Gomisin M2 Ameliorates Atopic Dermatitis-Like Skin Lesions Via Inhibition of STAT1 and NF-B Activation in 2,4-Dinitrochlorobenze
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Transport Biofuels' R&D Roadmap in Korea
IEA Bioenergy Task 39 Beijing Meeting, China, April 07-09, 2018 Country Report (Korea) 2018. 4. 7. Jin-Suk Lee IEA Bioenergy Task 39 Beijing Meeting, China, April 07-09, 2018 Presentation Agenda • Implementation Agenda - Main drivers for biofuel - Biofuels policy - Market developments - Biofuel facilities - R&D Information IEA Bioenergy Task 39 Beijing Meeting, China, April 07-09, 2018 Main Drivers for Biofuels Climate Change Mitigation RFS IEA Bioenergy Task 39 Beijing Meeting, China, April 07-09, 2018 Biofuels Policy Policies for biofuel supply Biofuel obligations Types of Year Biodiesel, % Yes/No (Comments) Policy 2010 2.0 Mandates B3, Effective from 2018 2011 2.0 2012 2.0 R&D funding Several funding are available 2013 2.0 2014 2.0 Market for Very difficult new biofuels 2015 2.5 2016 2.5 Others None 2017 2.5 2018 3.0 IEA Bioenergy Task 39 Beijing Meeting, China, April 07-09, 2018 Market Developments Summary of transport fuel consumption (ML) Year Gasoline Diesel fuels Aviation fuel Biodiesel Bioethanol Market share (%) 2006 9.52 x 103 1.78 x 104 3.19 x 103 40 0 0.13 2007 9.93 x 103 1.81 x 104 3.31 x 103 100 0 0.32 2008 1.0 x 104 1.70 x 104 3.17 x 103 200 0 0.66 2009 1.04 x 104 1.65 x 104 3.33 x 103 300 0 0.99 2010 1.09 x 104 1.67 x 104 3.57 x 103 400 0 1.28 2011 1.10 x 104 1.66 x 104 3.60 x 103 400 0 1.28 2012 1.14 x 104 1.70 x 104 3.82 x 103 400 0 1.24 2013 1.16 x 104 1.79 x 104 3.86 x 103 400 0 1.19 2014 1.17 x 104 1.83 x 104 4.07 x 103 400 0 1.17 2015 1.22 x 104 1.98 x 104 4.35 x 103 500 0 1.38 2016 1.26 x 104 2.11 x 104 4.65 x 103 500 0 1.30 2017 Source: KEEI, http://www.keei.re.kr/main.nsf/index.html IEA Bioenergy Task 39 Beijing Meeting, China, April 07-09, 2018 Biofuel Facilities Biodiesel Plant Location Installed capacity [ML/yr] Feedstock Status M Energy Pyongtaek 148 Used cooking oil Mothballed Danseok Industry Siheung 113 Vegetable oil, Used cookin In production Pyongtaek 180 g oil Emac Bio Soonchun 50 Used cooking oil In production Jeongeup 32 SK Chemcial. -

Democratic People's Republic of Korea
Operational Environment & Threat Analysis Volume 10, Issue 1 January - March 2019 Democratic People’s Republic of Korea APPROVED FOR PUBLIC RELEASE; DISTRIBUTION IS UNLIMITED OEE Red Diamond published by TRADOC G-2 Operational INSIDE THIS ISSUE Environment & Threat Analysis Directorate, Fort Leavenworth, KS Topic Inquiries: Democratic People’s Republic of Korea: Angela Williams (DAC), Branch Chief, Training & Support The Hermit Kingdom .............................................. 3 Jennifer Dunn (DAC), Branch Chief, Analysis & Production OE&TA Staff: North Korea Penny Mellies (DAC) Director, OE&TA Threat Actor Overview ......................................... 11 [email protected] 913-684-7920 MAJ Megan Williams MP LO Jangmadang: Development of a Black [email protected] 913-684-7944 Market-Driven Economy ...................................... 14 WO2 Rob Whalley UK LO [email protected] 913-684-7994 The Nature of The Kim Family Regime: Paula Devers (DAC) Intelligence Specialist The Guerrilla Dynasty and Gulag State .................. 18 [email protected] 913-684-7907 Laura Deatrick (CTR) Editor Challenges to Engaging North Korea’s [email protected] 913-684-7925 Keith French (CTR) Geospatial Analyst Population through Information Operations .......... 23 [email protected] 913-684-7953 North Korea’s Methods to Counter Angela Williams (DAC) Branch Chief, T&S Enemy Wet Gap Crossings .................................... 26 [email protected] 913-684-7929 John Dalbey (CTR) Military Analyst Summary of “Assessment to Collapse in [email protected] 913-684-7939 TM the DPRK: A NSI Pathways Report” ..................... 28 Jerry England (DAC) Intelligence Specialist [email protected] 913-684-7934 Previous North Korean Red Rick Garcia (CTR) Military Analyst Diamond articles ................................................ -

