Tl24 Minimum Reporting Level for Certain Diuretics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Optum Essential Health Benefits Enhanced Formulary PDL January
PENICILLINS ketorolac tromethamineQL GENERIC mefenamic acid amoxicillin/clavulanate potassium nabumetone amoxicillin/clavulanate potassium ER naproxen January 2016 ampicillin naproxen sodium ampicillin sodium naproxen sodium CR ESSENTIAL HEALTH BENEFITS ampicillin-sulbactam naproxen sodium ER ENHANCED PREFERRED DRUG LIST nafcillin sodium naproxen DR The Optum Preferred Drug List is a guide identifying oxacillin sodium oxaprozin preferred brand-name medicines within select penicillin G potassium piroxicam therapeutic categories. The Preferred Drug List may piperacillin sodium/ tazobactam sulindac not include all drugs covered by your prescription sodium tolmetin sodium drug benefit. Generic medicines are available within many of the therapeutic categories listed, in addition piperacillin sodium/tazobactam Fenoprofen Calcium sodium to categories not listed, and should be considered Meclofenamate Sodium piperacillin/tazobactam as the first line of prescribing. Tolmetin Sodium Amoxicillin/Clavulanate Potassium LOW COST GENERIC PREFERRED For benefit coverage or restrictions please check indomethacin your benefit plan document(s). This listing is revised Augmentin meloxicam periodically as new drugs and new prescribing LOW COST GENERIC naproxen kit information becomes available. It is recommended amoxicillin that you bring this list of medications when you or a dicloxacillin sodium CARDIOVASCULAR covered family member sees a physician or other penicillin v potassium ACE-INHIBITORS healthcare provider. GENERIC QUINOLONES captopril ANTI-INFECTIVES -

Eslicarbazepine Acetate Longer Procedure No
European Medicines Agency London, 19 February 2009 Doc. Ref.: EMEA/135697/2009 CHMP ASSESSMENT REPORT FOR authorised Exalief International Nonproprietary Name: eslicarbazepine acetate longer Procedure No. EMEA/H/C/000987 no Assessment Report as adopted by the CHMP with all information of a commercially confidential nature deleted. product Medicinal 7 Westferry Circus, Canary Wharf, London, E14 4HB, UK Tel. (44-20) 74 18 84 00 Fax (44-20) 74 18 84 16 E-mail: [email protected] http://www.emea.europa.eu TABLE OF CONTENTS 1. BACKGROUND INFORMATION ON THE PROCEDURE........................................... 3 1.1. Submission of the dossier ...................................................................................................... 3 1.2. Steps taken for the assessment of the product..................................................................... 3 2. SCIENTIFIC DISCUSSION................................................................................................. 4 2.1. Introduction............................................................................................................................ 4 2.2. Quality aspects ....................................................................................................................... 5 2.3. Non-clinical aspects................................................................................................................ 8 2.4. Clinical aspects.................................................................................................................... -

Pediatric Pharmacotherapy
Pediatric Pharmacotherapy A Monthly Review for Health Care Professionals of the Children's Medical Center Volume 1, Number 10, October 1995 DIURETICS IN CHILDREN • Overview • Loop Diuretics • Thiazide Diuretics • Metolazone • Potassium Sparing Diuretics • Diuretic Dosages • Efficacy of Diuretics in Chronic Pulmonary Disease • Summary • References Pharmacology Literature Reviews • Ibuprofen Overdosage • Predicting Creatinine Clearance Formulary Update Diuretics are used for a wide variety of conditions in infancy and childhood, including the management of pulmonary diseases such as respiratory distress syndrome (RDS) and bronchopulmonary dysplasia (BPD)(1 -5). Both RDS and BPD are often associated with underlying pulmonary edema and clinical improvement has been documented with diuretic use.6 Diuretics also play a major role in the management of congestive heart failure (CHF), which is frequently the result of congenital heart disease (7). Other indications, include hypertension due to the presence of cardiac or renal dysfunction. Hypertension in children is often resistant to therapy, requiring the use of multidrug regimens for optimal blood pressure control (8). Control of fluid and electrolyte status in the pediatric population remains a therapeutic challenge due to the profound effects of age and development on renal function. Although diuretics have been used extensively in infants and children, few controlled studies have been conducted to define the pharmacokinetics and pharmacodynamics of diuretics in this population. Nonetheless, diuretic therapy has become an important part of the management of critically ill infants and children. This issue will review the mechanisms of action, monitoring parameters, and indications for use of diuretics in the pediatric population (1-5). Loop Diuretics Loop diuretics are the most potent of the available diuretics (4). -

