Nasogastric Intubation and Sengstaken-Blakemore Tube
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Letters to the Editor
letters to the Editor Porphyria, Cardiopulmonary Bypass, and heart with additional hemorrhage into the pericardial sac (5). Peri- cardiocentesis, however, can be a temporizing measure in the se- Volatile Anesthetics verely compromised patient (4,7,8) until definitive surgical estab- lishment of a pericardial window. A pericardial window can be To the Editor: established under local anesthesia (9) via the subxiphoid or lateral We take issue with Stevens et al’s contentious statements in their thoracotomy approach (1,2,5,8,9). The subxiphoid approach is less discussion of volatile anesthetics in the patient with acute intermit- useful for trauma because limited surgical exposure may preclude tent porphyria undergoing mitral valve replacement (1). repair of cardiac wounds (2). However, a pericardial window dur- In the “pre-propofol” era, the safe and appropriate use of halo- ing awake lateral thoracotomy may be both poorly tolerated and thane and isoflurane in porphyric patients was established (2). dangerous in the distressed, moving patient (7). Recent reports of the successful use of isoflurane in porphyric A blunt trauma victim (2) recently presented for an emergent patients undergoing cardiac surgery also exist (3,4). As the authors surgical pericardial window for recurrent acute pericardial tampon- themselves allude to a report of elevated porphyrins after propofol ade. Although the patient was not hypotensive, jugular venous anesthesia in acute intermittent porphyria, favoring propofol over distention, pulsus paradoxus (1,3,7), patient distress (4), and echo- inhaled anesthetics because of the latter’s implied lack of a “safety cardiographic signs were present. As an alternative to endotracheal record” cannot be supported. -

Incidence, Risk Factors and Management of Severe Post-Transsphenoidal Epistaxis Q ⇑ Kenneth M
Journal of Clinical Neuroscience 22 (2015) 116–122 Contents lists available at ScienceDirect Journal of Clinical Neuroscience journal homepage: www.elsevier.com/locate/jocn Clinical Study Incidence, risk factors and management of severe post-transsphenoidal epistaxis q ⇑ Kenneth M. De Los Reyes a, Bradley A. Gross a, , Kai U. Frerichs a, Ian F. Dunn a, Ning Lin a, Jordina Rincon-Torroella a, Donald J. Annino b, Edward R. Laws a a Department of Neurological Surgery, Brigham and Women’s Hospital and Harvard Medical School, 75 Francis Street, Boston, MA, 02115, USA b Department of Otolaryngology, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA, USA article info abstract Article history: Among the major complications of transsphenoidal surgery, less attention has been given to severe post- Received 16 June 2014 operative epistaxis, which can lead to devastating consequences. In this study, we reviewed 551 consec- Accepted 2 July 2014 utive patients treated over a 4 year period by the senior author to evaluate the incidence, risk factors, etiology and management of immediate and delayed post-transsphenoidal epistaxis. Eighteen patients (3.3%) developed significant postoperative epistaxis – six immediately and 12 delayed (mean postoper- Keywords: ative day 10.8). Fourteen patients harbored macroadenomas (78%) and 11 of 18 (61.1%) had complex Endoscopic nasal/sphenoid anatomy. In the immediate epistaxis group, 33% had acute postoperative hypertension. Epistaxis In the delayed group, one had an anterior ethmoidal pseudoaneurysm, and one had restarted anticoagu- Management Microscopic lation on postoperative day 3. We treated the immediate epistaxis group with bedside nasal packing fol- Pituitary lowed by operative re-exploration if conservative measures were unsuccessful. -

