Benzodiazepine and Z-Drug Safety Guideline
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diazepam - Alcohol Withdrawal
Diazepam - alcohol withdrawal Why have I been prescribed diazepam? If a person stops drinking alcohol after a time of drinking too much they can experience withdrawal effects. These include “the shakes”, sweating, having fits, seeing things which are not there (hallucinations) and feeling anxious and low in mood. They can feel wound up and find it difficult to sleep. These withdrawal effects can be very uncomfortable and in extreme cases can be dangerous if they persist into “DTs” (delirium tremens). Diazepam is used to help reduce these withdrawal symptoms. It relieves anxiety and tension and aids sleep. Diazepam can also prevent fits. It controls the withdrawal symptoms until the body is free of alcohol and has settled down. This usually takes three to seven days from the time you stop drinking. What exactly is diazepam? Diazepam is a benzodiazepine. This group of medicines is also called anxiolytics or minor tranquillisers. Diazepam has many uses. It can be used to reduce symptoms of anxiety and insomnia, as well as to help people come off alcohol. Diazepam should only be prescribed and taken as a short course. Is diazepam safe to take? Diazepam is safe to take for a short period of time, but it doesn’t suit everyone. Below are a few conditions where diazepam may be less suitable. If any of these apply to you please tell your doctor or key-worker. If you have depression or a mental illness If you have lung disease or breathing problems, or suffer from liver or kidney trouble If you take any other medicines or drugs, including those on prescription and bought from a chemist If you take illicit drugs bought “on the street” If you are pregnant or breast-feeding What is the usual dose of diazepam? The dose of diazepam will usually be started at 10-20mg four times a day. -
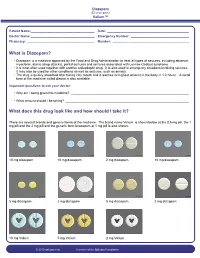
What Is Diazepam?
Diazepam (Di-a-ze-pam) Valium™ Patient Name: ___________________________________ Date: _____________________________________________ Doctor Name: ___________________________________ Emergency Number: ________________________________ Pharmacy: _____________________________________ Number: __________________________________________ What is Diazepam? • Diazepam is a medicine approved by the Food and Drug Administration to treat all types of seizures, including absence, myoclonic, atonic (drop attacks), partial seizures and seizures associated with Lennox-Gastaut syndrome. • It is most often used together with another antiepileptic drug. It is also used in emergency situations involving seizures. It may also be used for other conditions as well as seizures, such as anxiety. • The drug is quickly absorbed after taking it by mouth and it reaches its highest amount in the body in 1-2 hours. A rectal form of the medicine called diastat is also available. Important questions to ask your doctor: • Why am I being given this medicine? _________________________________________________________________ • What amount should I be taking? ____________________________________________________________________ What does this drug look like and how should I take it? There are several brands and generic forms of the medicine. The brand name Valium is shown below at the 0.5 mg pill, the 1 mg pill and the 2 mg pill and the generic form lorazepam at 1 mg pill is also shown. 10 mg diazepam 10 mg diazepam 2 mg diazepam 10 mg diazepam 5 mg diazepam 2 mg diazepam 5 mg diazepam 2 mg diazepam 10 mg Valium 5 mg Valium 2 mg Valium © 2010 epilepsy.com A service of the Epilepsy Foundation Diazepam (Di-a-ze-pam) Valium™ Frequently Asked Questions: How do I take Diazepam? To use the tablet form: chew tablets and swallow or swallow the tablet whole. -

