A Typical Presentation of Hepatocellular Carcinoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Etiology of Upper Gastrointestinal Haemorrhage in a Teaching Hospital
TAJ June 2008; Volume 21 Number 1 ISSN 1019-8555 The Journal of Teachers Association RMC, Rajshahi Original Article Etiology of Upper Gastrointestinal Haemorrhage in a Teaching Hospital M Uddin Ahmed1, M Abdul Ahad2, M A Alim2, A R M Saifuddin Ekram3, Q Abdullah Al Masum4, Sumona Tanu5, Refaz Uddin6 Abstract A descriptive study on all cases of haematemesis and or melaena was carried out at Rajshahi Medical College Hospital to observe the demographic profile, clinical presentation, cause and outcome of upper gastrointestinal bleeding in a tertiary hospital of Bangladesh. Fifty adult patients presenting with haematemesis and or melaena admitted consecutively into medical unit were evaluated through proper history taking, thorough clinical examination, endoscopic examination with in 48 hours of first presentation and other related investigations. Patients those who were not stabilized haemodynamically with in 48 hours of resuscitation and endoscopy could not be done with in that period were excluded from this study. Results our results showed that out of 50 patients 44 were male and 6 were female and average age of the patients was 39.9 years. Most of the patients were from low socio-economic condition. Farmers, service holders and laborers were the most (57%) affected group. Haematemesis and melaena (42%), only melaena (42%) and only haematemesis (16%) were the presenting features. Endoscopy revealed that duodenal ulcer( 34%) was the most common cause of UGI bleeding followed by rupture of portal varices( 16%) , neoplasm( 10%) , gastric ulcer ( 08%) and gastric erosion( 06%). Acute upper GI bleeding is a common medical problem that is responsible for significant morbidity and mortality. -

Obscure Gastrointestinal Bleeding in Cirrhosis: Work-Up and Management
Current Hepatology Reports (2019) 18:81–86 https://doi.org/10.1007/s11901-019-00452-6 MANAGEMENT OF CIRRHOTIC PATIENT (A CARDENAS AND P TANDON, SECTION EDITORS) Obscure Gastrointestinal Bleeding in Cirrhosis: Work-up and Management Sergio Zepeda-Gómez1 & Brendan Halloran1 Published online: 12 February 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose of Review Obscure gastrointestinal bleeding (OGIB) in patients with cirrhosis can be a diagnostic and therapeutic challenge. Recent advances in the approach and management of this group of patients can help to identify the source of bleeding. While the work-up of patients with cirrhosis and OGIB is the same as with patients without cirrhosis, clinicians must be aware that there are conditions exclusive for patients with portal hypertension that can potentially cause OGIB. Recent Findings New endoscopic and imaging techniques are capable to identify sources of OGIB. Balloon-assisted enteroscopy (BAE) allows direct examination of the small-bowel mucosa and deliver specific endoscopic therapy. Conditions such as ectopic varices and portal hypertensive enteropathy are better characterized with the improvement in visualization by these techniques. New algorithms in the approach and management of these patients have been proposed. Summary There are new strategies for the approach and management of patients with cirrhosis and OGIB due to new develop- ments in endoscopic techniques for direct visualization of the small bowel along with the capability of endoscopic treatment for different types of lesions. Patients with cirrhosis may present with OGIB secondary to conditions associated with portal hypertension. Keywords Obscure gastrointestinal bleeding . Cirrhosis . Portal hypertension . -
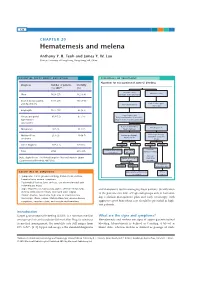
Hematemesis and Melena Chapter
126 CHAPTER 20 Hematemesis and melena Anthony Y. B. Teoh and James Y. W. Lau Chinese University of Hong Kong, Hong Kong SAR, China ESSENTIAL FACTS ABOUT CAUSATION ESSENTIALS OF TREATMENT Algorithm for management of acute GI bleeding Diagnosis Number of patients Mortality (%) 200716 (%) Major bleeding Minor bleeding Ulcer 1826 (27) 162 (8.9) (unstable hemodynamics) Erosive disease (gastric 1731 (26) 195 (14.1) Early elective upper and duodenum) Active resuscitation endoscopy Esophagitis 1177 (17) 65 (5.5) Urgent endoscopy Varices and portal 819 (12) 87 (14) Early administration of vasoactive hypertensive drugs in suspected variceal bleeding gastropathy Active ulcer bleeding Bleeding varices Malignancy 187 (3) 31 (17) Major stigmata Mallory-Weiss 213 (3) 10 (4.7) Endoscopic therapy Endoscopic therapy Adjunctive PPI Adjunctive vasoactive syndrome drugs Other diagnosis 797 (12) 125 (16) Success Failure Success Failure Continue Continue ulcer healing Recurrent Total 6750 675 (10) vasoactive drugs medications bleeding Variceal Data adapted from The United Kingdom National Audit in Upper Repeat endoscopic eradication Gastrointestinal Bleeding 2007 [16]. therapy program Sengstaken- Success Failure Blakemore tube ESSENTIALS OF DIAGNOSIS Angiographic embolization TIPS vs vs. surgery surgery • Symptoms: Coffee ground vomiting, hematemesis, melena, hematochezia, anemic symptoms • Past medical history: Liver cirrhosis, use of non-steroidal anti- inflammatory drugs • Signs: Hypotension, tachycardia, pallor, altered mental status, and therapeutic tool in managing these patients. Stratification melena or blood per rectum, decreased urine output of the patients into low- or high-risk groups aids in formulat- • Bloods: Anemia, raised urea, high urea to creatinine ratio • Endoscopy: Ulcers, varices, Mallory-Weiss tear, erosive disease, ing a clinical management plan and early endoscopy with neoplasms, vascular ectasia, and vascular malformations aggressive post-hemostasis care should be provided in high- risk patients. -

