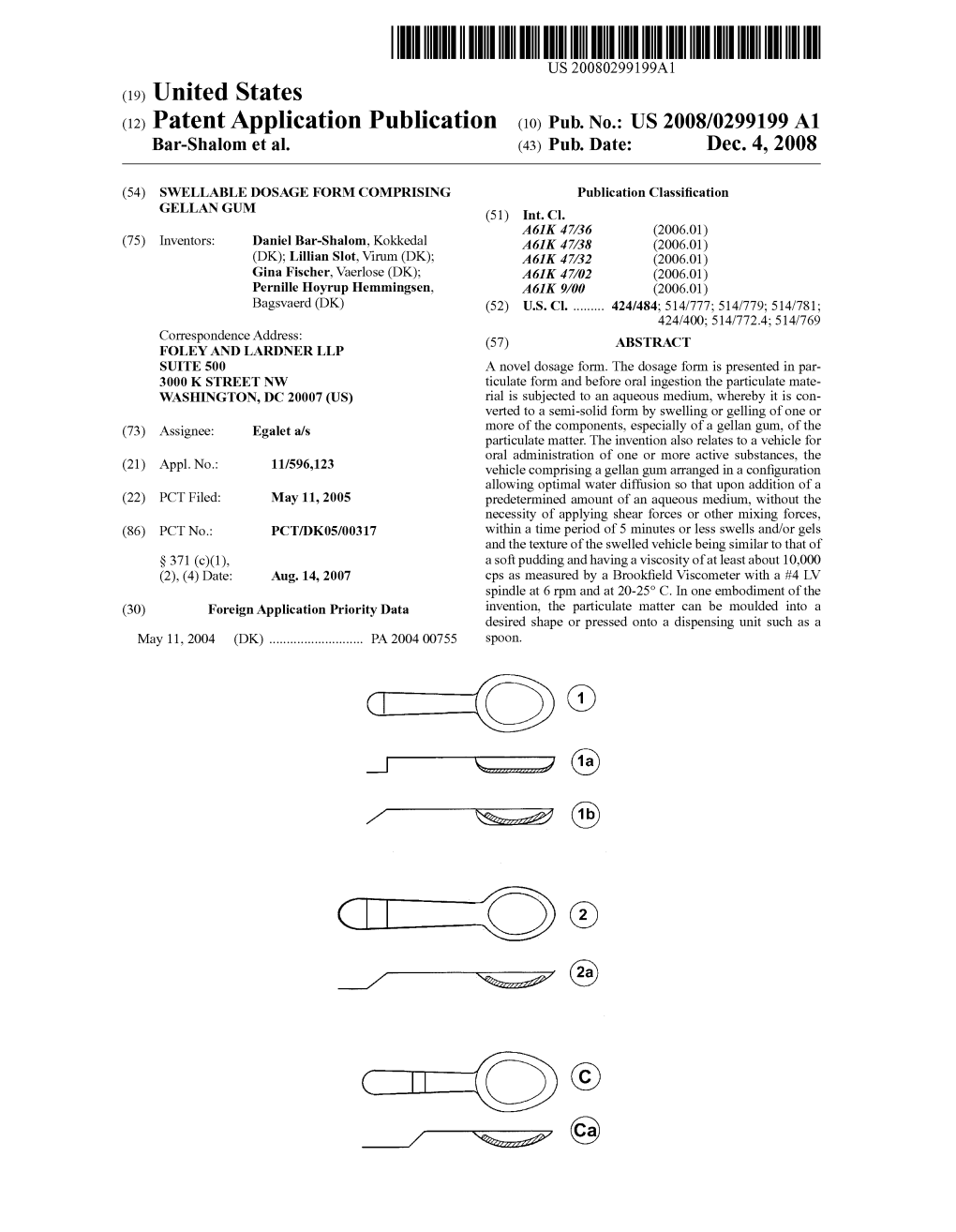
7 (1A) - N-27 (1B) Patent Application Publication Dec
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -

A Small Outbreak of Third Generation Cephem-Resistant Citrobacter
Jpn. J. Infect. Dis., 57, 2004 Laboratory and Epidemiology Communications A Small Outbreak of Third Generation Cephem-Resistant Citrobacter freundii Infection on a Surgical Ward Toshi Nada*, Hisashi Baba, Kumiko Kawamura2, Teruko Ohkura, Keizo Torii1 and Michio Ohta1 Department of Clinical Laboratory, Nagoya University Hospital, Nagoya 466-8560, 1Department of Bacteriology, Nagoya University Graduate School of Medicine, Nagoya 466-8550 and 2Department of Medical Technology, Nagoya University School of Health Sciences, Nagoya 461-8673 Communicated by Yoshichika Arakawa (Accepted June 11, 2004) Citrobacter freundii is a member of family Enterobacteri- from those of type a and b strains. aceae and has been associated with nosocomial infections As previous studies have indicated, third generation in the urinary, respiratory, and biliary tracts of debilitated cephem-resistance of Gram-negative bacteria are due to the hospital patients. C. freundii has an inducible chromosomally hydrolysis of β-lactams by β-lactamases. These β-lactamases encoded cephalosporinase that can inactivate cephamycins include extended spectrum β-lactamase (ESBL), metallo- and cephalosporins. However, most clinical isolates are β-lactamase, and plasmid-encoded AmpC cephalosporinase sensitive to new third generation cephems and carbapenems. (1-3). ESBL confers variable levels of resistance to cefotaxime, We report here a small outbreak of infection caused by ceftazidime, and other broad-spectrum cephalosporins and third generation cephem-resistant C. freundii on a surgical to monobactams, but has no detectable activity against ward of a university hospital in 2002. We identified four cephamycins and carbapenems, and is relatively sensitive patients with biliary infection and two carrier patients during to sulbactam (1). Plasmid-encoded metallo-β-lactamase July and October. -

Sepsis Caused by Newly Identified Capnocytophaga Canis Following Cat Bites: C
doi: 10.2169/internalmedicine.9196-17 Intern Med 57: 273-277, 2018 http://internmed.jp 【 CASE REPORT 】 Sepsis Caused by Newly Identified Capnocytophaga canis Following Cat Bites: C. canis Is the Third Candidate along with C. canimorsus and C. cynodegmi Causing Zoonotic Infection Minami Taki 1, Yoshio Shimojima 1, Ayako Nogami 2, Takuhiro Yoshida 1, Michio Suzuki 3, Koichi Imaoka 3, Hiroki Momoi 1 and Norinao Hanyu 1 Abstract: Sepsis caused by a Capnocytophaga canis infection has only been rarely reported. A 67-year-old female with a past medical history of splenectomy was admitted to our hospital with fever and general malaise. She had been bitten by a cat. She showed disseminated intravascular coagulation and multi-organ failure because of severe sepsis. On blood culture, characteristic gram-negative fusiform rods were detected; therefore, a