NIH Public Access Author Manuscript J Pharmacol Exp Ther
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug & Alcohol Testing Program
Pottawattmie County Drug & Alcohol Testing Program Appendix A Table of Contents POLICY STATEMENT ...................................................................................................................................... 3 SCOPE ............................................................................................................................................................ 4 EDUCATION AND TRAINING .......................................................................................................................... 4 DESIGNATED EMPLOYER REPRESENTATIVE (DER): ....................................................................................... 5 DUTY TO COOPERATE ................................................................................................................................... 5 EMPLOYEE ADMISSION OF ALCOHOL AND CONTROLLED SUBSTANCE USE: (49 CFR Part 382.121) ... 6 PROHIBITED DRUGS AND ILLEGALLY USED CONTROLLED SUBSTANCES: ..................................................... 7 PROHIBITED BEHAVIOR AND CONDUCT: ...................................................................................................... 8 DRUG & ALCOHOL TESTING REQUIREMENTS (49 CFR, Part 40 & 382) ............................................... 10 DRUG & ALCOHOL TESTING CIRCUMSTANCES (49 CFR Part 40 & 382) .............................................. 12 A. Pre-Employment Testing: .................................................................................................... 12 B. Reasonable Suspicion Testing: ......................................................................................... -

Pentameric Ligand-Gated Ion Channel ELIC Is Activated by GABA And
Pentameric ligand-gated ion channel ELIC is activated PNAS PLUS by GABA and modulated by benzodiazepines Radovan Spurnya, Joachim Ramerstorferb, Kerry Pricec, Marijke Bramsa, Margot Ernstb, Hugues Nuryd, Mark Verheije, Pierre Legrandf, Daniel Bertrandg, Sonia Bertrandg, Dennis A. Doughertyh, Iwan J. P. de Esche, Pierre-Jean Corringerd, Werner Sieghartb, Sarah C. R. Lummisc, and Chris Ulensa,1 aDepartment of Cellular and Molecular Medicine, Laboratory of Structural Neurobiology, Catholic University of Leuven, 3000 Leuven, Belgium; bDepartment of Biochemistry and Molecular Biology of the Nervous System, Medical University of Vienna, A-1090 Vienna, Austria; cDepartment of Biochemistry, University of Cambridge, Cambridge CB2 1QW, United Kingdom; dPasteur Institute, G5 Group of Channel-Receptor, Centre National de la Recherche Scientifique, 75724 Paris, France; eDepartment of Medicinal Chemistry, VU University Amsterdam, 1081 HV, Amsterdam, The Netherlands; fSOLEIL Synchrotron, 91192 Gif sur Yvette, France; gHiQScreen, CH-1211 Geneva, Switzerland; and hCalifornia Institute of Technology, Pasadena, CA 91125 Edited* by Jean-Pierre Changeux, Institut Pasteur, Paris Cedex 15, France, and approved September 10, 2012 (received for review May 24, 2012) GABAA receptors are pentameric ligand-gated ion channels in- marized in SI Appendix, Table S1). In addition, it has been volved in fast inhibitory neurotransmission and are allosterically suggested that the GABA carboxylate group is stabilized through modulated by the anxiolytic, anticonvulsant, and sedative-hypnotic electrostatic interactions with Arg residues on the principal and benzodiazepines. Here we show that the prokaryotic homolog ELIC complementary faces of the binding site (4, 7–9). For benzo- also is activated by GABA and is modulated by benzodiazepines diazepines, the individual contributions of residues in loops A–F with effects comparable to those at GABAA receptors. -

Pharmacological Treatments in Insomnia
Pharmacological treatments in insomnia Sue Wilson Centre for Neuropsychopharmacology, Division of Brain Sciences, Imperial College, London Drugs used in insomnia Licensed for insomnia •GABA-A positive allosteric modulators •melatonin (modified release) •promethazine •diphenhydramine •doxepin (USA) Unlicensed prescribed frequently •antihistamines (and OTC) •antidepressants Sometimes prescribed drugs for psychosis Some GABA-A positive allosteric modulators Drugs acting at the GABA-A benzodiazepine receptor zopiclone zolpidem zaleplon benzodiazepines eg temazepam, lorazepam (safe in overdose, as long as no other drug involved) Drugs acting at the barbiturate/alcohol receptor chloral hydrate/chloral betaine clomethiazole (dangerous in overdose) GABA calms the brain Gamma aminobutyic acid (GABA) is the main inhibitory transmitter in the mammalian central nervous system. It plays the principal role in reducing neuronal excitability and its receptors are prolific throughout the brain, in cortex, limbic system, thalamus and cerebellum sedative Increase anticonvulsant GABA anxiolytic function ataxia, memory effects Effects of GABA-A positive allosteric modulators •These drugs enhance the effect of GABA, the main inhibitory neurotransmitter in the brain •They all produce sedation, sleep promotion, ataxia, muscle relaxation, effects on memory, anticonvulsant effects •Therefore for insomnia the duration of action of the drug is important – these effects are unwanted during the day Effects of these GABA-ergic drugs on sleep EEG/PSG • Appearance of -

