green Line Main Palestinian City or Road Link Neighborhood Jerusalem Israeli Settlement, Separation Israeli Checkpoint Existing / Barrier and/or Gate Under Construction Trajectory Israeli (Re) Constructed Israeli Civil or Military Israeli Municipal Settler Road, Facility and Area Limit East Jerusalem Projected or Under Construction E 1-Plan Outline Settlement Area Planned Settlement East of the Barrier 60 Road Number Construction . -

Draft Program
Under the high patronage of Mr François Hollande President of the French Republic Optimizing Euro-Palestinian Decentralised Cooperation www.dunkerqueplus10.org DRAFT PROGRAM Wednesday, November 27th 14.00 – 18.00 : Registration / Kursaal 19.00 : Welcoming cocktail reception / Greater Dunkirk Council Hall Dinner (not included) Thursday, November 28th /Morning / Kursaal of Dunkirk. 9.00 – 9.30 Registration 9.30 – 11.00 OPENING PLENARY CONFERENCE Speakers : Mahmoud Abbas, President of the Palestinian National Authority Michel Delebarre, Former Minister, Senator-Mayor of Dunkirk, Chairman of the Greater Dunkirk Council, Chairman of Cites Unies France. Marylise Lebranchu, Minister of Civil Service, State Reform and Decentralisation Claude Nicolet, Chairman of the French Network of Decentralized Cooperation Initiatives for Palestine (RCDP) Frode Mauring, Special Representative, United Nations Devlopment Program (UNDP), Palestine Isabelle Durant, Vice-president, European Parliament Leoluca Orlando, Mayor of Palermo, Member of the European Network of Local Authorities for Peace in the Middle East Anne Paugam, General manager of the French Development Agency Video message from Kadir Topbas, Mayor of Istanbul, Chairman of United Cities and Local Governments (UCLG) 2 11.00 – 13.15 PALESTINE: CONTEXT AND PERSPECTIVES Plenary session moderated by Bertrand Gallet, General manager of Cités Unies France Strategic challenge Pascal Boniface, Director of the Institute for International and Strategic Relations (IRIS) The humanitarian situation Ray Dolphin, -

A Survey of the Mental Health and the Psychosocial Support Organizations in the West Bank
The East Jerusalem YMCA Rehabilitation Program A Survey of the Mental Health and the Psychosocial Support organizations in the West Bank April 2014 The East Jerusalem YMCA Rehabilitation Program A Survey of the Mental Health and the Psychosocial Support organizations in the West Bank April 2014 By The East Jerusalem YMCA Rehabilitation Program 5 5 A Letter of Appreciation On my behalf and the behalf of the East Jerusalem YMCA - Rehabilitation Program administration, staff and volunteers I extend great thanks and appreciation to all the institutions that have collaborated and contributed to the completion of this important survey. This survey provides an excellent base for knowledge and facilitates the process of providing services, in addition to supplying an accurate informational background necessary for developing national plans. It also provides social protection services to our people, especially to children whose life, growth and future have been affected by the emergency incidents, caused primarily by the Israeli occupation of Palestine. The occupation’s oppressive actions that contradict with the international law and human values became a source of continuous danger, terror, anxiety and tension to the majority of our people especially the children. We thank and appreciate the efforts of the devoted people, especially our colleague Hussien Warasneh - The coordinator of the Training and Research Unit, who coordinated all of these efforts from the very beginning of our project until the completion of this study. We also thank the team of field workers, their supervisors, volunteers, staff and data entry clerks for their professionalism, eagerness, dedication and patience while collecting and validating the data, and then inputting it to the online database system. -
Development Assistance and the Occupied Palestinian Territories
House of Commons International Development Committee Development Assistance and the Occupied Palestinian Territories Fourth Report of Session 2006-07 Volume II Oral and written evidence Ordered by The House of Commons to be printed 24 January 2007 HC 114-II Published on 31 January 2007 by authority of the House of Commons London: The Stationery Office Limited £0.00 International Development Committee The International Development Committee is appointed by the House of Commons to examine the expenditure, administration, and policy of the Department for International Development and its associated public bodies. Current membership Malcolm Bruce MP (Liberal Democrat, Gordon) (Chairman) John Barrett MP (Liberal Democrat, Edinburgh West) John Battle MP (Labour, Leeds West) Hugh Bayley MP (Labour, City of York) John Bercow MP (Conservative, Buckingham) Richard Burden MP (Labour, Birmingham Northfield) Mr Quentin Davies MP (Conservative, Grantham and Stamford) James Duddridge MP (Conservative, Rochford and Southend East) Ann McKechin MP (Labour, Glasgow North) Joan Ruddock MP (Labour, Lewisham Deptford) Mr Marsha Singh MP (Labour, Bradford West) Powers The Committee is one of the departmental select committees, the powers of which are set out in House of Commons Standing Orders, principally in SO No 152. These are available on the Internet via www.parliament.uk. Publications The Reports and evidence of the Committee are published by The Stationery Office by Order of the House. All publications of the Committee (including press notices) are on the Internet at www.parliament.uk/indcom Committee staff The staff of the Committee are Carol Oxborough (Clerk), Matthew Hedges (Second Clerk), Anna Dickson (Committee Specialist), Chlöe Challender (Committee Specialist), Alex Paterson (Media Officer), Katie Phelan (Committee Assistant) and Jennifer Steele (Secretary). -