Capnocytophaga species infection was suspected. A nucleotide sequence analysis revealed the species to be C. canis, which was newly identified in 2016. C. canis may have low virulence in humans; however, C. canis with oxidase activity may cause severe zoonotic infection. Key words: Capnocytophaga canis, Capnocytophaga canimorsus, sepsis, oxidase activity (Intern Med 57: 273-277, 2018) (DOI: 10.2169/internalmedicine.9196-17) Introduction Case Report The genus Capnocytophaga consists of gram-negative A 67-year-old woman was admitted to our hospital with rod-shaped bacteria that reside in the oral cavities of humans general malaise and fever for 3 days starting the day after and domestic animals. Capnocytophaga formerly comprised being bitten by a cat on both her hands. She had a medical eight species (1, 2). -
List of Union Reference Dates A
Active substance name (INN) EU DLP BfArM / BAH DLP yearly PSUR 6-month-PSUR yearly PSUR bis DLP (List of Union PSUR Submission Reference Dates and Frequency (List of Union Frequency of Reference Dates and submission of Periodic Frequency of submission of Safety Update Reports, Periodic Safety Update 30 Nov. 2012) Reports, 30 Nov. -

Product Information
ATROPINE INJECTION BP (Atropine sulfate monohydrate) 1. NAME OF THE MEDICINE Atropine sulfate monohydrate 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Atropine Injection BP is a sterile, isotonic, preservative free solution containing 600 microgram of atropine sulfate monohydrate in 1 mL or 1.2 mg of atropine sulfate monohydrate in 1 mL. 3. PHARMACEUTICAL FORM Solution for injection 4. CLINICAL PARTICULARS 4.1 Therapeutic Indications Preanaesthetic medication to reduce salivary secretions and bronchial secretions to prevent cholinergic cardiac effects such as cardiac arrhythmias, hypotension and bradycardia management of patients with acute myocardial infarction and sinus bradycardia who have associated hypotension and increased ventricular irritability concurrent administration with anticholinesterase agents (e.g. neostigmine, physostigmine) to block the adverse muscarinic effects of these agents following surgery to terminate curarisation for poisoning by organophosphate pesticides, atropine may be used concomitantly with a cholinesterase reactivator such as pralidoxime to reverse muscarinic effects. 4.2 Dose and Method of Administration Atropine Injection may be given by subcutaneous (SC), intramuscular (IM) or direct intravenous (IV) injection. Atropine Injection should not be added to any IV infusion solutions for administration. Atropine Injection contains no microbial agent. It should be used only once and any residue discarded. Cardiopulmonary resuscitation The usual adult dose is 0.4 - 1 mg IV, which may be repeated at 5 minute intervals until the desired heart rate is achieved. The total dose should not exceed 2 mg. Page 1 of 11 The usual paediatric dose is 0.02 mg/kg (maximum single dose 0.5 mg) IV, which may be repeated at 5 minute intervals until the desired heart rate is achieved. -