Substance Use Resources for Grades 7-12
1 Substance Use Resources for Grades 7-12 Online Resource Library Search: https://www.voa-dakotas.org/resource-library Addiction: page 1 Alcohol: page 1 Drugs: page 4 Vaping/tobacco: page 10 Addiction Addiction and the Human Brain o DVD, 2006, HRM, 27 minutes, Grades 7-12 o Drug addiction is a disease of the brain and teens are at highest risk for acquiring this disease. This DVD explains the changes to the brain caused by prolonged use of drugs and shows why voluntary drug use eventually becomes involuntary and compulsive. Studies indicate that drugs affect the developing brain more than the brain of someone more mature, thus putting teens at a higher risk of addiction. Interviews with recovering teen addicts, an addiction counselor, and brain experts and researchers provide sobering considerations to viewers. Pre- and Post-tests are included. How Addiction Hijacks the Brain o DVD, 2016, HRM, CC, 24 minutes, Grades 7-College o This film drives home the message that drug and alcohol addiction are a disease of the brain and that teens are at highest risk for acquiring this disease. Leading scientists detail how drugs like heroin, nicotine, cocaine and marijuana change the brain, subvert the way it registers pleasure, and corrupt learning and motivation. Young recovering addicts provide a human face to the effects of drugs and alcohol as they describe how addiction involves intense craving for a drug and loss of control over its use. Viewers also learn that the brain’s plasticity, or ability to change, offers hope for addicts that they can turn their lives around. -

Drug & Alcohol Testing Program
Pottawattmie County Drug & Alcohol Testing Program Appendix A Table of Contents POLICY STATEMENT ...................................................................................................................................... 3 SCOPE ............................................................................................................................................................ 4 EDUCATION AND TRAINING .......................................................................................................................... 4 DESIGNATED EMPLOYER REPRESENTATIVE (DER): ....................................................................................... 5 DUTY TO COOPERATE ................................................................................................................................... 5 EMPLOYEE ADMISSION OF ALCOHOL AND CONTROLLED SUBSTANCE USE: (49 CFR Part 382.121) ... 6 PROHIBITED DRUGS AND ILLEGALLY USED CONTROLLED SUBSTANCES: ..................................................... 7 PROHIBITED BEHAVIOR AND CONDUCT: ...................................................................................................... 8 DRUG & ALCOHOL TESTING REQUIREMENTS (49 CFR, Part 40 & 382) ............................................... 10 DRUG & ALCOHOL TESTING CIRCUMSTANCES (49 CFR Part 40 & 382) .............................................. 12 A. Pre-Employment Testing: .................................................................................................... 12 B. Reasonable Suspicion Testing: ......................................................................................... -

Management of Status Epilepticus
Published online: 2019-11-21 THIEME Review Article 267 Management of Status Epilepticus Ritesh Lamsal1 Navindra R. Bista1 1Department of Anaesthesiology, Tribhuvan University Teaching Address for correspondence Ritesh Lamsal, MD, DM, Department Hospital, Institute of Medicine, Tribhuvan University, Nepal of Anaesthesiology, Tribhuvan University Teaching Hospital, Institute of Medicine, Tribhuvan University,Kathmandu, Nepal (e-mail: [email protected]). J Neuroanaesthesiol Crit Care 2019;6:267–274 Abstract Status epilepticus (SE) is a life-threatening neurologic condition that requires imme- diate assessment and intervention. Over the past few decades, the duration of seizure Keywords required to define status epilepticus has shortened, reflecting the need to start thera- ► convulsive status py without the slightest delay. The focus of this review is on the management of con- epilepticus vulsive and nonconvulsive status epilepticus in critically ill patients. Initial treatment ► neurocritical care of both forms of status epilepticus includes immediate assessment and stabilization, ► nonconvulsive status and administration of rapidly acting benzodiazepine therapy followed by nonbenzodi- epilepticus azepine antiepileptic drug. Refractory and super-refractory status epilepticus (RSE and ► refractory status SRSE) pose a lot of therapeutic problems, necessitating the administration of contin- epilepticus uous infusion of high doses of anesthetic agents, and carry a high risk of debilitating ► status epilepticus morbidity as well as mortality. ► super-refractory sta- tus epilepticus Introduction occur after 30 minutes of seizure activity. However, this working definition did not indicate the need to immediately Status epilepticus (SE) is a medical and neurologic emergency commence treatment and that permanent neuronal injury that requires immediate evaluation and treatment. It is associat- could occur by the time a clinical diagnosis of SE was made. -