A Taxonomic Study of the Genus Fimbristylis 329 Appendix 1
A taxonomic study of the genus Fimbristylis 329 Appendix 1. Examined specimens of Fimbristylis species in Korea. Fimbristylis ovata (Burm.f.) J. Kern 쇠하늘지기 KOREA. Jeju-do: Seogwipo-si, 17 Aug 2017, J. H. Kim 174384, J. H. Kim 174386, J. H. Kim 174393 (JNU). Fimbristylis dipsacea (Rottb.) C. B. Clarke var. verrucifera (Maxim.) T. Koyama 푸른하늘지기 KOREA. Busan-si: Gijang-gun, 18 Jun 2015, J. H. Kim 152159, J. H. Kim 152160 (JNU); Jeollanam-do: Gangjin-gun, 19 Aug 2012, J. H. Kim 1204 (JNU); Jeollabuk-do: Jeongeup-si, 28 Sep 2013, J. H Kim 1313, J. H. Kim 13140, J. H. Kim 13147, J. H. Kim 13148 (JNU); 18 Sep 2015, J. H. Kim 152527, J. H. Kim 152530 (JNU); Gunsan-si, 23 Sep 2015, J. H. Kim 152585 (JNU). Fimbristylis stauntonii Debeaux and Meyen 밭하늘지기 KOREA. Chungcheongbuk-do: Danyang-gun, 30 Jul 2012, J. H. Kim 12137, J. H. Kim 12138, J. H. Kim 12141, J. H. Kim 12144, J. H. Kim 12149, J. H. Kim 12150 (JNU); Gyeongsangnam-do: Changnyeong-gun, 6 Oct 2013, J. H. Kim 13079–J. H. Kim 13081 (JNU); Jeollanam-do: Yeonggwang-gun, 31 Aug 2013, J. H. Kim 152600 (JNU). Fimbristylis sericea (Poir) R. Br. 털잎하늘지기 KOREA. Jeollanam-do: Sinan-gun, 2 Nov 2006, J. H. Kim 233; 29 Aug 1997, H. T. Im 49621; 2 Sep 2005, H. B. Shim and S. G. Kwon 3085 (KB); Wando-gun, 16 Oct 2010, J. H. Kim 1877 (KB); 16 Sep 2014, J. H. Kim 141483, J. H. Kim 141484; Jeollabuk-do: Gochang-gun, 9 Aug 2008, J. -

Tax Practice Group Tax Practice Group
TAX PRACTICE GROUP TAX PRACTICE GROUP YOON & YANG Yoon & Yang LLC, which was established in 2003 through the merger of Yoon & Partners and Roh LLC & Yang, has provided the optimized legal service to clients by maintaining perfect balance between consulting and litigation services. Yoon & Yang LLC has systematically streamlined its expertise and know-how in every area of cor- porate counseling and litigation for the purpose of providing a more specialized legal service. The firm’s professionals are grouped into specialized teams according to practice area centering on the expertise and know-how of the experts in their respective fields. The close cooperation between the teams enables the firm to provide optimized one-stop legal services. Yoon & Yang LLC practices law with the mindset of viewing our services from the perspective of cli- ents based on the staunch belief that it is only possible to provide the highest quality legal services when the requisite care and attention are paid to clients and the trust of clients has been earned. Yoon & Yang LLC aims at providing the highest quality legal services, while observing ethical prin- ciples and valuing democratic relationships. The firm strives to grow into a world-class law firm based in Korea to provide a one-stop total legal service and develop together with our clients. TAX Yoon & Yang Tax Practice Group is comprised of a team of leading attorneys, certified public accoun- PRACTICE tants, and certified public tax accountants with depth of knowledge and decades of experiences who GROUP can provide the highest quality services for diverse tax issues. -