NINDS Custom Collection II
ACACETIN ACEBUTOLOL HYDROCHLORIDE ACECLIDINE HYDROCHLORIDE ACEMETACIN ACETAMINOPHEN ACETAMINOSALOL ACETANILIDE ACETARSOL ACETAZOLAMIDE ACETOHYDROXAMIC ACID ACETRIAZOIC ACID ACETYL TYROSINE ETHYL ESTER ACETYLCARNITINE ACETYLCHOLINE ACETYLCYSTEINE ACETYLGLUCOSAMINE ACETYLGLUTAMIC ACID ACETYL-L-LEUCINE ACETYLPHENYLALANINE ACETYLSEROTONIN ACETYLTRYPTOPHAN ACEXAMIC ACID ACIVICIN ACLACINOMYCIN A1 ACONITINE ACRIFLAVINIUM HYDROCHLORIDE ACRISORCIN ACTINONIN ACYCLOVIR ADENOSINE PHOSPHATE ADENOSINE ADRENALINE BITARTRATE AESCULIN AJMALINE AKLAVINE HYDROCHLORIDE ALANYL-dl-LEUCINE ALANYL-dl-PHENYLALANINE ALAPROCLATE ALBENDAZOLE ALBUTEROL ALEXIDINE HYDROCHLORIDE ALLANTOIN ALLOPURINOL ALMOTRIPTAN ALOIN ALPRENOLOL ALTRETAMINE ALVERINE CITRATE AMANTADINE HYDROCHLORIDE AMBROXOL HYDROCHLORIDE AMCINONIDE AMIKACIN SULFATE AMILORIDE HYDROCHLORIDE 3-AMINOBENZAMIDE gamma-AMINOBUTYRIC ACID AMINOCAPROIC ACID N- (2-AMINOETHYL)-4-CHLOROBENZAMIDE (RO-16-6491) AMINOGLUTETHIMIDE AMINOHIPPURIC ACID AMINOHYDROXYBUTYRIC ACID AMINOLEVULINIC ACID HYDROCHLORIDE AMINOPHENAZONE 3-AMINOPROPANESULPHONIC ACID AMINOPYRIDINE 9-AMINO-1,2,3,4-TETRAHYDROACRIDINE HYDROCHLORIDE AMINOTHIAZOLE AMIODARONE HYDROCHLORIDE AMIPRILOSE AMITRIPTYLINE HYDROCHLORIDE AMLODIPINE BESYLATE AMODIAQUINE DIHYDROCHLORIDE AMOXEPINE AMOXICILLIN AMPICILLIN SODIUM AMPROLIUM AMRINONE AMYGDALIN ANABASAMINE HYDROCHLORIDE ANABASINE HYDROCHLORIDE ANCITABINE HYDROCHLORIDE ANDROSTERONE SODIUM SULFATE ANIRACETAM ANISINDIONE ANISODAMINE ANISOMYCIN ANTAZOLINE PHOSPHATE ANTHRALIN ANTIMYCIN A (A1 shown) ANTIPYRINE APHYLLIC -

B-Lactams: Chemical Structure, Mode of Action and Mechanisms of Resistance
b-Lactams: chemical structure, mode of action and mechanisms of resistance Ru´ben Fernandes, Paula Amador and Cristina Prudeˆncio This synopsis summarizes the key chemical and bacteriological characteristics of b-lactams, penicillins, cephalosporins, carbanpenems, monobactams and others. Particular notice is given to first-generation to fifth-generation cephalosporins. This review also summarizes the main resistance mechanism to antibiotics, focusing particular attention to those conferring resistance to broad-spectrum cephalosporins by means of production of emerging cephalosporinases (extended-spectrum b-lactamases and AmpC b-lactamases), target alteration (penicillin-binding proteins from methicillin-resistant Staphylococcus aureus) and membrane transporters that pump b-lactams out of the bacterial cell. Keywords: b-lactams, chemical structure, mechanisms of resistance, mode of action Historical perspective Alexander Fleming first noticed the antibacterial nature of penicillin in 1928. When working with Antimicrobials must be understood as any kind of agent another bacteriological problem, Fleming observed with inhibitory or killing properties to a microorganism. a contaminated culture of Staphylococcus aureus with Antibiotic is a more restrictive term, which implies the the mold Penicillium