2015-16 59. On-Line Learning Bipolar Medications
Pharmacology/Therapeutics II Block II Handouts – 2015‐16 59. On‐Line learning Bipolar Medications ‐ Schilling 60. On‐Line Learning Anti‐Depressants ‐ Schilling 61. On‐Line Learning Sedative Hypnotics ‐ Battaglia 62. On‐Line Learning Treatment of Insomnia ‐ Battaglia 63. On‐Line Learning AntiPsychotics ‐ Schilling 64. On‐Line Only Drugs of Abuse, tolerance & Dependence – Bakowska 65. Active Learning Session: Mood Disorders & Treatment – Schilling 66. Active Learning Session – Anxiety Disorders – Schilling 67. Active Learning Session – Psychotic Illness & Treatment – Schilling 68. Drugs to Treat Rheumatoid Arthritis & Gout ‐ Clipstone Pharmacology & Therapeutics Bipolar Medications February 15, 2016 David Schilling, M.D. Bipolar Disorder Medications Goals & Objectives: Describe the pharmacologic profiles of major drugs/drug classes used in the treatment of bipolar disorder. These drugs include: Lithium, Divalproex (Depakote), Carbamazepine (Tegretol), Lamotrigine (Lamictal) 1. List the major drugs/drug classes used in the treatment of bipolar disorder 2. Describe the mechanism of action of each of the major drugs/drug classes used in the treatment of bipolar disorder 3. Describe the principle pharmacokinetic properties of the major drugs used to treat bipolar disorder. This includes: half-life & time to steady state, trough levels, metabolic auto-induction, P450 system induction, therapeutic index 4. Describe the pharmacodynamics (common adverse effects) of the major drugs used to treat bipolar disorder. 5. Describe the pharmacodynamics (serious adverse effects) of the major drugs used to treat bipolar disorder. This includes: lithium toxicity, agranulocytosis, aplastic anemia, hepatic failure, exfoliative dermatitis, pancreatitis, Steven’s Johnson syndrome 6. Identify the laboratory tests that may be used to monitor for common and serious major adverse effects of the major drugs used to treat bipolar disorder. -

Neonatal Drug Withdrawal Abstract
Guidance for the Clinician in Rendering Pediatric Care CLINICAL REPORT Neonatal Drug Withdrawal Mark L. Hudak, MD, Rosemarie C. Tan, MD,, PhD, THE abstract COMMITTEE ON DRUGS, and THE COMMITTEE ON FETUS AND Maternal use of certain drugs during pregnancy can result in transient NEWBORN neonatal signs consistent with withdrawal or acute toxicity or cause KEY WORDS opioid, methadone, heroin, fentanyl, benzodiazepine, cocaine, sustained signs consistent with a lasting drug effect. In addition, hos- methamphetamine, SSRI, drug withdrawal, neonate, abstinence pitalized infants who are treated with opioids or benzodiazepines to syndrome provide analgesia or sedation may be at risk for manifesting signs ABBREVIATIONS of withdrawal. This statement updates information about the clinical CNS—central nervous system — presentation of infants exposed to intrauterine drugs and the thera- DTO diluted tincture of opium ECMO—extracorporeal membrane oxygenation peutic options for treatment of withdrawal and is expanded to include FDA—Food and Drug Administration evidence-based approaches to the management of the hospitalized in- 5-HIAA—5-hydroxyindoleacetic acid fant who requires weaning from analgesics or sedatives. Pediatrics ICD-9—International Classification of Diseases, Ninth Revision — – NAS neonatal abstinence syndrome 2012;129:e540 e560 SSRI—selective serotonin reuptake inhibitor INTRODUCTION This document is copyrighted and is property of the American fi Academy of Pediatrics and its Board of Directors. All authors Use and abuse of drugs, alcohol, and tobacco contribute signi cantly have filed conflict of interest statements with the American to the health burden of society. The 2009 National Survey on Drug Use Academy of Pediatrics. Any conflicts have been resolved through and Health reported that recent (within the past month) use of illicit a process approved by the Board of Directors. -