The Effect of City-County Consolidation in South Korea.Pdf
The Effect of City-County Consolidation in South Korea by Byoung-Ik Min A dissertation submitted to the Graduate Faculty of Auburn University in partial fulfillment of the requirements for the Degree of Doctor of Philosophy Auburn, Alabama August 3, 2013 Keywords: city-county consolidation, technical efficiency, financial status, disparity, local government size, boundary Copyright 2013 by Byoung-Ik Min Approved by Cynthia J. Bowling, Chair, Professor of Political Science and Public Administration Steven Brown, Professor of Political Science and Public Administration Hua Xu, Assistant Professor of Political Science and Public Administration Keren Deal, Professor of Accounting Abstract In 1994, the South Korean central government initiated a massive merger of city and county governments, and during the next two years, a total of 40 consolidated cities were established. Following the city-county consolidations, there has been significant debate regarding whether the local mergers achieved the desired effect. This study seeks to determine whether the technical efficiency of the consolidated governments improved following the mergers, whether their financial status improved, and whether the disparities between the urban and rural areas were reduced. The literature review in this study identifies the most significant literature and the most prominent theories pertaining governmental size and boundary. It also highlights local governmental consolidation studies previously conducted in both the U.S. and South Korea. Finally, it describes the South Korean local governmental structure, and discusses the process of the city-county consolidations that took place in South Korea from 1994 through 1995. To facilitate the research and analysis related to the city-county consolidations in South Korea, this study has identified and tests the following three hypotheses: •H1: The technical efficiency of consolidated governments improved following the city-county consolidations. -

Case Study of Honam KTX in Korea
applied sciences Article Analysis of Mobile Phone Data to Compare Mobility Flows and Hotspots Before and After the Opening of High-Speed Railway: Case Study of Honam KTX in Korea Jin Ki Eom * , Kwang-Sub Lee, Ji Young Song and Jun Lee Railroad Policy Research Team, Future Transport Policy Research Division, Korea Railroad Research Institute, Uiwang 16105, Korea; [email protected] (K.-S.L.); [email protected] (J.Y.S.); [email protected] (J.L.) * Correspondence: [email protected]; Tel.: +82-31-460-5467 Received: 26 June 2020; Accepted: 18 July 2020; Published: 21 July 2020 Abstract: Mobile phone data provides information, such as the home (origin) and current locations of people. The data can be used to analyze the impact of new high-speed railway (HSR) openings. This study examined the population observed in stations and cities of the Honam HSR line in Korea, based on mobile phone data recorded one year before and after its opening. We analyzed the volume of the population observed at each railway station, density of the distance between home and station, and activity hotspots in a city. The results show that the number of people and travel distance increased after the opening of the HSR. The distance to access railway stations increased, as the HSR saves travel time. Moreover, the activity hotspots in a city increased after the opening of the HSR, as more people gathered near the station area. The findings show that the mobility measures enhanced after the opening of the HSR for regional travel and local activities. -