Al-Bireh Ramallah Salfit
Biddya Haris Kifl Haris Marda Tall al Khashaba Mas-ha Yasuf Yatma Sarta Dar Abu Basal Iskaka Qabalan Jurish 'Izbat Abu Adam Az Zawiya (Salfit) Talfit Salfit As Sawiya Qusra Majdal Bani Fadil Rafat (Salfit) Khirbet Susa Al Lubban ash Sharqiya Bruqin Farkha Qaryut Jalud Deir Ballut Kafr ad Dik Khirbet Qeis 'Ammuriya Khirbet Sarra Qarawat Bani Zeid (Bani Zeid al Gharb Duma Kafr 'Ein (Bani Zeid al Gharbi)Mazari' an Nubani (Bani Zeid qsh Shar Khirbet al Marajim 'Arura (Bani Zeid qsh Sharqiya) Turmus'ayya Al Lubban al Gharbi 'Abwein (Bani Zeid ash Sharqiya) Bani Zeid Deir as Sudan Sinjil Rantis Jilijliya 'Ajjul An Nabi Salih (Bani Zeid al Gharbi) Al Mughayyir (Ramallah) 'Abud Khirbet Abu Falah Umm Safa Deir Nidham Al Mazra'a ash Sharqiya 'Atara Deir Abu Mash'al Jibiya Kafr Malik 'Ein Samiya Shuqba Kobar Burham Silwad Qibya Beitillu Shabtin Yabrud Jammala Ein Siniya Bir Zeit Budrus Deir 'Ammar Silwad Camp Deir Jarir Abu Shukheidim Jifna Dura al Qar' Abu Qash At Tayba (Ramallah) Deir Qaddis Al Mazra'a al Qibliya Al Jalazun Camp 'Ein Yabrud Ni'lin Kharbatha Bani HarithRas Karkar Surda Al Janiya Al Midya Rammun Bil'in Kafr Ni'ma 'Ein Qiniya Beitin Badiw al Mus'arrajat Deir Ibzi' Deir Dibwan 'Ein 'Arik Saffa Ramallah Beit 'Ur at Tahta Khirbet Kafr Sheiyan Al-Bireh Burqa (Ramallah) Beituniya Al Am'ari Camp Beit Sira Kharbatha al Misbah Beit 'Ur al Fauqa Kafr 'Aqab Mikhmas Beit Liqya At Tira Rafat (Jerusalem) Qalandiya Camp Qalandiya Beit Duqqu Al Judeira Jaba' (Jerusalem) Al Jib Jaba' (Tajammu' Badawi) Beit 'Anan Bir Nabala Beit Ijza Ar Ram & Dahiyat al Bareed Deir al Qilt Kharayib Umm al Lahim QatannaAl Qubeiba Biddu An Nabi Samwil Beit Hanina Hizma Beit Hanina al Balad Beit Surik Beit Iksa Shu'fat 'Anata Shu'fat Camp Al Khan al Ahmar (Tajammu' Badawi) Al 'Isawiya. -