Treatment of Equine Gastric Impaction by Gastrotomy R
EQUINE VETERINARY EDUCATION / AE / april 2011 169 Case Reporteve_165 169..173 Treatment of equine gastric impaction by gastrotomy R. A. Parker*, E. D. Barr† and P. M. Dixon Dick Vet Equine Hospital, University of Edinburgh, Easter Bush Veterinary Centre, Midlothian; and †Bell Equine Veterinary Clinic, Mereworth, UK. Keywords: horse; colic; gastric impaction; gastrotomy Summary Edinburgh with a deep traumatic shoulder wound of 24 h duration. Examination showed a mildly contaminated, A 6-year-old Warmblood gelding was referred for treatment of 15 cm long wound over the cranial aspect of the left a traumatic shoulder wound and while hospitalised developed scapula that transected the brachiocephalicus muscle a large gastric impaction which was unresponsive to and extended to the jugular groove. The horse was sound medical management. Gastrotomy as a treatment for gastric at the walk and ultrasonography showed no abnormalities impactions is rarely attempted in adult horses due to the of the bicipital bursa. limited surgical access to the stomach. This report describes The wound was debrided and lavaged under standing the successful surgical treatment of the impaction by sedation and partially closed with 2 layers of 3 metric gastrotomy and management of the post operative polyglactin 910 (Vicryl)1 sutures in the musculature and complications encountered. simple interrupted polypropylene (Prolene)1 skin sutures, leaving some ventral wound drainage. Sodium benzyl Introduction penicillin/Crystapen)2 (6 g i.v. q. 8 h), gentamicin (Gentaject)3 (6.6 mg/kg bwt i.v. q. 24 h), flunixin 4 Gastric impactions are rare in horses but, when meglumine (Flunixin) (1.1 mg/kg bwt i.v. -

World Journal of Hepatology
World Journal of W J H Hepatology Submit a Manuscript: https://www.f6publishing.com World J Hepatol 2020 June 27; 12(6): 288-297 DOI: 10.4254/wjh.v12.i6.288 ISSN 1948-5182 (online) ORIGINAL ARTICLE Retrospective Cohort Study Hospital teaching status on the outcomes of patients with esophageal variceal bleeding in the United States Pavan Patel, Laura Rotundo, Evan Orosz, Faiz Afridi, Nikolaos Pyrsopoulos ORCID number: Pavan Patel Pavan Patel, Faiz Afridi, Nikolaos Pyrsopoulos, Division of Gastroenterology and Hepatology, (0000-0001-5682-4939); Laura Rutgers - New Jersey Medical School, Newark, NJ 07101-1709, United States Rotundo (0000-0002-4094-3682); Evan Orosz (0000-0003-2474-5501); Laura Rotundo, Evan Orosz, Department of Medicine, Rutgers - New Jersey Medical School, Faiz Afridi (0000-0002-0172-0486); Newark, NJ 07101-1709, United States Nikolaos Pyrsopoulos (0000-0002-6950-8174). Corresponding author: Nikolaos Pyrsopoulos, FACP, MD, PhD, Chief Doctor, Professor, Division of Gastroenterology and Hepatology, Rutgers – New Jersey Medical School, 185 S. Author contributions: Patel P Orange Avenue, MSB H-535, Newark, NJ 07101-1709, United States. provided conception and design of [email protected] the study, acquisition and analysis of data, and drafting of the manuscript; Rotundo L, Afridi F and Orosz E drafted the manuscript; Pyrsopoulos N Abstract contributed to the manuscript by BACKGROUND providing revision and oversight Acute variceal bleeding is a major complication of portal hypertension and is a of its writing. leading cause of death in patients with cirrhosis. There is limited data on the Institutional review board outcomes of patients with esophageal variceal bleeding in teaching versus statement: This study did not nonteaching hospitals. -