Primary Structure and Functional Expression of a Cdna Encoding the Thiazide-Sensitive, Electroneutral Sodium-Chloride Cotransporter GERARDO GAMBA*, SAMUEL N
Proc. Natl. Acad. Sci. USA Vol. 90, pp. 2749-2753, April 1993 Physiology Primary structure and functional expression of a cDNA encoding the thiazide-sensitive, electroneutral sodium-chloride cotransporter GERARDO GAMBA*, SAMUEL N. SALTZBERG*t, MICHAEL LOMBARDI*, AKIHIKO MIYANOSHITA*, JONATHAN LYTTON*, MATTHIAS A. HEDIGER*, BARRY M. BRENNER*, AND STEVEN C. HEBERT*t§ *Laboratory of Molecular Physiology and Biophysics, Renal Division, Department of Medicine, Brigham and Women's Hospital, Harvard Center for Study of Kidney Disease, Harvard Medical School, 75 Francis Street, Boston, MA 02115; and tMount Desert Island Biological Laboratory, Salsbury Cave, ME 04672 Communicated by Robert W. Berliner, December 17, 1992 ABSTRACT Electroneutral Na+:Cl- cotransport systems et al. (15) have identified a protein band of 185 kDa obtained are involved in a number of important physiological processes from membranes of rabbit renal cortex exposed to [3H]me- including salt absorption and secretion by epithelia and cell tolazone that may be a component of the thiazide-sensitive volume regulation. One group of Na+:Cl- cotransporters is Na+:Cl- cotransporter. specifically inhibited by the benzothiadiazine (thiazide) class of In this report we describe the sequence, functional and diuretic agents and can be distinguished from Na+:K+:2ClI pharmacological characterization, and tissue-specific expres- cotransporters based on a lack of K+ requirement and insen- sion of a cDNA clone (TSCil) encoding the electroneutral sitivity to sulfamoylbenzoic acid diuretics like bumetanide. We thiazide-sensitive Na+ :C1- cotransporter, isolated by a func- report here the isolation of a cDNA encoding a thiazide- tional expression strategy from the urinary bladder of the sensitive, electroneutral sodium-chloride cotransporter from euryhaline teleost P. -

Non-Steroidal Drug-Induced Glaucoma MR Razeghinejad Et Al 972
Eye (2011) 25, 971–980 & 2011 Macmillan Publishers Limited All rights reserved 0950-222X/11 www.nature.com/eye 1,2 1 1 Non-steroidal drug- MR Razeghinejad , MJ Pro and LJ Katz REVIEW induced glaucoma Abstract vision. The majority of drugs listed as contraindicated in glaucoma are concerned with Numerous systemically used drugs are CAG. These medications may incite an attack in involved in drug-induced glaucoma. Most those individuals with narrow iridocorneal reported cases of non-steroidal drug-induced angle.3 At least one-third of acute closed-angle glaucoma are closed-angle glaucoma (CAG). glaucoma (ACAG) cases are related to an Indeed, many routinely used drugs that have over-the-counter or prescription drug.1 Prevalence sympathomimetic or parasympatholytic of narrow angles in whites from the Framingham properties can cause pupillary block CAG in study was 3.8%. Narrow angles are more individuals with narrow iridocorneal angle. The resulting acute glaucoma occurs much common in the Asian population. A study of a more commonly unilaterally and only rarely Vietnamese population estimated a prevalence 4 bilaterally. CAG secondary to sulfa drugs is a of occludable angles at 8.5%. The reported bilateral non-pupillary block type and is due prevalence of elevated IOP months to years to forward movement of iris–lens diaphragm, after controlling ACAG with laser iridotomy 5,6 which occurs in individuals with narrow or ranges from 24 to 72%. Additionally, a open iridocorneal angle. A few agents, significant decrease in retinal nerve fiber layer including antineoplastics, may induce thickness and an increase in the cup/disc ratio open-angle glaucoma. -