Greater Jerusalem” Has Jerusalem (Including the 1967 Rehavia Occupied and Annexed East Jerusalem) As Its Centre
4 B?63 B?466 ! np ! 4 B?43 m D"D" np Migron Beituniya B?457 Modi'in Bei!r Im'in Beit Sira IsraelRei'ut-proclaimed “GKharbrathae al Miasbah ter JerusaBeitl 'Uer al Famuqa ” D" Kochav Ya'akov West 'Ein as Sultan Mitzpe Danny Maccabim D" Kochav Ya'akov np Ma'ale Mikhmas A System of Settler-Colonialism and Apartheid Deir Quruntul Kochav Ya'akov East ! Kafr 'Aqab Kh. Bwerah Mikhmas ! Beit Horon Duyuk at Tahta B?443 'Ein ad D" Rafat Jericho 'Ajanjul ya At Tira np ya ! Beit Liq Qalandi Kochav Ya'akov South ! Lebanon Neve Erez ¥ ! Qalandiya Giv'at Ze'ev D" a i r Jaba' y 60 Beit Duqqu Al Judeira 60 B? a S Beit Nuba D" B? e Atarot Ind. Zone S Ar Ram Ma'ale Hagit Bir Nabala Geva Binyamin n Al Jib a Beit Nuba Beit 'Anan e ! Giv'on Hahadasha n a r Mevo Horon r Beit Ijza e t B?4 i 3 Dahiyat al Bareed np 6 Jaber d Aqbat e Neve Ya'akov 4 M Yalu B?2 Nitaf 4 !< ! ! Kharayib Umm al Lahim Qatanna Hizma Al Qubeiba ! An Nabi Samwil Ein Prat Biddu el Almon Har Shmu !< Beit Hanina al Balad Kfar Adummim ! Beit Hanina D" 436 Vered Jericho Nataf B? 20 B? gat Ze'ev D" Dayr! Ayyub Pis A 4 1 Tra Beit Surik B?37 !< in Beit Tuul dar ! Har A JLR Beit Iksa Mizpe Jericho !< kfar Adummim !< 21 Ma'ale HaHamisha B? 'Anata !< !< Jordan Shu'fat !< !< A1 Train Ramat Shlomo np Ramot Allon D" Shu'fat !< !< Neve Ilan E1 !< Egypt Abu Ghosh !< B?1 French Hill Mishor Adumim ! B?1 Beit Naqquba !< !< !< ! Beit Nekofa Mevaseret Zion Ramat Eshkol 1 Israeli Police HQ Mesilat Zion B? Al 'Isawiya Lifta a Qulunyia ! Ma'alot Dafna Sho'eva ! !< Motza Sheikh Jarrah !< Motza Illit Mishor Adummim Ind. -

Report on Mission Palestine
SJTN– Palestine Report Mission– May 2017 Report on mission to Palestine st - 1 to 4th May 2017 - “The world is too small for walls” – graffiti on Bethlehem’s “Apartheid wall” 1/42 SJTN– Palestine Report Mission– May 2017 2/42 SJTN– Palestine Report Mission– May 2017 Table of contents Acknowledgements ............................................................................................................................. 5 Introduction – Context of the mission ............................................................................................... 7 Mission to Palestine ............................................................................................................................. 8 Aims of the mission ........................................................................................................................... 8 Mission participants: ......................................................................................................................... 8 PART 1: BRIEF INTRODUCTION TO THE MUNICIPALITY OF AL-AZHARIYAH …........9 1.1.Location ........................................................................................................................................ 10 1.2.Description of Al-Azhariyah ....................................................................................................... 11 1.3.Municipality of Al-Azhariyah ..................................................................................................... 12 1.4.Challenges .................................................................................................................................... -

The Applied Research Institute – Jerusalem
Applied Research Institute ‐ Jerusalem (ARIJ) P.O Box 860, Caritas Street – Bethlehem, Phone: (+972) 2 2741889, Fax: (+972) 2 2776966. [email protected] | http://www.arij.org Applied Research Institute – Jerusalem Report on the Israeli Colonization Activities in the West Bank & the Gaza Strip Volume 157, August 2011 Issue http://www.arij.org Bethlehem • The Israeli occupation forces stormed Tqou’ town east of Bethlehem city and raided the houses of Jabril family and searched in its contents. Al Ayyam (August16, 2011). • The Israeli Bulldozers protected by the Israeli Army Forces razed 300 dunums of lands nearby the illegal Israeli outpost of Nevi Daniel North in attempt to expand it, which located 1.5 km north of the Nevi Dabiel settlement west of Al Khader town in the western parts of Bethlehem city. Palestine press News Agency (August16, 2011). • The Israeli settlers threw stones on the Abed Al Raham Shakarneh vehicles while passing through Khan Al Ahmar road between Jericho and Jerusalem caused damages to the cars of Adnan Mahmud Sobieh and Anwar Nasri Daʹdou from Al Khader town west of Bethlehem. Al Ayyam (August17, 2011). • The Israeli settlers threw stones and damaged Palestinian vehicle from Nahalin village west of Bethlehem city while passing near Beit ʹAyn settlement within what the Israeli call the Etzion settlements’ bloc southwest of Bethlehem city. The targeted vehicle owned by Abed Al Rahamn Shakarneh. Al Ayyam (August19, 2011). • The Israeli Occupation soldiers manning Al Container checkpoint closed the checkpoint in the face of Palestinians and started checking the IDs cards which caused obstructed the vehicular movements.