Femoral and Sciatic Nerve Blocks for Total Knee Replacement in an Obese Patient with a Previous History of Failed Endotracheal Intubation −A Case Report−
Anesth Pain Med 2011; 6: 270~274 ■Case Report■ Femoral and sciatic nerve blocks for total knee replacement in an obese patient with a previous history of failed endotracheal intubation −A case report− Department of Anesthesiology and Pain Medicine, School of Medicine, Catholic University of Daegu, Daegu, Korea Jong Hae Kim, Woon Seok Roh, Jin Yong Jung, Seok Young Song, Jung Eun Kim, and Baek Jin Kim Peripheral nerve block has frequently been used as an alternative are situations in which spinal or epidural anesthesia cannot be to epidural analgesia for postoperative pain control in patients conducted, such as coagulation disturbances, sepsis, local undergoing total knee replacement. However, there are few reports infection, immune deficiency, severe spinal deformity, severe demonstrating that the combination of femoral and sciatic nerve blocks (FSNBs) can provide adequate analgesia and muscle decompensated hypovolemia and shock. Moreover, factors relaxation during total knee replacement. We experienced a case associated with technically difficult neuraxial blocks influence of successful FSNBs for a total knee replacement in a 66 year-old the anesthesiologist’s decision to perform the procedure [1]. In female patient who had a previous cancelled surgery due to a failed tracheal intubation followed by a difficult mask ventilation for 50 these cases, peripheral nerve block can provide a good solution minutes, 3 days before these blocks. FSNBs were performed with for operations on a lower extremity. The combination of 50 ml of 1.5% mepivacaine because she had conditions precluding femoral and sciatic nerve blocks (FSNBs) has frequently been neuraxial blocks including a long distance from the skin to the used for postoperative pain control after total knee replacement epidural space related to a high body mass index and nonpalpable lumbar spinous processes. -

Most Common Robotic Bariatric Procedures: Review and Technical Aspects Pablo A
Acquafresca et al. Ann Surg Innov Res (2015) 9:9 DOI 10.1186/s13022-015-0019-9 REVIEW Open Access Most common robotic bariatric procedures: review and technical aspects Pablo A. Acquafresca1, Mariano Palermo1*, Tomasz Rogula2, Guillermo E. Duza1 and Edgardo Serra1 Abstract Since its appear in the year 1997, when Drs. Cadiere and Himpens did the first robotic cholecystectomy in Brus- sels, not long after the first cholecystectomy, they performed the first robotic bariatric procedure. It is believed that robotically-assisted surgery’s most notable contributions are reflected in its ability to extend the benefits of minimally invasive surgery to procedures not routinely performed using minimal access techniques. We describe the 3 most common bariatric procedures done by robot. The main advantages of the robotic system applied to the gastric bypass appear to be better control of stoma size, avoidance of stapler costs, elimination of the potential for oro- pharyngeal and esophageal trauma, and a potential decrease in wound infection. While in the sleeve gastrectomy and adjustable gastric banding its utility is more debatable, giving a bigger advantage during surgery on patients