Proper Logging of Podiatric Surgical Procedures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Practice Guideline for Limb Salvage Or Early Amputation
Limb Salvage or Early Amputation Evidence-Based Clinical Practice Guideline Adopted by: The American Academy of Orthopaedic Surgeons Board of Directors December 6, 2019 Endorsed by: Please cite this guideline as: American Academy of Orthopaedic Surgeons. Limb Salvage or Early Amputation Evidence-Based Clinical Practice Guideline. https://www.aaos.org/globalassets/quality-and-practice-resources/dod/ lsa-cpg-final-draft-12-10-19.pdf Published December 6, 2019 View background material via the LSA CPG eAppendix Disclaimer This clinical practice guideline was developed by a physician volunteer clinical practice guideline development group based on a formal systematic review of the available scientific and clinical information and accepted approaches to treatment and/or diagnosis. This clinical practice guideline is not intended to be a fixed protocol, as some patients may require more or less treatment or different means of diagnosis. Clinical patients may not necessarily be the same as those found in a clinical trial. Patient care and treatment should always be based on a clinician’s independent medical judgment, given the individual patient’s specific clinical circumstances. Disclosure Requirement In accordance with AAOS policy, all individuals whose names appear as authors or contributors to this clinical practice guideline filed a disclosure statement as part of the submission process. All panel members provided full disclosure of potential conflicts of interest prior to voting on the recommendations contained within this clinical practice guideline. Funding Source This clinical practice guideline was funded exclusively through a research grant provided by the United States Department of Defense with no funding from outside commercial sources to support the development of this document. -

Effectiveness of Distal Tibial Osteotomy
Nozaka et al. BMC Musculoskeletal Disorders (2020) 21:31 https://doi.org/10.1186/s12891-020-3061-7 RESEARCH ARTICLE Open Access Effectiveness of distal tibial osteotomy with distraction arthroplasty in varus ankle osteoarthritis Koji Nozaka* , Naohisa Miyakoshi, Takeshi Kashiwagura, Yuji Kasukawa, Hidetomo Saito, Hiroaki Kijima, Shuichi Chida, Hiroyuki Tsuchie and Yoichi Shimada Abstract Background: In highly active older individuals, end-stage ankle osteoarthritis has traditionally been treated using tibiotalar arthrodesis, which provides considerable pain relief. However, there is a loss of ankle joint movement and a risk of future arthrosis in the adjacent joints. Distraction arthroplasty is a simple method that allows joint cartilage repair; however, the results are currently mixed, with some reports showing improved pain scores and others showing no improvement. Distal tibial osteotomy (DTO) without fibular osteotomy is a type of joint preservation surgery that has garnered attention in recent years. However, to our knowledge, there are no reports on DTO with joint distraction using a circular external fixator. Therefore, the purpose of this study was to examine the effect of DTO with joint distraction using a circular external fixator for treating ankle osteoarthritis. Methods: A total of 21 patients with medial ankle arthritis were examined. Arthroscopic synovectomy and a microfracture procedure were performed, followed by angled osteotomy and correction of the distal tibia; the ankle joint was then stabilized after its condition improved. An external fixator was used in all patients, and joint distraction of approximately 5.8 mm was performed. All patients were allowed full weight-bearing walking immediately after surgery. Results: The anteroposterior and lateral mortise angle during weight-bearing, talar tilt angle, and anterior translation of the talus on ankle stress radiography were improved significantly (P < 0.05). -
Wound Classification
Wound Classification Presented by Dr. Karen Zulkowski, D.N.S., RN Montana State University Welcome! Thank you for joining this webinar about how to assess and measure a wound. 2 A Little About Myself… • Associate professor at Montana State University • Executive editor of the Journal of the World Council of Enterstomal Therapists (JWCET) and WCET International Ostomy Guidelines (2014) • Editorial board member of Ostomy Wound Management and Advances in Skin and Wound Care • Legal consultant • Former NPUAP board member 3 Today We Will Talk About • How to assess a wound • How to measure a wound Please make a note of your questions. Your Quality Improvement (QI) Specialists will follow up with you after this webinar to address them. 4 Assessing and Measuring Wounds • You completed a skin assessment and found a wound. • Now you need to determine what type of wound you found. • If it is a pressure ulcer, you need to determine the stage. 5 Assessing and Measuring Wounds This is important because— • Each type of wound has a different etiology. • Treatment may be very different. However— • Not all wounds are clear cut. • The cause may be multifactoral. 6 Types of Wounds • Vascular (arterial, venous, and mixed) • Neuropathic (diabetic) • Moisture-associated dermatitis • Skin tear • Pressure ulcer 7 Mixed Etiologies Many wounds have mixed etiologies. • There may be both venous and arterial insufficiency. • There may be diabetes and pressure characteristics. 8 Moisture-Associated Skin Damage • Also called perineal dermatitis, diaper rash, incontinence-associated dermatitis (often confused with pressure ulcers) • An inflammation of the skin in the perineal area, on and between the buttocks, into the skin folds, and down the inner thighs • Scaling of the skin with papule and vesicle formation: – These may open, with “weeping” of the skin, which exacerbates skin damage. -