Drug and Alcohol Withdrawal Clinical Practice Guidelines - NSW
Guideline Drug and Alcohol Withdrawal Clinical Practice Guidelines - NSW Summary To provide the most up-to-date knowledge and current level of best practice for the treatment of withdrawal from alcohol and other drugs such as heroin, and other opioids, benzodiazepines, cannabis and psychostimulants. Document type Guideline Document number GL2008_011 Publication date 04 July 2008 Author branch Centre for Alcohol and Other Drugs Branch contact (02) 9424 5938 Review date 18 April 2018 Policy manual Not applicable File number 04/2766 Previous reference N/A Status Active Functional group Clinical/Patient Services - Pharmaceutical, Medical Treatment Population Health - Pharmaceutical Applies to Area Health Services/Chief Executive Governed Statutory Health Corporation, Board Governed Statutory Health Corporations, Affiliated Health Organisations, Affiliated Health Organisations - Declared Distributed to Public Health System, Ministry of Health, Public Hospitals Audience All groups of health care workers;particularly prescribers of opioid treatments Secretary, NSW Health Guideline Ministry of Health, NSW 73 Miller Street North Sydney NSW 2060 Locked Mail Bag 961 North Sydney NSW 2059 Telephone (02) 9391 9000 Fax (02) 9391 9101 http://www.health.nsw.gov.au/policies/ space space Drug and Alcohol Withdrawal Clinical Practice Guidelines - NSW space Document Number GL2008_011 Publication date 04-Jul-2008 Functional Sub group Clinical/ Patient Services - Pharmaceutical Clinical/ Patient Services - Medical Treatment Population Health - Pharmaceutical -

Understanding Benzodiazephine Use, Abuse, and Detection
Siemens Healthcare Diagnostics, the leading clinical diagnostics company, is committed to providing clinicians with the vital information they need for the accurate diagnosis, treatment and monitoring of patients. Our comprehensive portfolio of performance-driven systems, unmatched menu offering and IT solutions, in conjunction with highly responsive service, is designed to streamline workflow, enhance operational efficiency and support improved patient care. Syva, EMIT, EMIT II, EMIT d.a.u., and all associated marks are trademarks of General Siemens Healthcare Diagnostics Inc. All Drugs other trademarks and brands are the Global Division property of their respective owners. of Abuse Siemens Healthcare Product availability may vary from Diagnostics Inc. country to country and is subject 1717 Deerfield Road to varying regulatory requirements. Deerfield, IL 60015-0778 Please contact your local USA representative for availability. www.siemens.com/diagnostics Siemens Global Headquarters Global Siemens Healthcare Headquarters Siemens AG Understanding Wittelsbacherplatz 2 Siemens AG 80333 Muenchen Healthcare Sector Germany Henkestrasse 127 Benzodiazephine Use, 91052 Erlangen Germany Abuse, and Detection Telephone: +49 9131 84 - 0 www.siemens.com/healthcare www.usa.siemens.com/diagnostics Answers for life. Order No. A91DX-0701526-UC1-4A00 | Printed in USA | © 2009 Siemens Healthcare Diagnostics Inc. Syva has been R1 R2 a leading developer N and manufacturer of AB R3 X N drugs-of-abuse tests R4 for more than 30 years. R2 C Now part of Siemens Healthcare ® Diagnostics, Syva boasts a long and Benzodiazepines have as their basic chemical structure successful track record in drugs-of-abuse a benzene ring fused to a seven-membered diazepine ring. testing, and leads the industry in the All important benzodiazepines contain a 5-aryl substituent ring (ring C) and a 1,4–diazepine ring. -