National Food Cluster Is an Industrial Complex Designed to Incubate an R&D- and Export-Oriented Food Industry
English Commercial site Iksan IC Gas station Parking lot The National Food Cluster is an industrial complex designed to incubate an R&D- and export-oriented food industry. Industrial facilities Land Use Plan Industrial facilities ■Location : Ilwon, Wanggung-myeon, Iksan-si, Park Jeollabuk-do, Korea All-in-one for the food industry ■Size : 2,322,932m² Industrial facilities Industrial facilities ■Target business : Food and beverage manufacturing Zoom-in on global possibilities and related industries ■Sales price : 150,761 won/m² (498.383 won/3.3m²) Find successful solutions Industrial facilities A global food city engineered with innovation Logistics facility site for the food business Gas station Residential District Parking lot Agency for National Food Cluster Parking lot Source Logistics facility site Semi-residential District Wastewater treatment plant Business Support facilities Center in the National Food Cluster National Food Cluster Research facility site Electric supply utility S3 Support facilities Fire Park Neighborhood amenities station Pedestrian walkway Industrial facilities Industrial facilities Research Park facility site Foreign Waste disposal facility Support facilities Investment Zone Industrial facilities Public office building Multi-purpose site Housing Zone Religious facilities Parking lot Industrial facilities Industrial facilities Commercial site Detention pond Logistics facility site Gas station Green buffer zone Industrial facilities Industrial facilities Industrial facilities Industrial facilities Detention pond Industrial facilities Detention pond Park Wastewater Industrial facilities treatment plant Industrial facilities Waste disposal facility Religious facilities Semi-residential Industrial facilities District Parking lot Semi-residential District Industrial facilities Park Electric supply utility Neighborhood amenities Residential District Housing Zone Industrial facilities Religious facilities This plan is for reference only. -
Bitter Harvest. Exploitation and Forced Labour of Migrant Agricultural
BITTER HARVEST EXPLOITATION AND FORCED LABOUR OF MIGRANT AGRICULTURAL WORKERS IN SOUTH KOREA Amnesty International is a global movement of more than 3 million supporters, members and activists in more than 150 countries and territories who campaign to end grave abuses of human rights. Our vision is for every person to enjoy all the rights enshrined in the Universal Declaration of Human Rights and other international human rights standards. We are independent of any government, political ideology, economic interest or religion and are funded mainly by our membership and public donations. First published in 2014 by Amnesty International Ltd Peter Benenson House 1 Easton Street London WC1X 0DW United Kingdom © Amnesty International 2014 Index: ASA 25/004/2014 Original language: English Printed by Amnesty International, International Secretariat, United Kingdom All rights reserved. This publication is copyright, but may be reproduced by any method without fee for advocacy, campaigning and teaching purposes, but not for resale. The copyright holders request that all such use be registered with them for impact assessment purposes. For copying in any other circumstances, or for reuse in other publications, or for translation or adaptation, prior written permission must be obtained from the publishers, and a fee may be payable. To request permission, or for any other inquiries, please contact [email protected] Cover photo: Agricultural land with greenhouses in below freezing tempratures in Gyeonggi province. © Amnesty International / Robert Godden amnesty.org CONTENTS 1. Executive Summary ................................................................................................... 5 1.1. Exploitation and abuse of migrant agricultural workers ............................................ 6 1.2. How the EPS increases migrant workers’ risk of exploitation ................................... -
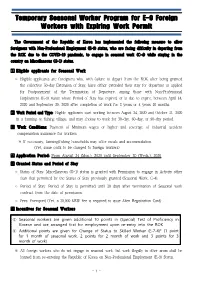
Temporary Seasonal Worker Program for E-9 Foreign Workers with Expiring Work Permit
Temporary Seasonal Worker Program for E-9 Foreign Workers with Expiring Work Permit The Government of the Republic of Korea has implemented the following measure to allow foreigners with Non-Professional Employment (E-9) status, who are facing difficulty in departing from the ROK due to the COVID-19 pandemic, to engage in seasonal work (C-4) while staying in the country on Miscellaneous (G-1) status. Eligible applicants for Seasonal Work ◦ Eligible applicants are foreigners who, with failure to depart from the ROK after being granted the collective 50-day Extension of Stay, have either extended their stay for departure or applied for Postponement of the Termination of Departure, among those with Non-Professional Employment (E-9) status whose Period of Stay has expired, or is due to expire, between April 14, 2020 and September 30, 2020 after completion of work for 3 years or 4 years 10 months. Work Period and Type: Eligible applicants start working between August 24, 2020 and October 31, 2020 in a farming or fishing village, and may choose to work for 30-day, 60-day, or 90-day period. Work Conditions: Payment of Minimum wages or higher and coverage of industrial accident compensation insurance for workers ※ If necessary, farming/fishing households may offer meals and accommodation. (Yet, some costs to be charged to foreign workers) Application Period: From August 24 (Mon.), 2020 until September 30 (Weds.), 2020 Granted Status and Period of Stay ◦ Status of Stay: Miscellaneous (G-1) status is granted with Permission to engage in Activity other than that permitted by the Status of Stay previously granted (Seasonal Work, C-4). -

The Impacts of High-Speed Rail Extensions on Accessibility and Spatial Equity Changes in South Korea from 2004 to 2018
The impacts of high-speed rail extensions on accessibility and spatial equity changes in South Korea from 2004 to 2018 By: Hyojin Kim and Selima Sultana Kim, H. and Sultana, S. The impacts of high-speed rail extensions on accessibility and spatial equity changes in South Korea from 2004 to 2018. Journal of Transport Geography, Vol. 45 (May 2015), pp. 48-61. Made available courtesy of Elsevier: https://doi.org/10.1016/j.jtrangeo.2015.04.007 This work is licensed under a Creative Commons Attribution- NonCommercial-NoDerivatives 4.0 International License. ***© 2015 Elsevier. Reprinted with permission. This version of the document is not the version of record. Abstract: The construction of South Korean High-Speed Rail (HSR) or Korea Train eXpress (KTX) has been evolving in phases since its first operation in 2004. This development raises concerns whether the benefits from the extended HSR network would again be limited to the initial HSR corridors and will deepen the inequalities in accessibility with the rising issue of uneven regional development of the country. This paper measures the accessibility of each stage of HSR network extension and evaluates its spatial distribution, variation, and changes using weighted averaged travel time and potential accessibility indicators. The results of this study find different accessibility impacts from each stage of HSR extension. Although travel-time reduction and increased attractions have been widened in more cities by each HSR extension, the spatial equity is degenerated by the extension in 2010/2011 as the improvement of accessibility has been concentrated in cities along the primary HSR corridor near the already-advantageous Seoul capital area. -