Spider Silk for Tissue Engineering Applications
molecules Review Spider Silk for Tissue Engineering Applications Sahar Salehi 1, Kim Koeck 1 and Thomas Scheibel 1,2,3,4,5,* 1 Department for Biomaterials, University of Bayreuth, Prof.-Rüdiger-Bormann-Strasse 1, 95447 Bayreuth, Germany; [email protected] (S.S.); [email protected] (K.K.) 2 The Bayreuth Center for Colloids and Interfaces (BZKG), University of Bayreuth, Universitätsstraße 30, 95447 Bayreuth, Germany 3 The Bayreuth Center for Molecular Biosciences (BZMB), University of Bayreuth, Universitätsstraße 30, 95447 Bayreuth, Germany 4 The Bayreuth Materials Center (BayMAT), University of Bayreuth, Universitätsstraße 30, 95447 Bayreuth, Germany 5 Bavarian Polymer Institute (BPI), University of Bayreuth, Universitätsstraße 30, 95447 Bayreuth, Germany * Correspondence: [email protected]; Tel.: +49-0-921-55-6700 Received: 15 January 2020; Accepted: 6 February 2020; Published: 8 February 2020 Abstract: Due to its properties, such as biodegradability, low density, excellent biocompatibility and unique mechanics, spider silk has been used as a natural biomaterial for a myriad of applications. First clinical applications of spider silk as suture material go back to the 18th century. Nowadays, since natural production using spiders is limited due to problems with farming spiders, recombinant production of spider silk proteins seems to be the best way to produce material in sufficient quantities. The availability of recombinantly produced spider silk proteins, as well as their good processability has opened the path towards modern biomedical applications. Here, we highlight the research on spider silk-based materials in the field of tissue engineering and summarize various two-dimensional (2D) and three-dimensional (3D) scaffolds made of spider silk. -

The Whale Tendon Ligature
The Whale Tendon Ligature. By T. Ishiguko, M. D. Chief Surgeon of the- Imperial Japanese Army. The ligatures formerly in use iu tying vessels of the human body, were of different kinds to those of the present day. Silk and hemp ligatures were at one time applied by surgeons to such purpose, but as both had the defect of act- ing as foreign bodies in the animal oponomy, they were superseded by ligatures made of thin strips of leather. In support of the use of the leather, it was thought that ligatures of that materia would be decomposed by the heat aud moisture of the body, and that they would finally become absorbed; but numerous trials convinced those favorable to the use of leather ligatures that the idea was a fallacy : for leather, it was found, was far from being easily dissolved, and besides, it was very apt to break off at the time of its application. Dr. Lister’s ligature (cat-gut), though of comparatively recent origin, is held in such high estimation, that it is now almost exclusively used for tying vessels, or applying the suture to the viscera. It was in the year 1874 that I first saw its practical application in the operating theatre of the College, by Dr. Schultz, Instructor of Surgery to the Imperial Medical College, Tokio, which was possibly the first introduction and utilization of Lister’s ligature in Japan. My whale tendon ligature was invented a few years after. I first conceived the idea upon seeing, in the country, a whale tendon bow-string used in whip- ping cotton. -
Validation of a Clinical Prediction Rule for the Differentiation Between Septic Arthritis and Transient Synovitis of the Hip in Children by MININDER S
COPYRIGHT © 2004 BY THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED Validation of a Clinical Prediction Rule for the Differentiation Between Septic Arthritis and Transient Synovitis of the Hip in Children BY MININDER S. KOCHER, MD, MPH, RAHUL MANDIGA, BS, DAVID ZURAKOWSKI, PHD, CAROL BARNEWOLT, MD, AND JAMES R. KASSER, MD Investigation performed at the Departments of Orthopaedic Surgery, Biostatistics, and Radiology, Children’s Hospital, Boston, Massachusetts Background: The differentiation between septic arthritis and transient synovitis of the hip in children can be difficult. The purpose of the present study was to validate a previously published clinical prediction rule for this differentiation in a new patient population. Methods: We prospectively studied children who presented to a major children’s hospital between 1997 and 2002 with an acutely irritable hip. As in the previous study, diagnoses of septic arthritis (fifty-one patients) and transient synovitis (103 patients) were operationally defined on the basis of the white blood-cell count in the joint fluid, the re- sults of cultures of joint fluid and blood, and the clinical course. Univariate analysis and multiple logistic regression were used to compare the two groups. The predicted probability of septic arthritis of the hip from the prediction rule was compared with actual distributions in the current patient population. The area under the receiver operating char- acteristic curve was determined. Results: The same four independent predictors of septic arthritis of the hip (a history of fever, non-weight-bearing, an erythrocyte sedimentation rate of 40 mm/hr, and a serum white blood-cell count of >12,000 cells/mm3 (>12.0 × 109/L)) were identified in the current patient population. -