with a very large BMI or revisional cases. Keywords: Bariatric surgery, Robotic surgery, Gastric by pass, Sleeve gastrectomy, Gastric band Background laparoscopy and robotic laparoscopy is now a controver- Since its appear in the year 1997, when Drs. Cadiere and sial topic that concerns patients and surgeons alike. Himpens did the first robotic cholecystectomy in Brussels To date, the robotic technique is reported to be at least [1], the da Vinci™ Robotic Surgical System from Intuitive as safe and effective as the conventional approach for sev- Surgical, Inc., Sunny Vale, California (Fig. -
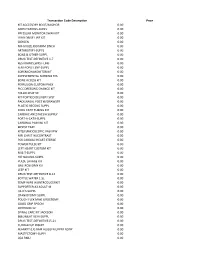
Transaction Code Description
Transaction Code Description Price KIT ACCESSORY BOOT/ANCHOR 0.00 AMPUTATIONS-SUPPL 0.00 PRESSURE MONITOR SWAN KIT 0.00 LVAD DRIVE LINE KIT 0.00 OXYGEN 0.00 NU-GAUZE,IODAFRM 1INCH 0.00 ARTHROTMY-SUPPL 0.00 BONE & OTHER-SUPPL 0.00 DRUG TEST-DEFINITIVE 1-7 0.00 RESTRAINTS,WRST-LMB 0.00 FEM-POPLIT.BYP-SUPPL 0.00 SORENSON MONITOR KIT 0.00 SUPPLEMENTAL NURSING SYS 0.00 BONE ACCESS KIT 0.00 PERFUSION CUSTOM PACK 0.00 PICC DRESSING CHANGE KIT 0.00 FOLLOLWUP 30 0.00 KIT PORTICO DELIVERY SYST 0.00 PACK,NASAL POST W/DRAWSTR 0.00 PLASTIC RECONS-SUPPL 0.00 COOL CATH TUBING KIT 0.00 CARDIAC ANESTHESIA SUPPLY 0.00 PORT-A-CATH-SUPPL 0.00 CARDINAL PAIN INJ KIT 0.00 BIOPSY TRAY 0.00 KIT(LF)ENDOSCOPIC VASVIEW 0.00 MRI CHEST W/CONTRAST 0.00 PCK CARDIAC HEART STERILE 0.00 POWER PULSE KIT 0.00 LEFT HEART CUSTOM KIT 0.00 M & T-SUPPL 0.00 HIP NAILING-SUPPL 0.00 PULSE LAVAGE KIT 0.00 GASTROSTOMY KIT 0.00 LEEP KIT 0.00 DRUG TEST-DEFINITIVE 8-14 0.00 BOTTLE WATER 1.5L 0.00 TEMP WIRE W/INTRODUCERKIT 0.00 SUPPORTER,A3 ADULT-M 0.00 I & D'S-SUPPL 0.00 CRANIOTOMY-SUPPL 0.00 POUCH FLEX MAXI UROSTOMY 0.00 GOOD GRIP SPOON 0.00 OXYHOOD 12- 0.00 SPINAL CARE KIT JACKSON 0.00 BI&UNILAT VEIN-SUPPL 0.00 DRUG TEST-DEFINITIVE15-21 0.00 CUDDLECUP INSERT 0.00 BLANKET (LF) BAIR HUGGER UPPER BODY 0.00 MASTECTOMY-SUPPL 0.00 LOA RMU 0.00 PACK LINQ 0.00 CHOLECYSTECTOM-SUPPL 0.00 RES BWL,SIG,AP-SUPPL 0.00 TRAY BIOPSY GENERAL UTIL 0.00 KIT(LF)CUSTOM SYRINGE ANGIO 0.00 OXISENSOR(LF)PEDI (PINK) 0.00 THORACIC SURG-SUPPL 0.00 NU-GAUZE PLAIN 1/2INCH 0.00 NU-GAUZE,IODAFRM 1/4INCH 0.00 PICC -

Journal of Clinical Toxicology Iwai Et Al., J Clin Toxicol 2014, 4:6 ISSN: 2161-0495 DOI: 10.4172/2161-0495.1000218
linica f C l To o x l ic a o n r l o u g o y J Journal of Clinical Toxicology Iwai et al., J Clin Toxicol 2014, 4:6 ISSN: 2161-0495 DOI: 10.4172/2161-0495.1000218 Case Report Open Access Utility of Upper Gastrointestinal Endoscopy for Management of Patients with Roundup® Poisoning Kenji Iwai1, Masato Miyauchi2, Daisuke Komazawa1, Ryoko Murao1, Hiroyuki Yokota2, and Atushi Koyama1 1Department of Emergency and Critical Care Medicine, Iwaki Kyoritu General Hospital, Fukushima, Japan 2Department of Emergency and Critical Care Medicine, Nippon Medical School, Tokyo, Japan *Corresponding author: Masato Miyauchi, Department of Emergency and Critical Care Medicine, Nippon Medical School, Tokyo, Japan, Tel: +81-3-3822-2131; E-mail: [email protected] Received date: Nov 03, 2014, Accepted date: Dec 05, 2014, Published date: Dec 08, 2014 Copyright: © 2014, Miyauchi M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Introduction: Roundup® is a herbicide widely used in Japan in gardening and agriculture. When ingested, Roundup is highly toxic, but gastrointestinal decontamination, including gastric lavage, is not routinely performed after ingestion. Endoscopy may be useful in managing individuals with liquid herbicide poisoning, by identifying gastric residual contents, assessing mucosal damage and retrieving herbicide directly by aspiration. Case report: A 73 year old, 40 kg female with a history of depression was transported to our emergency room by ambulance 1 h after attempting suicide by ingesting 100 ml Roundup, which contains 48% glyphosate-potassium, and 52% surfactant and water. -