notatum. Fleming remarkably saw natural source of the antimicrobial agent. Similarly, under- the potential of this unfortunate event. He dis- lying the term chemotherapeutic is the artificial origin of continued the work that he was dealing with and was an antimicrobial agent by chemical synthesis [1]. Initially, able to describe the compound around the mold antibiotics were considered as small molecular weight and isolates it. He named it penicillin and published organic molecules or metabolites used in response of his findings along with some applications of penicillin some microorganisms against others that inhabit the same [4]. -

Antibiotics and Antibacterials, General
B. Sulfamethoxydiazine (Sulfameter, Sulla) IX. TOXICITY AND SIDE EFFECTS: C. Sulfadimethoxine (Madribon) A. Fever D. Sulphormethoxine-Very long-acting; thera- B. Rash, urticaria peutic blood levels for 1 week. C. Cyanosis, methemoglobinemia D. Nausea, vomiting, diarrhea V. POORLY ABSORBED SULFONAMIDES: E. Hepatitis, jaundice for local use in the intestinal tract only. F. Hematuria, albuminuria, crystalluria, toxic A. Succinylsulfathiazole (Sulfasuxidine): nephritis. 1. Dosage-3.0 Gm q 4 h p.o. G. Headache, mental depression, psychosis, 2. Maximum effect usually not achieved un- peripheral neuritis. til 7th day of therapy. H. Leukopenia, agranulocytosis, purpura, aplas- B. Phthalylsulfathiazole (Sulfathalidine): tic anemia, hypoprothrombinemia, hemolytic ane- 1. Dosage-1.5 Gmq4hp.o. mia. 2. Double this dosage in the presence of I. Severe hypersensitivity reactions - anaphy- diarrhea. laxis, periarteritis nodosa and other collagen dis- 3. Effect produced in 5-7 days. eases, Stevens-Johnson syndrome. C. Para-nitrosulfathiazole (Nisulfazole): Used X. only for intrarectal instillation in treatment of PRECAUTIONS: proctitis or non-specific colitis. A. Keep careful record of urine output - try to maintain output of at least 1200-1500 ml/24 VI. TOPICAL SULFONAMIDES: hrs. B. Alkalinization of urine-sodium bicarbonate A. Mafenide (Sulfamylon): Used on skin as (12-15 Gm/day) may be used for this purpose 10% cream. Unlike other sulfonamides, effective when full systemic doses of sulfonamides are used, in presence of pus and necrotic tissue and does not when there is difficulty in being sure of adequate sensitize readily when used topically. Of value in fluid intake and output, and when such adjunctive prevention and therapy of burn infection due to therapy is not contraindicated. -

AMEG Categorisation of Antibiotics
12 December 2019 EMA/CVMP/CHMP/682198/2017 Committee for Medicinal Products for Veterinary use (CVMP) Committee for Medicinal Products for Human Use (CHMP) Categorisation of antibiotics in the European Union Answer to the request from the European Commission for updating the scientific advice on the impact on public health and animal health of the use of antibiotics in animals Agreed by the Antimicrobial Advice ad hoc Expert Group (AMEG) 29 October 2018 Adopted by the CVMP for release for consultation 