Techniques in Hand & Upper Extremity Surgery
Open Journal of Orthopedics, 2016, 6, 321-325 http://www.scirp.org/journal/ojo ISSN Online: 2164-3016 ISSN Print: 2164-3008 Techniques in Hand & Upper Extremity Surgery Anna De Leo, Billy Ching Leung*, Henk Giele Department of Plastic Surgery, John Radcliffe Hospital, Oxford University Hospital NHS Trust, Oxford, UK How to cite this paper: De Leo, A., Leung, Abstract B.C. and Giele, H. (2016) Techniques in Hand & Upper Extremity Surgery. Open The use of tendon transfer to restore functions of extremities was initially recognised Journal of Orthopedics, 6, 321-325. in the 19th century, and its advancement was further amplified by the polio epidemic http://dx.doi.org/10.4236/ojo.2016.610042 towards the turn of that century. Tendon transfer surgery extended to the use for Received: August 18, 2016 traumatic reconstructive surgery during World War I, with key surgical pioneers, in- Accepted: October 16, 2016 cluding Mayer, Sterling Bunnell, Guy Pulvertaft and Joseph Boyes. In 1921, Robert Published: October 19, 2016 Jones first described the transfer of pronator teres (PT) to the wrist extensors for ir- reparable radial nerve paralysis in infantile hemiplegia. Although, a detailed descrip- Copyright © 2016 by authors and Scientific Research Publishing Inc. tion of its indication and surgical outcomes were not published until 1959 and 1970 This work is licensed under the Creative by Stelling and Meyer, and Keats, respectively. Pronator teres is often the tendon of Commons Attribution International choice for reconstructing wrist extensors, and used in a multiple of pathologies, in- License (CC BY 4.0). cluding radial nerve palsy, cerebral palsy, and tetraplegia. -

ICD~10~PCS Complete Code Set Procedural Coding System Sample
ICD~10~PCS Complete Code Set Procedural Coding System Sample Table.of.Contents Preface....................................................................................00 Mouth and Throat ............................................................................. 00 Introducton...........................................................................00 Gastrointestinal System .................................................................. 00 Hepatobiliary System and Pancreas ........................................... 00 What is ICD-10-PCS? ........................................................................ 00 Endocrine System ............................................................................. 00 ICD-10-PCS Code Structure ........................................................... 00 Skin and Breast .................................................................................. 00 ICD-10-PCS Design ........................................................................... 00 Subcutaneous Tissue and Fascia ................................................. 00 ICD-10-PCS Additional Characteristics ...................................... 00 Muscles ................................................................................................. 00 ICD-10-PCS Applications ................................................................ 00 Tendons ................................................................................................ 00 Understandng.Root.Operatons..........................................00 -
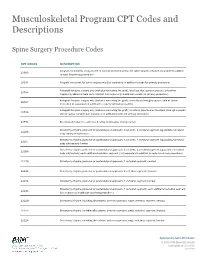
Musculoskeletal Program CPT Codes and Descriptions
Musculoskeletal Program CPT Codes and Descriptions Spine Surgery Procedure Codes CPT CODES DESCRIPTION Allograft, morselized, or placement of osteopromotive material, for spine surgery only (List separately in addition 20930 to code for primary procedure) 20931 Allograft, structural, for spine surgery only (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); local (eg, ribs, spinous process, or laminar 20936 fragments) obtained from same incision (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); morselized (through separate skin or fascial 20937 incision) (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); structural, bicortical or tricortical (through separate 20938 skin or fascial incision) (List separately in addition to code for primary procedure) 20974 Electrical stimulation to aid bone healing; noninvasive (nonoperative) Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22206 body subtraction); thoracic Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22207 body subtraction); lumbar Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22208 body subtraction); each additional vertebral segment (List separately in addition to code for -