Progressive Mandibular Midline Deviation After Difficult Tracheal
Anaesthesia 2013 doi:10.1111/anae.12271 Case Report Progressive mandibular midline deviation after difficult tracheal intubation J. Mareque Bueno,1,2 M. Fernandez-Barriales,3 M. A. Morey-Mas4,5 and F. Hernandez-Alfaro6,7 1 Associate Professor, 6 Professor, Department of Oral and Maxillofacial Surgery, Universitat Internacional de Catalunya, Barcelona, Spain 2 Staff, 3 Visiting Resident, 7 Director, Institute of Maxillofacial Surgery, Teknon Medical Center, Barcelona, Spain 4 Staff, Department of Oral and Maxillofacial Surgery, Hospital Son Dureta, Palma de Mallorca, Illes Balears, Spain 5 Associate Professor, Especialidad Universitaria en Implantologıa Oral, Universitat des Illes Balears, Illes Balears, Spain Summary We report condylar resorption of the temporomandibular joint after difficult intubation, leading to progressive midline mandibular deviation, subsequently treated by prosthetic joint replacement. ................................................................................................................................................................. Correspondence to: M. Fernandez-Barriales Email: [email protected] Accepted: 19 March 2013 Forces applied during difficult tracheal intubations can Following induction of anaesthesia and neuromus- cause oedema, bleeding, tracheal and oesophageal per- cular blockade, laryngoscopy with a Macintosh blade foration, pneumothorax or aspiration. Resorption of (size 3) permitted revealed a poor laryngeal view the temporomandibular joint has not been associated (Cormack-Lehane -

CPT Code Description Charge Amount 83498 17-Alpha
CPT Code Description Charge Amount 83498 17-alpha-Hydroxyprogester 308.41 83497 5-HIAA, SO 125.99 83516 A MYELOPEROX (MPO) AB QL 74.1 86021 AB ID LEUKOCYTE AB/SO 610.25 86022 AB ID, PLATELET ABS;SRA U 1318 86720 AB LEPTOSPIRA/SO 166.12 86850 AB SCREEN (IDC) 207.83 86850 AB SCREEN RBC EA SRM TECH 195.25 86793 AB, YERSINIA/SO 149 74018 ABDOMEN 1 VIEW 348.75 74018 ABDOMEN 1 VIEW PORTABLE 321.36 74022 ABDOMEN ACUTE COMP WSGL V 398.36 74019 ABDOMEN COMPLETE 398.36 74018 ABDOMEN SGL ANTEROPOSTERI 475.8 49083 ABDOMINAL PARACENTESIS W/ 1216.89 86870 ABID,WNJ 294.85 ABLATOR APOLLORF XL90 ASP 877.8 86900 ABO BLOOD TYPE 370 86900 ABO,BBSO 176.5 73050 AC JOINTS W/WO WEIGHTS BI 297.94 ACCUGRID RADIOGRAPH BREAS 121.36 82164 ACE, CSF SO 144.38 83519 ACHR BIND AB QT,RIA/SO MA 258 83519 ACHR BIND QNT MGP/SO 181.37 83519 ACHR BLOC QNT MGP/SO 181.37 83519 ACHR GANGL NEUR AB,RIA/SO 258 83519 ACHR MOD QNT MGP/SO 201.16 87116 ACID FAST CULTURE SO 227.33 83519 ACR BLOCKING QNT SO 181.37 83519 ACR RECEPTOR QNT SO 108.61 82024 ACTH,SO 459.3 86602 ACTINOMYCES AB/SO 64 85347 ACTIVATED CLOTTING TIME 126.93 85307 Activated Protein C Resis 216.04 97535GO ACTIVITY DAILY LIVING 15 265.91 78278 ACUTE GI BLOOD LOSS IMAGI 1326.15 82017 ACYLCARNITINES; QUANT, EA 574 85397 ADAMSTS 13 ACTIVITY/SO 796.62 ADAPTER CATH LUER 8.69 ADAPTER CONFIDENCE CEMENT 743.66 ADAPTER DLP PERFUS Y W/6 47.54 ADAPTER FIBEROPTIC SWIVEL 73.16 ADAPTER LUER LOC SHORT 3/ 2.2 ADAPTER LUER TO COLDER 15.29 ADAPTER MALE-MALE 4.57 C1776 ADAPTER PFC SIGMA FEMORAL 8474.76 ADAPTER PLUG MALE CLAVE 5.02 ADAPTER PRODIGY EXTENSION 2340 ADAPTER UROSTOMY DRAIN TU 9.09 ADAPTER VERSO AIRWAY ADUL 33.51 82952 ADDL GLUCOSE > 3 SPEC 136.24 87260 ADENOV/ RSPFAC / SO 141.75 ADHESIVE DEMABOND .07 PEN 193.48 ADHESIVE DEMABOND .07 PEN 193.48 ADHESIVE DERMABOND PEN 0. -