Summary of Product Characteristics
Sandoz Business use only Page 1 of 9 1.3.1 spc-label-pl - common-spc – 11,006 20191218 (DE/H/1772/001-002-003 – 155347 - validation) TORASEMIDE 100 MG, 200 MG, 50 MG, TABLET 721-6534.01, 721-6535.01, 721-6536.01 SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT [Nationally completed name] 50 mg tablets [Nationally completed name] 100 mg tablets [Nationally completed name] 200 mg tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each tablet contains 50 mg of torasemide. Each tablet contains 100 mg of torasemide. Each tablet contains 200 mg of torasemide. For excipients, see section 6.1 3. PHARMACEUTICAL FORM Tablet. 50 mg tablets: White to off-white round tablet. 100 mg tablets: White to off-white round tablet with break notch. The tablet can be divided into equal doses. 200 mg tablets: White to off-white round tablet with cross break notch on both sides. The tablet can be divided into four equal doses. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications The administration of [Nationally completed name] 50 mg/- 100 mg/- 200 mg tablets is exclusively indicated in patients with highly reduced renal function (creatinine clearance less than 20 ml/min and/or serum creatinine concentration greater than 6 mg/dl). For maintenance of residual diuresis in case of severe renal insufficiency – even on dialysis if there is a considerable residual diuresis (more than 200 ml/24 hours) – if oedemas, effusions and/or hypertension exist. Note: [Nationally completed name] 50 mg/- 100 mg/- 200 mg tablets tablets are to be used only in case of highly impaired and not in normal renal function. -

Chapter 25 Mechanisms of Action of Antiepileptic Drugs
Chapter 25 Mechanisms of action of antiepileptic drugs GRAEME J. SILLS Department of Molecular and Clinical Pharmacology, University of Liverpool _________________________________________________________________________ Introduction The serendipitous discovery of the anticonvulsant properties of phenobarbital in 1912 marked the foundation of the modern pharmacotherapy of epilepsy. The subsequent 70 years saw the introduction of phenytoin, ethosuximide, carbamazepine, sodium valproate and a range of benzodiazepines. Collectively, these compounds have come to be regarded as the ‘established’ antiepileptic drugs (AEDs). A concerted period of development of drugs for epilepsy throughout the 1980s and 1990s has resulted (to date) in 16 new agents being licensed as add-on treatment for difficult-to-control adult and/or paediatric epilepsy, with some becoming available as monotherapy for newly diagnosed patients. Together, these have become known as the ‘modern’ AEDs. Throughout this period of unprecedented drug development, there have also been considerable advances in our understanding of how antiepileptic agents exert their effects at the cellular level. AEDs are neither preventive nor curative and are employed solely as a means of controlling symptoms (i.e. suppression of seizures). Recurrent seizure activity is the manifestation of an intermittent and excessive hyperexcitability of the nervous system and, while the pharmacological minutiae of currently marketed AEDs remain to be completely unravelled, these agents essentially redress the balance between neuronal excitation and inhibition. Three major classes of mechanism are recognised: modulation of voltage-gated ion channels; enhancement of gamma-aminobutyric acid (GABA)-mediated inhibitory neurotransmission; and attenuation of glutamate-mediated excitatory neurotransmission. The principal pharmacological targets of currently available AEDs are highlighted in Table 1 and discussed further below. -
Acetazolamide
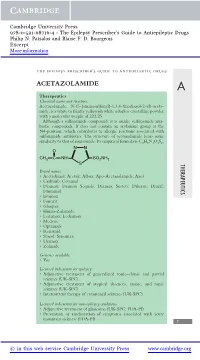
Cambridge University Press 978-0-521-68716-4 - The Epilepsy Prescriber’s Guide to Antiepileptic Drugs Philip N. Patsalos and Blaise F. D. Bourgeois Excerpt More information the epilepsy prescriber’s guide to antiepileptic drugs ACETAZOLAMIDE A Therapeutics Chemical name and structure: Acetazolamide, N-(5-(aminosulfonyl)-1,3,4-thiadiazol-2-yl)-aceta- mide, is a white to faintly yellowish white odorless crystalline powder with a molecular weight of 222.25. Although a sulfonamide compound, it is unlike sulfonamide anti- biotic compounds. It does not contain an arylamine group at the N4-position, which contributes to allergic reactions associated with sulfonamide antibiotics. The structure of acetazolamide bears some similarity to that of zonisamide. Its empirical formula is C4H6N4O3S2. NN O CH3 CNH SO2NH2 S THERAPEUTICS Brand names: r Acetadiazol; Acetak; Albox; Apo-Acetazolamide; Azol r Carbinib; Cetamid r Diamox; Diamox Sequals; Diamox Sustets; Diluran; Diural; Diuramid r Evamox r Fonurit r Glaupax r Huma-Zolamide r Ledamox; Lediamox r Medene r Optamide r Renamid r Stazol; Synomax r Uramox r Zolmide Generics available: r Yes Licensed indications for epilepsy: r Adjunctive treatment of generalized tonic–clonic and partial seizures (UK-SPC) r Adjunctive treatment of atypical absences, atonic, and tonic seizures (UK-SPC) r Intermittent therapy of catamenial seizures (UK-SPC) Licensed indications for non-epilepsy conditions: r Adjunctive treatment of glaucoma (UK-SPC; FDA-PI) r Prevention or amelioration of symptoms associated with acute mountain sickness (FDA-PI) 1 © in this web service Cambridge University Press www.cambridge.org Cambridge University Press 978-0-521-68716-4 - The Epilepsy Prescriber’s Guide to Antiepileptic Drugs Philip N. -