24 January 2019 Adopted by the CHMP for release for consultation 31 January 2019 Start of public consultation 5 February 2019 End of consultation (deadline for comments) 30 April 2019 Agreed by the Antimicrobial Advice ad hoc Expert Group (AMEG) 19 November 2019 Adopted by the CVMP 5 December 2019 Adopted by the CHMP 12 December 2019 Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2020. Reproduction is authorised provided the source is acknowledged. Categorisation of antibiotics in the European Union Table of Contents 1. Summary assessment and recommendations .......................................... 3 2. Introduction ............................................................................................ 7 2.1. Background ........................................................................................................ -

(12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness Et Al
USOO6264,917B1 (12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness et al. (45) Date of Patent: Jul. 24, 2001 (54) TARGETED ULTRASOUND CONTRAST 5,733,572 3/1998 Unger et al.. AGENTS 5,780,010 7/1998 Lanza et al. 5,846,517 12/1998 Unger .................................. 424/9.52 (75) Inventors: Jo Klaveness; Pál Rongved; Dagfinn 5,849,727 12/1998 Porter et al. ......................... 514/156 Lovhaug, all of Oslo (NO) 5,910,300 6/1999 Tournier et al. .................... 424/9.34 FOREIGN PATENT DOCUMENTS (73) Assignee: Nycomed Imaging AS, Oslo (NO) 2 145 SOS 4/1994 (CA). (*) Notice: Subject to any disclaimer, the term of this 19 626 530 1/1998 (DE). patent is extended or adjusted under 35 O 727 225 8/1996 (EP). U.S.C. 154(b) by 0 days. WO91/15244 10/1991 (WO). WO 93/20802 10/1993 (WO). WO 94/07539 4/1994 (WO). (21) Appl. No.: 08/958,993 WO 94/28873 12/1994 (WO). WO 94/28874 12/1994 (WO). (22) Filed: Oct. 28, 1997 WO95/03356 2/1995 (WO). WO95/03357 2/1995 (WO). Related U.S. Application Data WO95/07072 3/1995 (WO). (60) Provisional application No. 60/049.264, filed on Jun. 7, WO95/15118 6/1995 (WO). 1997, provisional application No. 60/049,265, filed on Jun. WO 96/39149 12/1996 (WO). 7, 1997, and provisional application No. 60/049.268, filed WO 96/40277 12/1996 (WO). on Jun. 7, 1997. WO 96/40285 12/1996 (WO). (30) Foreign Application Priority Data WO 96/41647 12/1996 (WO). -

Effects of Protein Synthesis Inhibitors on the Lethal Action of Kanamycin and Streptomycin
222 THE JOURNAL OF ANTIBIOTICS, SER. A Nov. 1963 EFFECTS OF PROTEIN SYNTHESIS INHIBITORS ON THE LETHAL ACTION OF KANAMYCIN AND STREPTOMYCIN Hrnosm YA MAKI & NoBuo TAN AKA Institute of Applied Microbiology, University of Tokyo (Received for publication June 11, 1963) It was reported by ANAND and DAv1s 1l that chloramphenicol prevents killing of E.coli by streptomycin when the two antibiotics are added to the bacterial culture concomitantly. ANAND, DAvrs and ARMITAGE 2l demonstrated that chloramphenicol blocks accumulation of BC-streptomycin in bacteria. HuRwITz and RosANo 8l assumed the prerequisite