13. the Stomach & Duodenum
243 MEDICAL TREATMENT. 13 The stomach and No smoking, no alcohol, and frequent small meals may help the symptoms. Treatment with cimetidine 400mg bd duodenum or ranitidine 150mg bd for 4wks will cure 70% of duodenal ulcers. Extend this for 6wks for gastric ulcers, and 8wks for NSAID-induced ulcers. 13.1 Peptic ulcer Treating with Magnesium or Aluminium compounds in Indications for surgery on a peptic ulcer in the stomach or addition will reduce the absorption of anti-histamines and duodenum include: so is not logical. Dietary restrictions are unnecessary. (1) Closing a perforation. Bismuth compounds are often useful, as they ‘coat’ the (2).Performing a gastrojejunostomy or pyloroplasty if the mucosal surface, allowing it to heal. pylorus stenoses. (3).Stopping bleeding. If helicobacter is common (it usually is), a week’s course (4).Performing an elective truncal vagotomy and of ranitidine 400mg, amoxicillin 1g, and metronidazole pyloroplasty or gastrojejunostomy if there is a chronic 400mg bd will eradicate it in c.90% and may be worth disabling duodenal ulcer which has resisted medical administering ‘blind’. (Unfortunately, though, in some treatment. places, e.g. India, there may now be resistance to metronidazole.) Remember a breath or stool test may be Peptic ulcers are a common cause of epigastric pain in negative unless you stop proton-pump inhibitors 2wks most parts of the world. The underlying cause may well be beforehand! Helicobacter pylori. You will need to take a careful history to diagnose and manage peptic ulcer disease. For proven ulcers which recur after proper treatment with This can be difficult, so enquire how the patients cimetidine or ranitidine, it is worth trying proton-pump in your community express their ulcer symptoms. -

Chapter I GENERAL CORRECT CODING POLICIES for NATIONAL CORRECT CODING INITIATIVE POLICY MANUAL for MEDICARE SERVICES
CHAP1-gencorrectcodingpolicies Revision Date: 1/1/2021 Chapter I GENERAL CORRECT CODING POLICIES FOR NATIONAL CORRECT CODING INITIATIVE POLICY MANUAL FOR MEDICARE SERVICES Current Procedural Terminology (CPT) codes, descriptions and other data only are copyright 2020 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association. Applicable FARS\DFARS Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors, prospective payment systems, and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for the data contained or not contained herein. Revision Date (Medicare): 1/1/2021 Table of Contents LIST OF ACRONYMS ............................................ I-2 Chapter I ................................................... I-4 General Correct Coding Policies ............................ I-4 A. Introduction ..........................................I-4 B. Coding Based on Standards of Medical/Surgical Practice I-8 C. Medical/Surgical Package .............................I-11 D. Evaluation & Management (E&M) Services ...............I-16 E. Modifiers and Modifier Indicators ....................I-18 F. Standard Preparation/Monitoring Services for Anesthesia .................................................. I-26 G. Anesthesia Service Included in the Surgical Procedure I-26 H. HCPCS/CPT