Southwest Journal of Pulmonary and Critical Care/2017/Volume 15 100 September 2017 Critical Care Case of the Month James T. Dean
September 2017 Critical Care Case of the Month James T. Dean III, MD Tyler R. Shackelford, DO Michel Boivin, MD Division of Pulmonary, Critical Care and Sleep Medicine University of New Mexico School of Medicine Albuquerque, NM USA A 73-year-old man presented with a three-day history of diffuse abdominal pain, decreased urine output, nausea and vomiting. His past medical history included diabetes, coronary artery disease, hypertension and chronic back pain. The patient reported being started on hydrochlorothiazide, furosemide, pregabalin and diclofenac within the last week in addition to his long-standing metformin prescription. Initial vitals were significant for tachypnea, tachycardia to 120 bpm, hypothermia to 35ºC and hypotension with a blood pressure of 70/40 mm Hg. Physical exam was remarkable for bilateral lung wheezing and significant respiratory distress. Laboratory examination was concerning for a pH of 6.85, pCO2 of < 5mmHg, serum lactate of 27mmol/l, WBC of 15.6 x106 cells/cc and a serum creatinine of 8.36 mg/dl. A chest X-ray showed evidence of mild pulmonary edema and a CT of the abdomen did not show any acute pathology. What is the most likely etiology of the patient’s severe acidosis? 1. Diabetic ketoacidosis 2. Ethylene glycol poisoning 3. Metformin-associated lactic acidosis 4. Septic shock Southwest Journal of Pulmonary and Critical Care/2017/Volume 15 100 Correct! 3. Metformin-associated lactic acidosis The most likely cause of the acidosis in this situation is metformin-induced lactic acidosis (1). The patient was intubated for respiratory failure secondary to severe non- compensated metabolic acidosis and shortly thereafter was started on maximal pressor support with norepinephrine, vasopressin, epinephrine and phenylephrine. -

The Bumetanide-Sensitive Na-K-2Cl Cotransporter NKCC1 As a Potential Target of a Novel Mechanism-Based Treatment Strategy for Neonatal Seizures
Neurosurg Focus 25 (3):E22, 2008 The bumetanide-sensitive Na-K-2Cl cotransporter NKCC1 as a potential target of a novel mechanism-based treatment strategy for neonatal seizures KRISTOPHER T. KAHLE, M.D., PH.D.,1 AND KEVIN J. STALEY, M.D.2 1Department of Neurosurgery and 2Division of Pediatric Neurology, Massachusetts General Hospital and Harvard Medical School, Boston, Massachusetts Seizures that occur during the neonatal period do so with a greater frequency than at any other age, have profound con- sequences for cognitive and motor development, and are difficult to treat with the existing series of antiepileptic drugs. During development, ␥-aminobutyric acid (GABA)ergic neurotransmission undergoes a switch from excitatory to – – inhibitory due to a reversal of neuronal chloride (Cl ) gradients. The intracellular level of chloride ([Cl ]i) in immature neonatal neurons, compared with mature adult neurons, is about 20-40 mM higher due to robust activity of the chlo- ride-importing Na-K-2Cl cotransporter NKCC1, such that the binding of GABA to ligand-gated GABAA receptor- associated Cl– channels triggers Cl– efflux and depolarizing excitation. In adults, NKCC1 expression decreases and the – expression of the genetically related chloride-extruding K-Cl cotransporter KCC2 increases, lowering [Cl ]i to a level – such that activation of GABAA receptors triggers Cl influx and inhibitory hyperpolarization. The excitatory action of GABA in neonates, while playing an important role in neuronal development and synaptogenesis, accounts for the decreased seizure threshold, increased seizure propensity, and poor efficacy of GABAergic anticonvulsants in this age group. Bumetanide, a furosemide-related diuretic already used to treat volume overload in neonates, is a specific inhibitor of NKCC1 at low doses, can switch the GABA equilibrium potential of immature neurons from depolarizing to hyperpolarizing, and has recently been shown to inhibit epileptic activity in vitro and in vivo in animal models of neonatal seizures. -