Hematemesis Melena Due to Helicobacter Pylori Infection in Duodenal Ulcer: a Case Report and Literature Review
International Journal of Science and Research (IJSR) ISSN (Online): 2319-7064 Index Copernicus Value (2016): 79.57 | Impact Factor (2017): 7.296 Hematemesis Melena due to Helicobacter Pylori Infection In Duodenal Ulcer: A Case Report and Literature Review Ayu Budhi Trisna Dewi Rahayu Sutanto1, I Made Suma Wirawan2 1General Practitioner Wangaya Hospital Denpasar Bali Indonesia 2 Endoscopy Unit of Internal Medicine Wangaya Hospital Denpasar Bali Indoensia Abstract: A Balinese woman, 60 years old complaint of hematemesis and melena. Esophagogastroduodenoscopy performed one day after admission and revealed a soliter ulcer at duodenum bulb. Histopathology examination revealed a spherical like organism suspected Helicobacter pylori (H. pylori) infection. Eradication of H. pylori by triple drug consisting of omeprazole, amoxicillin and chlarythromycin as the standard protocol of eradication within 14 days. Reevaluation by esophagogastroduodenoscopy examination will perform in the next 3 months to evaluate the treatment succesfull. Keywords: peptic ulcer, duodenum, H. pylori 1. Background also normal. The patient diagnosed with hematemesis suspect peptic ulcer. The patient was then admitted to ward Approximately 500,000 persons develop peptic ulcer disease and giving infusion ringer lactat, proton pump inhibitor in the United States each year. in 70 percent of patients it esomeprazole bolus 40 mg intravenous and continuous with occurs between the ages of 25 and 64 years. The annual 8 mg/ hours and planned for esofagogastroduodenoscopy to direct and indirect health care costs of the disease are evaluate the source of hematemesis. estimated at about $10 billion. However, the incidence of peptic ulcers is declining, possibly as a result of the increasing use of proton pump inhibitors and decreasing rates of Helicobacter pylori (H. -

Diagnosis and Management of Autoimmune Hemolytic Anemia in Patients with Liver and Bowel Disorders
Journal of Clinical Medicine Review Diagnosis and Management of Autoimmune Hemolytic Anemia in Patients with Liver and Bowel Disorders Cristiana Bianco 1 , Elena Coluccio 1, Daniele Prati 1 and Luca Valenti 1,2,* 1 Department of Transfusion Medicine and Hematology, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, 20122 Milan, Italy; [email protected] (C.B.); [email protected] (E.C.); [email protected] (D.P.) 2 Department of Pathophysiology and Transplantation, Università degli Studi di Milano, 20122 Milan, Italy * Correspondence: [email protected]; Tel.: +39-02-50320278; Fax: +39-02-50320296 Abstract: Anemia is a common feature of liver and bowel diseases. Although the main causes of anemia in these conditions are represented by gastrointestinal bleeding and iron deficiency, autoimmune hemolytic anemia should be considered in the differential diagnosis. Due to the epidemiological association, autoimmune hemolytic anemia should particularly be suspected in patients affected by inflammatory and autoimmune diseases, such as autoimmune or acute viral hepatitis, primary biliary cholangitis, and inflammatory bowel disease. In the presence of biochemical indices of hemolysis, the direct antiglobulin test can detect the presence of warm or cold reacting antibodies, allowing for a prompt treatment. Drug-induced, immune-mediated hemolytic anemia should be ruled out. On the other hand, the choice of treatment should consider possible adverse events related to the underlying conditions. Given the adverse impact of anemia on clinical outcomes, maintaining a high clinical suspicion to reach a prompt diagnosis is the key to establishing an adequate treatment. Keywords: autoimmune hemolytic anemia; chronic liver disease; inflammatory bowel disease; Citation: Bianco, C.; Coluccio, E.; autoimmune disease; autoimmune hepatitis; primary biliary cholangitis; treatment; diagnosis Prati, D.; Valenti, L. -