Calculating Equivalent Doses of Oral Benzodiazepines
Calculating equivalent doses of oral benzodiazepines Background Benzodiazepines are the most commonly used anxiolytics and hypnotics (1). There are major differences in potency between different benzodiazepines and this difference in potency is important when switching from one benzodiazepine to another (2). Benzodiazepines also differ markedly in the speed in which they are metabolised and eliminated. With repeated daily dosing accumulation occurs and high concentrations can build up in the body (mainly in fatty tissues) (2). The degree of sedation that they induce also varies, making it difficult to determine exact equivalents (3). Answer Advice on benzodiazepine conversion NB: Before using Table 1, read the notes below and the Limitations statement at the end of this document. Switching benzodiazepines may be advantageous for a variety of reasons, e.g. to a drug with a different half-life pre-discontinuation (4) or in the event of non-availability of a specific benzodiazepine. With relatively short-acting benzodiazepines such as alprazolam and lorazepam, it is not possible to achieve a smooth decline in blood and tissue concentrations during benzodiazepine withdrawal. These drugs are eliminated fairly rapidly with the result that concentrations fluctuate with peaks and troughs between each dose. It is necessary to take the tablets several times a day and many people experience a "mini-withdrawal", sometimes a craving, between each dose. For people withdrawing from these potent, short-acting drugs it has been advised that they switch to an equivalent dose of a benzodiazepine with a long half life such as diazepam (5). Diazepam is available as 2mg tablets which can be halved to give 1mg doses. -

The Emergence of New Psychoactive Substance (NPS) Benzodiazepines
Issue: Ir Med J; Vol 112; No. 7; P970 The Emergence of New Psychoactive Substance (NPS) Benzodiazepines. A Survey of their Prevalence in Opioid Substitution Patients using LC-MS S. Mc Namara, S. Stokes, J. Nolan HSE National Drug Treatment Centre Abstract Benzodiazepines have a wide range of clinical uses being among the most commonly prescribed medicines globally. The EU Early Warning System on new psychoactive substances (NPS) has over recent years detected new illicit benzodiazepines in Europe’s drug market1. Additional reference standards were obtained and a multi-residue LC- MS method was developed to test for 31 benzodiazepines or metabolites in urine including some new benzodiazepines which have been classified as New Psychoactive Substances (NPS) which comprise a range of substances, including synthetic cannabinoids, opioids, cathinones and benzodiazepines not covered by international drug controls. 200 urine samples from patients attending the HSE National Drug Treatment Centre (NDTC) who are monitored on a regular basis for drug and alcohol use and which tested positive for benzodiazepine class drugs by immunoassay screening were subjected to confirmatory analysis to determine what Benzodiazepine drugs were present and to see if etizolam or other new benzodiazepines are being used in the addiction population currently. Benzodiazepine prescription and use is common in the addiction population. Of significance we found evidence of consumption of an illicit new psychoactive benzodiazepine, Etizolam. Introduction Benzodiazepines are useful in the short-term treatment of anxiety and insomnia, and in managing alcohol withdrawal. 1 According to the EMCDDA report on the misuse of benzodiazepines among high-risk opioid users in Europe1, benzodiazepines, especially when injected, can prolong the intensity and duration of opioid effects. -

A Review of the Evidence of Use and Harms of Novel Benzodiazepines
ACMD Advisory Council on the Misuse of Drugs Novel Benzodiazepines A review of the evidence of use and harms of Novel Benzodiazepines April 2020 1 Contents 1. Introduction ................................................................................................................................. 4 2. Legal control of benzodiazepines .......................................................................................... 4 3. Benzodiazepine chemistry and pharmacology .................................................................. 6 4. Benzodiazepine misuse............................................................................................................ 7 Benzodiazepine use with opioids ................................................................................................... 9 Social harms of benzodiazepine use .......................................................................................... 10 Suicide ............................................................................................................................................. 11 5. Prevalence and harm summaries of Novel Benzodiazepines ...................................... 11 1. Flualprazolam ......................................................................................................................... 11 2. Norfludiazepam ....................................................................................................................... 13 3. Flunitrazolam .......................................................................................................................... -