Diuretics in Clinical Practice. Part I: Mechanisms of Action, Pharmacological Effects and 1
Review Diuretics in clinical practice. Part I: mechanisms of action, pharmacological effects and 1. Introduction clinical indications of diuretic 2. Principles of diuretic action and classification of diuretic compounds compounds † 3. Carbonic anhydrase inhibitors Pantelis A Sarafidis , Panagiotis I Georgianos & Anastasios N Lasaridis Aristotle University of Thessaloniki, AHEPA Hospital, Section of Nephrology and Hypertension, 4. Osmotic diuretics 1st Department of Medicine, Thessaloniki, St. Kiriakidi 1, 54636, Thessaloniki, Greece 5. Loop diuretics 6. Thiazides and thiazide-related Importance of the field: Diuretics are among the most important drugs of our diuretics therapeutic armamentarium and have been broadly used for > 50 years, 7. Potassium-retaining diuretics providing important help towards the treatment of several diseases. Although all diuretics act primarily by impairing sodium reabsorption in the renal 8. Conclusion tubules, they differ in their mechanism and site of action and, therefore, in 9. Expert opinion their specific pharmacological properties and clinical indications. Loop diure- tics are mainly used for oedematous disorders (i.e., cardiac failure, nephrotic syndrome) and for blood pressure and volume control in renal disease; thiazides and related agents are among the most prescribed drugs for hypertension treatment; aldosterone-blockers are traditionally used for primary or secondary aldosteronism; and other diuretic classes have more specific indications. Areas covered in this review: This article discusses the mechanisms of action, pharmacological effects and clinical indications of the various diuretic classes For personal use only. used in everyday clinical practice, with emphasis on recent knowledge sug- gesting beneficial effects of certain diuretics on clinical conditions distinct from the traditional indications of these drugs (i.e., heart protection for aldosterone blockers). -

Topiramate Is More Effective Than Acetazolamide at Lowering
University of Birmingham Topiramate is more effective than acetazolamide at lowering intracranial pressure Scotton, William J; Botfield, Hannah F; Westgate, Connar Sj; Mitchell, James L; Yiangou, Andreas; Uldall, Maria S; Jensen, Rigmor H; Sinclair, Alex J DOI: 10.1177/0333102418776455 License: Creative Commons: Attribution (CC BY) Document Version Publisher's PDF, also known as Version of record Citation for published version (Harvard): Scotton, WJ, Botfield, HF, Westgate, CS, Mitchell, JL, Yiangou, A, Uldall, MS, Jensen, RH & Sinclair, AJ 2018, 'Topiramate is more effective than acetazolamide at lowering intracranial pressure', Cephalalgia. https://doi.org/10.1177/0333102418776455 Link to publication on Research at Birmingham portal Publisher Rights Statement: William J Scotton, Hannah F Botfield, Connar SJ Westgate, James L Mitchell, Andreas Yiangou, Maria S Uldall, Rigmor H Jensen, and Alex J Sinclair, Topiramate is more effective than acetazolamide at lowering intracranial pressure, Cephalalgia, First Published June 13, 2018; https://doi.org/10.1177/0333102418776455. Checked 02/07/2018. General rights Unless a licence is specified above, all rights (including copyright and moral rights) in this document are retained by the authors and/or the copyright holders. The express permission of the copyright holder must be obtained for any use of this material other than for purposes permitted by law. •Users may freely distribute the URL that is used to identify this publication. •Users may download and/or print one copy of the publication from the University of Birmingham research portal for the purpose of private study or non-commercial research. •User may use extracts from the document in line with the concept of ‘fair dealing’ under the Copyright, Designs and Patents Act 1988 (?) •Users may not further distribute the material nor use it for the purposes of commercial gain.