Challenging Cases of Hospitalized Patients with Cirrhosis
Challenging cases of hospitalized patients with cirrhosis Danielle Brandman, MD, MAS Associate Professor of Clinical Medicine Program Director, Transplant Hepatology Fellowship Inpatient Chief of Service, Hepatology October 17, 2019 Disclosure ■ Grant/research support: Grifols Case 1 ■ 63M with HCV cirrhosis is hospitalized due to worsened fluid retention, with ascites and lower extremity edema Case 1 ■ 63M with HCV cirrhosis is hospitalized due to worsened fluid retention, with ascites and lower extremity edema ■ He denies fever or frank abdominal pain, though is uncomfortable from abdominal distension. Case 1 ■ 63M with HCV cirrhosis is hospitalized due to worsened fluid retention, with ascites and lower extremity edema ■ He denies fever or frank abdominal pain, though is uncomfortable from abdominal distension. ■ He finds it difficult to walk as a result of severe leg edema Case 1 ■ VS: T37 HR 65 BP 110/70 RR 20 SpO2 98% ■ Gen: chronically ill ■ CV: 3+ BLE edema, anasarca ■ Resp: normal other than decreased BS at bases ■ GI: distended abdomen with dullness to percussion, nontender ■ Labs: WBC 4, hct 32, plt 60, INR 1.9, Na 122, Cr 2.5, total bili 6, albumin 2.8 Case 1 ■ What is your strategy for management of this patient’s volume overload? ■ How would you handle his hyponatremia? Approach to hyponatremia in cirrhosis Attar, CLD, 2019. IV albumin leads to resolution of hyponatremia Bajaj, AJG, 2018. IV albumin and ascites Treatments Study Outcomes sample ANSWER Albumin 40g n = 431 IRR for death 0.61 BIW x 2 weeks On favoring albumin then 40g/wk + diuretics, SMT vs ascites SMT alone MACHT Albumin 40g q n = 196 No difference in survival 15d + midodrine (only 173 or liver complications vs placebo analyzed) More LT in albumin Listed for group (68% vs 55%; LT, p=0.08) ascites Outpatient IV albumin use may improve survival and hospitalization Mortality Hospitalization Di Pascoli, Liver Int, 2018. -

Gastrointestinal Bleeding Gary A
Article gastroenterology Gastrointestinal Bleeding Gary A. Neidich, MD* Educational Gaps Sarah R. Cole, MD* 1. Pediatricians should be familiar with diseases that may present with gastrointestinal bleeding in patients at varying ages. Author Disclosure 2. Pediatricians should be aware of newer technologies for the identification and therapy Drs Neidich and Cole of gastrointestinal bleeding sources. have disclosed no 3. Pediatricians should be familiar with polyps that have and do not have an increased financial relationships risk of malignant transformation. relevant to this article. 4. Pediatricians should be familiar with medications used in the treatment of children This commentary does with gastrointestinal bleeding. not contain a discussion of an Objectives After completing this article, readers should be able to: unapproved/ investigative use of 1. Formulate a diagnostic and management plan for children with gastrointestinal a commercial product/ bleeding. device. 2. Describe newer techniques and their limitations for the identification of bleeding, including small intestinal capsule endoscopy and small intestinal enteroscopy. 3. Differentiate common and less common causes of gastrointestinal bleeding in children of varying ages. 4. Identify types of polyps that may present in childhood and which of these have malignant potential. Introduction An 11-year-old boy is seen in the emergency department after fainting at home. He has a 2-day history of headache and dizziness. Epigastric pain has been present during the past 2 days. His pulse is 150 beats per minute, and his blood pressure is 90/50 mm Hg. An in- travenous bolus of normal saline is administered; his hemoglobin level is 8.1 g/dl (81 g/L). -