Priority Health Spine and Joint Code List
Priority Health Joint Services Code List Category CPT® Code CPT® Code Description Joint Services 23000 Removal of subdeltoid calcareous deposits, open Joint Services 23020 Capsular contracture release (eg, Sever type procedure) Joint Services 23120 Claviculectomy; partial Joint Services 23130 Acromioplasty or acromionectomy, partial, with or without coracoacromial ligament release Joint Services 23410 Repair of ruptured musculotendinous cuff (eg, rotator cuff) open; acute Joint Services 23412 Repair of ruptured musculotendinous cuff (eg, rotator cuff) open;chronic Joint Services 23415 Coracoacromial ligament release, with or without acromioplasty Joint Services 23420 Reconstruction of complete shoulder (rotator) cuff avulsion, chronic (includes acromioplasty) Joint Services 23430 Tenodesis of long tendon of biceps Joint Services 23440 Resection or transplantation of long tendon of biceps Joint Services 23450 Capsulorrhaphy, anterior; Putti-Platt procedure or Magnuson type operation Joint Services 23455 Capsulorrhaphy, anterior;with labral repair (eg, Bankart procedure) Joint Services 23460 Capsulorrhaphy, anterior, any type; with bone block Joint Services 23462 Capsulorrhaphy, anterior, any type;with coracoid process transfer Joint Services 23465 Capsulorrhaphy, glenohumeral joint, posterior, with or without bone block Joint Services 23466 Capsulorrhaphy, glenohumeral joint, any type multi-directional instability Joint Services 23470 ARTHROPLASTY, GLENOHUMERAL JOINT; HEMIARTHROPLASTY ARTHROPLASTY, GLENOHUMERAL JOINT; TOTAL SHOULDER [GLENOID -

Knee Joint Surgery: Open Synovectomy
Musculoskeletal Surgical Services: Open Surgical Procedures; Knee Joint Surgery: Open Synovectomy POLICY INITIATED: 06/30/2019 MOST RECENT REVIEW: 06/30/2019 POLICY # HH-5588 Overview Statement The purpose of these clinical guidelines is to assist healthcare professionals in selecting the medical service that may be appropriate and supported by evidence to improve patient outcomes. These clinical guidelines neither preempt clinical judgment of trained professionals nor advise anyone on how to practice medicine. The healthcare professionals are responsible for all clinical decisions based on their assessment. These clinical guidelines do not provide authorization, certification, explanation of benefits, or guarantee of payment, nor do they substitute for, or constitute, medical advice. Federal and State law, as well as member benefit contract language, including definitions and specific contract provisions/exclusions, take precedence over clinical guidelines and must be considered first when determining eligibility for coverage. All final determinations on coverage and payment are the responsibility of the health plan. Nothing contained within this document can be interpreted to mean otherwise. Medical information is constantly evolving, and HealthHelp reserves the right to review and update these clinical guidelines periodically. No part of this publication may be reproduced, stored in a retrieval system or transmitted, in any form or by any means, electronic, mechanical, photocopying, or otherwise, without permission from HealthHelp. -

Realignment Surgery As Alternative Treatment of Varus and Valgus Ankle Osteoarthritis
CLINICAL ORTHOPAEDICS AND RELATED RESEARCH Number 462, pp. 156–168 © 2007 Lippincott Williams & Wilkins Realignment Surgery as Alternative Treatment of Varus and Valgus Ankle Osteoarthritis Geert I. Pagenstert, MD*; Beat Hintermann, MD*; Alexej Barg, MD*; André Leumann, MD†; and Victor Valderrabano, MD, PhD† In patients with asymmetric (varus or valgus) ankle osteo- Level of Evidence: Level IV, therapeutic study. See the arthritis, realignment surgery is an alternative treatment to Guidelines for Authors for a complete description of levels of fusion or total ankle replacement in selected cases. To deter- evidence. mine whether realignment surgery in asymmetric ankle os- teoarthritis relieved pain and improved function, we clini- cally and radiographically followed 35 consecutive patients Surgical treatment for patients with symptomatic ankle with posttraumatic ankle osteoarthritis treated with lower osteoarthritis (OA) is controversial, particularly in me- leg and hindfoot realignment surgery. We further questioned if outcome correlated with achieved alignment. The average chanically induced, malaligned ankle OA in which joint patient age was 43 years (range, 26–68 years). We used a cartilage is partially preserved. These patients typically are standardized clinical and radiographic protocol. Besides dis- in their economically important, active middle ages be- tal tibial osteotomies, additional bony and soft tissue proce- cause early trauma is the predominant (70–80%) etiology dures were performed in 32 patients (91%). At mean fol- of their ankle OA.49,58 Currently, treatment recommenda- lowup of 5 years (range, 3–10.5 years), pain decreased by an tions after failed nonoperative therapy are polarized be- average of 4 points on a visual analog scale; range of ankle tween fusion2,11,33 and total ankle replacement motion increased by an average of 5°.