Chloral Hydrate: Summary Report
Chloral Hydrate: Summary Report Item Type Report Authors Yuen, Melissa V.; Gianturco, Stephanie L.; Pavlech, Laura L.; Storm, Kathena D.; Yoon, SeJeong; Mattingly, Ashlee N. Publication Date 2020-02 Keywords Compounding; Food, Drug, and Cosmetic Act, Section 503B; Food and Drug Administration; Outsourcing facility; Drug compounding; Legislation, Drug; United States Food and Drug Administration; Chloral Hydrate Rights Attribution-NoDerivatives 4.0 International Download date 26/09/2021 09:06:16 Item License http://creativecommons.org/licenses/by-nd/4.0/ Link to Item http://hdl.handle.net/10713/12087 Summary Report Chloral Hydrate Prepared for: Food and Drug Administration Clinical use of bulk drug substances nominated for inclusion on the 503B Bulks List Grant number: 2U01FD005946 Prepared by: University of Maryland Center of Excellence in Regulatory Science and Innovation (M-CERSI) University of Maryland School of Pharmacy February 2020 This report was supported by the Food and Drug Administration (FDA) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award (U01FD005946) totaling $2,342,364, with 100 percent funded by the FDA/HHS. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement by, the FDA/HHS or the U.S. Government. 1 Table of Contents REVIEW OF NOMINATION ..................................................................................................... 4 METHODOLOGY ................................................................................................................... -

Study Protocol Use of Benzodiazepines and Risk of Hip/Femur Fracture a Methodological Comparison Across Data Sources and Epidemiological Design
WP2 Framework for pharmacoepidemiological studies WG1 Databases Study Protocol Use of benzodiazepines and risk of hip/femur fracture A methodological comparison across data sources and epidemiological design Version: Final Nov 14, 2011 with Amendment 1 – Jan 2012, approved 29 Feb 2012 Version: Final Nov 14 2011 with Amendment 2 - Jan 2013, approved 31 December 2013 Version: Final Nov 14 2011 with Amendment 3 – Jun 2013, approved 31 December 2013 Version: Final Nov 14 2011 with Amendment 4 – Oct 2013, approved 31 December 2013 PROTECT_WP2 Final Protocol_BenzoHIPfracture_14Nov2011_Amend 4_Dec 2013 Page 1 of 193 WG1 Drug AE group Name Role Francisco de Abajo 1, 2 Protocol Lead Luis Alberto García Rodríguez 3 Protocol Backup Ulrik Hesse 4 Protocol Reviewer Andrew Bate 5 Protocol Reviewer Saga Johanson 6 Protocol Reviewer Frank de Vries 7 Protocol Reviewer Marietta Rottenkolber 8 Database 1 (Bavaria) lead Joerg Hasford 8 Database 1 (Bavaria) backup Consuelo Huerta 2 Database 2 (Bifap) lead Miguel Gil 2 Database 2 (Bifap) backup Ulrik Hesse4 Database 3 (DKMA) lead Frank de Vries7 Database 3 (DKMA) backup Montserrat Miret 11 and Jeane Pimienta 12 Database 3 (CPRD) lead Arlene Gallagher/ Dan Dedman /Jenny Campbell 13 Database 3 (CPRD) backup Olaf Klungel 7 Database 4 (Mondriaan) lead Liset van Dijk 7, 9 Database 4 (Mondriaan) backup Yolanda Alvarez 10 Database 5 (THIN) lead Ana Ruigomez 3 Database 5 (THIN) backup 1 Universidad de Alcalá, Madrid, Spain 2 Agencia Española de Medicamentos y Productos Sanitarios, Madrid, Spain (AEMPS) 3 Fundación -
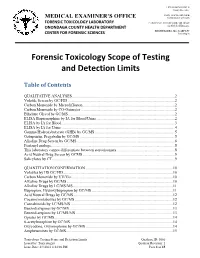
Forensic Toxicology Scope of Testing and Detection Limits
J. RYAN MCMAHON II County Executive INDU GUPTA, MD, MPH MEDICAL EXAMINER’S OFFICE Commissioner of Health FORENSIC TOXICOLOGY LABORATORY CAROLYN H. REVERCOMB, MD, DABP ONONDAGA COUNTY HEALTH DEPARTMENT Chief Medical Examiner KRISTIE BARBA, MS, D-ABFT-FT CENTER FOR FORENSIC SCIENCES Toxicologist Forensic Toxicology Scope of Testing and Detection Limits Table of Contents QUALITATIVE ANALYSES.........................................................................................................2 Volatile Screen by GC/FID .............................................................................................................2 Carbon Monoxide by Microdiffusion..............................................................................................2 Carbon Monoxide by CO-Oximeter ................................................................................................2 Ethylene Glycol by GC/MS.............................................................................................................2 ELISA Buprenorphine by IA for Blood/Urine ................................................................................2 ELISA by IA for Blood ...................................................................................................................3 ELISA by IA for Urine....................................................................................................................4 Gamma Hydroxybutyrate (GHB) by GC/MS..................................................................................5 Gabapentin, -