Original Article Risk Factors for Upper Gastrointestinal Bleeding Requiring Hospitalization
Int J Clin Exp Med 2016;9(2):4539-4544 www.ijcem.com /ISSN:1940-5901/IJCEM0016204 Original Article Risk factors for upper gastrointestinal bleeding requiring hospitalization Yi Jiang1, Yanhua Li2, Hong Xu2, Yang Shi2, Yanqing Song2, Yanyan Li2 1Second Hospital of Jilin University, Changchun 130051, Jilin, China; 2First Hospital of Jilin University, Changchun 130021, Jilin, China Received September 15, 2015; Accepted January 9, 2016; Epub February 15, 2016; Published February 29, 2016 Abstract: Objective: To analyze the causes of upper gastrointestinal bleeding (UGIB) in northeast China. Methods: In-patients with hematemesis, melena, and/or hematochezia who underwent upper endoscopy with an identified source at The First Hospital of Jilin University were enrolled in this study. The cause of bleeding, patient age, clinical features and drugs were retrospectively evaluated. Results: A total of 1,740 patients were included in this study. Among these patients, mean age was 57 ± 13 years and 1340 (77%) were male. Bleeding from varices was more common than from ulcers among patients with hematemesis with/without melena (47% vs. 30%, P<0.01). Varices were the most common cause of gastrointestinal bleeding in 672 (39%) patients, followed by peptic ulcer disease in 600 (34%) patients. One hundred twenty (7%) patients had acute UGIB associated with drugs, in which non- steroidal anti-inflammatory drugs (NSAIDs) were identified as the main drugs associated with UGIB. Among these 120 patients, 60 (50%) patients used aspirin, 9 (8%) patients used aspirin combined with clopidogrel, 30 (25%) patients used Chinese herbal medicines, 18 (15%) used aminopyrine-phenacetin, and 12 (10%) patients used cor- ticosteroids. -

Diagnosis and Management of Upper Gastrointestinal Bleeding in Children
J Am Board Fam Med: first published as 10.3122/jabfm.2015.01.140153 on 7 January 2015. Downloaded from CLINICAL REVIEW Diagnosis and Management of Upper Gastrointestinal Bleeding in Children Susan Owensby, DO, Kellee Taylor, DO, and Thad Wilkins, MD, MBA Upper gastrointestinal bleeding is an uncommon but potentially serious, life-threatening condition in children. Rapid assessment, stabilization, and resuscitation should precede all diagnostic modalities in unstable children. The diagnostic approach includes history, examination, laboratory evaluation, endo- scopic procedures, and imaging studies. The clinician needs to determine carefully whether any blood or possible blood reported by a child or adult represents true upper gastrointestinal bleeding because most children with true upper gastrointestinal bleeding require admission to a pediatric intensive care unit. After the diagnosis is established, the physician should start a proton pump inhibitor or histamine 2 receptor antagonist in children with upper gastrointestinal bleeding. Consideration should also be given to the initiation of vasoactive drugs in all children in whom variceal bleeding is suspected. An endoscopy should be performed once the child is hemodynamically stable. (J Am Board Fam Med 2015; 28:134–145.) Keywords: Gastrointestinal Hemorrhage, Pediatrics Upper gastrointestinal bleeding (UGIB) is an un- sive care, advances in diagnosis and treatment, as copyright. common but potentially serious and life-threaten- well as in the stabilization and management of ing clinical condition in children. Anatomically, the critically ill patients. Mortality can be decreased upper gastrointestinal (GI) tract includes the by early identification of UGIB, and improved esophagus to the ligament of Treitz; therefore morbidity and mortality are most often the result UGIB includes bleeding that originates throughout of a multidisciplinary approach to care.3 Among this region. -