The Feeling Korea CONTENTS 01 Program Guide 1
2019 Winter The Feeling Korea CONTENTS 01 Program Guide 1. The Feeling Korea 2. Timeline 3. Period 4. How to apply 5. Participants 6. Available slots 7. Participation Fee 8. Credit 9. Schedule 10. Program details 02 Details 1. Flight Booking 2. Pick-up Service 3. How to get to JBNU 4. Drop-off Service 5. Visa 6. Housing 7. University’s Facilities 8. Contact us 01 Program Guide 1 The Feeling Korea : Feel Fun and Interesting Korean Culture / The Feeling Korea Do you read a book to study the knowledge of Korean culture? From now, you don’t need to do anymore. Feel Korean culture by traveling, playing, looking at, listening to, and experiencing it. With the Feeling Korea Program, you can explore various Korean cultures which you haven’t known. If you join the program, you can not only make pottery, learn Taekwondo, and experience Korean traditional costume but also visit the largest amusement park in Korea. Enjoy these activities with The Feeling Korea. / Jeonbuk National University Jeonbuk National University was founded to grow local talent in 1947. Our university is the first university in Jeolla and Chungcheong province and is a flagship national university which has led local and national development. JBNU has the main campus in Jeonju, the specialized campus as agriculture and veterinary science in Iksan, and other rural campuses in Gochang, Wanju, Jeongeup, Saemangeum Gunsan. JBNU provides 1,024 full-time professors, 900 employees, and 21,753 students with educational, research, and support facilities. In addition, JBNU is comprised of 15 colleges, 12 graduate schools and 96 major departments. -

Energy Info. Korea 2008
2008 Energy Info. Korea 2008. 4 Preliminary Edition Ministry of Knowledge Economy Korea Energy Economics Institute 2008 Energy Info. Korea Preliminary Edition Energy Info. Korea is Published by KEEI (Korea Energy Economics Institute, Republic of Korea) Publisher : Ki-Yual Bang Editor : Ki-Choo Lim Chang-Bong Chung Korea Energy Economics Institute 665-1 Naeson-dong, Uiwang-si, Gyeonggi-do, Korea Tel : 82-31-420-2114, 82-31-420-2295 Fax : 82-31-420-2164 Homepage : http://www.keei.re.kr E-mail : [email protected], [email protected] All rights reserved by KEEI. Reproduction in whole or in part without written permission is prohibited. ISBN 978-89-5504-166-8 93320 2008 Preliminary Edition Energy Info. Korea Contents ENERGY FLOW CHART 2007 / 4 1. Major Energy Indicators / 8 2. Primary Energy Supply / 10 3. Transformation / 12 4. Primary Energy Consumption / 16 5. Final Energy Consumption / 18 6. Energy Balances / 28 7. CO2 Emissions / 36 8. Imports / 38 9. Prices / 46 10. Reserves & Distribution Map / 50 11. Energy Consumption in the Korean Peninsula / 54 12. World Energy Statistics / 58 Appendices / 68 ENERGY FLOW CHART 2007 Generation Production ImportsImports Coal 1.3 Coal 55.6 Generation Nuclear 35.7 Oil 157.5 Coal 37.4 Production Hydro 1.3 (Products132.2) Export Oil 0.4 Electricity 21.9 Others 4.8 LNG 31.8 Oil 41.9 LNG 13.5 Heat 0.9 Primary Energry Supply(240.5 Mtoe) Trans Bunkering Stock Change Crube Oil 120.5 Oil Prod. 132.2 Oil 7.7 Gasoline 10.3 Diesel 37.0 B-C 28.3 Naphtha 24.0 Note : Includes Refinery Input & Output Others 32.5 (Crude Oil 1ton = 7.33bbl) Source : Energy Balances 2007(Preliminary Data) Refinery (million toe) District Heating Final Consumption Power Industry 101.8 Oil 0.4 Transportation 37.5 LNG 0.8 Resid/Comm.