Drug-Facilitated Sexual Assault in the U.S
The author(s) shown below used Federal funds provided by the U.S. Department of Justice and prepared the following final report: Document Title: Estimate of the Incidence of Drug-Facilitated Sexual Assault in the U.S. Document No.: 212000 Date Received: November 2005 Award Number: 2000-RB-CX-K003 This report has not been published by the U.S. Department of Justice. To provide better customer service, NCJRS has made this Federally- funded grant final report available electronically in addition to traditional paper copies. Opinions or points of view expressed are those of the author(s) and do not necessarily reflect the official position or policies of the U.S. Department of Justice. AWARD NUMBER 2000-RB-CX-K003 ESTIMATE OF THE INCIDENCE OF DRUG-FACILITATED SEXUAL ASSAULT IN THE U.S. FINAL REPORT Report prepared by: Adam Negrusz, Ph.D. Matthew Juhascik, Ph.D. R.E. Gaensslen, Ph.D. Draft report: March 23, 2005 Final report: June 2, 2005 Forensic Sciences Department of Biopharmaceutical Sciences (M/C 865) College of Pharmacy University of Illinois at Chicago 833 South Wood Street Chicago, IL 60612 ABSTRACT The term drug-facilitated sexual assault (DFSA) has been recently coined to describe victims who were given a drug by an assailant and subsequently sexually assaulted. Previous studies that have attempted to determine the prevalence of drugs in sexual assault complainants have had serious biases. This research was designed to better estimate the rate of DFSA and to examine the social aspects surrounding it. Four clinics were provided with sexual assault kits and asked to enroll sexual assault complainants. -

Medication Guide Flurazepam Hydrochloride Capsules
Medication Guide Flurazepam Hydrochloride Capsules, USP (flur az' e pam hye" droe klor' ide) What is the most important information I should know about flurazepam hydrochloride capsules? • Flurazepam hydrochloride capsules are a benzodiazepine medicine. Taking benzodiazepines with opioid medicines, alcohol, or other central nervous system depressants (including street drugs) can cause severe drowsiness, breathing problems (respiratory depression), coma and death. • Flurazepam hydrochloride capsules may cause serious side effects that you may not know are happening to you. These side effects include: • sleepiness during the day • not thinking clearly • act strangely, confused, or upset • “sleep-walking” or doing other activities when you are asleep like: o eating o talking o having sex o driving a car Call your healthcare provider right away if you find out that you have done any of the above activities after taking flurazepam hydrochloride capsules. • Do not take flurazepam hydrochloride capsules unless you are able to stay in bed a full night (7 to 8 hours) before you must be active again. • Do not take more flurazepam hydrochloride capsules than prescribed. What are flurazepam hydrochloride capsules? • Flurazepam hydrochloride capsules are a prescription medicine used to treat certain types of insomnia including difficulty falling asleep, waking up often during the night, or waking up early in the morning. • Flurazepam hydrochloride is a federal controlled substance (C-IV) because it can be abused or lead to dependence. Keep in a safe place to prevent misuse and abuse. Selling or giving away flurazepam hydrochloride capsules may harm others, and is against the law. Tell your healthcare provider if you have ever abused or been dependent on alcohol, prescription medicines or street drugs. -

Harmonized Tariff Schedule of the United States (2020) Revision 7 Annotated for Statistical Reporting Purposes
Harmonized Tariff Schedule of the United States (2020) Revision 7 Annotated for Statistical Reporting Purposes CHAPTER 29 ORGANIC CHEMICALS VI 29-1 Notes 1. Except where the context otherwise requires, the headings of this chapter apply only to: (a) Separate chemically defined organic compounds, whether or not containing impurities; (b) Mixtures of two or more isomers of the same organic compound (whether or not containing impurities), except mixtures of acyclic hydrocarbon isomers (other than stereoisomers), whether or not saturated (chapter 27); (c) The products of headings 2936 to 2939 or the sugar ethers, sugar acetals and sugar esters, and their salts, of heading 2940, or the products of heading 2941, whether or not chemically defined; (d) Products mentioned in (a), (b) or (c) above dissolved in water; (e) Products mentioned in (a), (b) or (c) above dissolved in other solvents provided that the solution constitutes a normal and necessary method of putting up these products adopted solely for reasons of safety or for transport and that the solvent does not render the product particularly suitable for specific use rather than for general use; (f) The products mentioned in (a), (b), (c), (d) or (e) above with an added stabilizer (including an anticaking agent) necessary for their preservation or transport; (g) The products mentioned in (a), (b), (c), (d), (e) or (f) above with an added antidusting agent or a coloring or odoriferous substance added to facilitate their identification or for safety reasons, provided that the additions do not render the product particularly suitable for specific use rather than for general use; (h) The following products, diluted to standard strengths, for the production of azo dyes: diazonium salts, couplers used for these salts and diazotizable amines and their salts.