Liver Disease
Liver Disease What is the liver and what does it do? The liver is a remarkable and complex organ located in the very front of the abdomen, behind the diaphragm. The liver is responsible for metabolism and storage of nutrients, processing toxins and drugs, synthesizing proteins and other compounds, and forming and secreting bile to aid in digestion. The portal vein is a blood vessel that brings absorbed digested nutrients from the intestines to the liver for further processing and storage. Blood percolates through the liver before entering into the body as a whole. Bile is a greenish substance secreted into the small intestine via the gall bladder and bile ducts that contains compounds that aid in digestion of fats; certain drugs or toxins may also be excreted this way Albumin is the major blood protein made by the liver that helps with a wide array of functions in the body Coagulation factors are proteins made in the liver that work with platelets and blood vessels to help the blood to clot What types of liver disease occur in dogs and cats? Cats commonly get at least four different liver conditions: hepatic lipidosis, infectious cholangiohepatitis, immune-mediated cholangiohepatitis, and hepatic lymphoma. Lymphoma is a cancer that can be seen in both high-grade (aggressive and rapidly progressive) and low-grade (insidious and slowly progressive). Although other liver cancers can occur in cats, they are less common. Immune- mediated cholangiohepatitis is a condition wherein the immune system attacks the liver and associated structures; it can be associated with inflammatory bowel disease and pancreatitis in certain cats. -

Serum Lactate Is a Poor Marker of Bowel Ischemia Following Angioembolization for Lower Gastrointestinal Bleeding
4 Correspondence Page 1 of 4 Serum lactate is a poor marker of bowel ischemia following angioembolization for lower gastrointestinal bleeding Lynn Soo Hoon Yeo1^, Jiayan Wee2, Kumaresh Venkatesan3 1Department of Anaesthesia, Khoo Teck Puat Hospital/Woodlands Health Campus, Singapore; 2Department of Anaesthesiology, Intensive Care and Pain Medicine, Tan Tock Seng Hospital, Singapore; 3Department of Anaesthesia, Khoo Teck Puat Hospital, Singapore Correspondence to: Lynn Soo Hoon Yeo. Department of Anaesthesia, Khoo Teck Puat Hospital/Woodlands Health Campus, 90 Yishun Central, Singapore 768828, Singapore. Email: [email protected]. Received: 17 April 2020; Accepted: 19 November 2020; Published: 30 December 2020. doi: 10.21037/dmr-20-51 View this article at: http://dx.doi.org/10.21037/dmr-20-51 In patients with suspected active bleeding from the (ED) with abdominal pain and per-rectal bleeding. His lower gastrointestinal tract, urgent angiography and abdomen was soft, tender over left lower quadrant with angioembolization of bleeding vessels is an accepted no generalized peritonism. Computed tomography (CT) management strategy (1). Technological advances in mesenteric angiogram performed showed active contrast interventional radiology have allowed endovascular extravasation in one of the hepatic flexure diverticula, treatment of lower gastrointestinal tract bleeding to be safer keeping with an acute bleed of the right colic artery. and more precise (2). Angioembolization of right colic artery was performed. A known complication after angioembolization of Serum lactate levels were trended routinely after the bleeding vessels is the development of ischemic bowel. The angioembolization procedure. Serum lactate levels remained incidence of ischemic bowel after angioembolization has low at 0.8 to 1.7 mmol/L, however, the patient developed been reported as 13% to 24% in different case series (3,4). -
Stool-Based Diagnoses Made Ridiculously Simple
The POOP SCOOP Stool-based Diagnoses Made Ridiculously Simple AKSHATA MOGHE MD,PHD DIVISION OF GASTROENTEROLOGY, HEPATOLOGY AND NUTRITION Objective Describe how different stool characteristics can guide diagnosis and decision making Outline A step-wise guide to a good poop history - color, consistency, frequency GI bleed! - where is this blood coming from? - and what can I do (before paging GI) ? Everyone loves a good poopy tale “POOP HISTORY” STEP 1: COLOR STEP 2: CONSISTENCY STEP 3: FREQUENCY Step 1: Color Step 1: Color Brown: normal Green: quick transit, breastfed babies Yellow: if also greasy, voluminous and foul-smelling, suspect fat malabsorption (pancreatic insufficiency, celiac disease) - 72 hr fecal fat excretion (> 6g/day is pathologic) White/Clay colored: also called ‘acholic’ stool, suggests biliary obstruction, ask if urine is darker than usual Black: if black and TARRY, suspect upper GI bleed if black but normal consistency/hard, check medications (Iron, pepto-bismol) Red: Blood in stool. Ahem, we will get there Step 2: Consistency CONSTIPATION ALSO NORMAL NORMAL DIARRHEA Step 3: Frequency Constipation - duration - diet, medications and lifestyle change - motility issue? Normal: 3 times per day once in 3 days Diarrhea - duration - diet, travel, antibiotics/laxatives history - Infectious? Secretory vs. osmotic? IBD? Outline A step-wise guide to a good poop history - color, consistency, frequency GI bleed! - where is this blood coming from? - and what can I do (before paging GI) ? 1. COLOR 2.CONSISTENCY 3. FREQUENCY Anatomy