of a strepto mycin-induced chloramphenicol-sensitive protein synthesis for the lethal action of strepto mycin. They•l also observed that chloramphenicol inhibits intrabacterial accumulation of BC-streptomycin and suggested that streptomycin-induced protein may be a specific transport system (permease). However, if the above assumption 1s correct, the induced protein synthesis appears not to be inhibited by streptomycin itself, although the antibiotic is known to interfere with protein synthesis under a certain conditions. W e5l are interested in the mode of action of kanamycin and like to know whether a similar phenomenon occurs with the lethal action of kanamycin. For the purpose of elucidating these problems, the effects of antibiotics, which inhibit bacterial protein synthesis, on the lethal action of kanamycin and streptomycin were studied and the results are presented in this publication. The antibiotics used include chloramphenicol, erythromycin, mikamycin A, puromycin, blasticidin S and tetracycline. The bactericidal action of both streptomycin and kanamycin was blocked by chloramphenicol, erythromycin, mikamycin A, blasticidin S and tetra cycline, but not by puromycin. -

EMA/CVMP/158366/2019 Committee for Medicinal Products for Veterinary Use
Ref. Ares(2019)6843167 - 05/11/2019 31 October 2019 EMA/CVMP/158366/2019 Committee for Medicinal Products for Veterinary Use Advice on implementing measures under Article 37(4) of Regulation (EU) 2019/6 on veterinary medicinal products – Criteria for the designation of antimicrobials to be reserved for treatment of certain infections in humans Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2019. Reproduction is authorised provided the source is acknowledged. Introduction On 6 February 2019, the European Commission sent a request to the European Medicines Agency (EMA) for a report on the criteria for the designation of antimicrobials to be reserved for the treatment of certain infections in humans in order to preserve the efficacy of those antimicrobials. The Agency was requested to provide a report by 31 October 2019 containing recommendations to the Commission as to which criteria should be used to determine those antimicrobials to be reserved for treatment of certain infections in humans (this is also referred to as ‘criteria for designating antimicrobials for human use’, ‘restricting antimicrobials to human use’, or ‘reserved for human use only’). The Committee for Medicinal Products for Veterinary Use (CVMP) formed an expert group to prepare the scientific report. The group was composed of seven experts selected from the European network of experts, on the basis of recommendations from the national competent authorities, one expert nominated from European Food Safety Authority (EFSA), one expert nominated by European Centre for Disease Prevention and Control (ECDC), one expert with expertise on human infectious diseases, and two Agency staff members with expertise on development of antimicrobial resistance .