Risk Based Requirements for Medicines Handling
Risk based requirements for medicines handling Including requirements for Schedule 4 Restricted medicines Contents 1. Introduction 2 2. Summary of roles and responsibilities 3 3. Schedule 4 Restricted medicines 4 4. Medicines acquisition 4 5. Storage of medicines, including control of access to storage 4 5.1. Staff access to medicines storage areas 5 5.2. Storage of S4R medicines 5 5.3. Storage of S4R medicines for medical emergencies 6 5.4. Access to storage for S4R and S8 medicines 6 5.5. Pharmacy Department access, including after hours 7 5.6. After-hours access to S8 medicines in the Pharmacy Department 7 5.7. Storage of nitrous oxide 8 5.8. Management of patients’ own medicines 8 6. Distribution of medicines 9 6.1. Distribution outside Pharmacy Department operating hours 10 6.2. Distribution of S4R and S8 medicines 10 7. Administration of medicines to patients 11 7.1. Self-administration of scheduled medicines by patients 11 7.2. Administration of S8 medicines 11 8. Supply of medicines to patients 12 8.1. Supply of scheduled medicines to patients by health professionals other than pharmacists 12 9. Record keeping 13 9.1. General record keeping requirements for S4R medicines 13 9.2. Management of the distribution and archiving of S8 registers 14 9.3. Inventories of S4R medicines 14 9.4. Inventories of S8 medicines 15 10. Destruction and discards of S4R and S8 medicines 15 11. Management of oral liquid S4R and S8 medicines 16 12. Cannabis based products 17 13. Management of opioid pharmacotherapy 18 14. -

Benzodiazepines
Benzodiazepines Using benzodiazepines in Children and Adolescents Overview Benzodiazepines are group of medications used to treat several different conditions. Some examples of these medications include: lorazepam (Ativan®); clonazepam (Rivotril®); alprazolam (Xanax®) and oxazepam (Serax®). Other benzodiazepine medications are available, but are less commonly used in children and adolescents. What are benzodiazepines used for? Benzodiazepines may be used for the following conditions: • anxiety disorders: generalized anxiety disorder; social anxiety disorder; post-traumatic stress disorder (PTSD); panic attacks/disorder; excessive anxiety prior to surgery • sleep disorders: trouble sleeping (insomnia); waking up suddenly with great fear (night terrors); sleepwalking • seizure disorders (epilepsy) • alcohol withdrawal • treatment of periods of extreme slowing or excessive purposeless motor activity (catatonia) Your doctor may be using this medication for another reason. If you are unclear why this medication is being prescribed, please ask your doctor. How do benzodiazepines work? Benzodiazepines works by affecting the activity of the brain chemical (neurotransmitter) called GABA. By enhancing the action of GABA, benzodiazepines have a calming effect on parts of the brain that are too excitable. This in turn helps to manage anxiety, insomnia, and seizure disorders. How well do benzodiazepines work in children and adolescents? When used to treat anxiety disorders, benzodiazepines decrease symptoms such as nervousness, fear, and excessive worrying. Benzodiazepines may also help with the physical symptoms of anxiety, including fast or strong heart beat, trouble breathing, dizziness, shakiness, sweating, and restlessness. Typically, benzodiazepines are prescribed to manage anxiety symptoms that are uncomfortable, frightening or interfere with daily activities for a short period of time before conventional anti-anxiety treatments like cognitive-behavioural therapy or anti-anxiety takes effect. -

XANAX® Alprazolam Tablets, USP
XANAX® alprazolam tablets, USP CIV WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death [see Warnings, Drug Interactions]. Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation. DESCRIPTION XANAX Tablets contain alprazolam which is a triazolo analog of the 1,4 benzodiazepine class of central nervous system-active compounds. The chemical name of alprazolam is 8-Chloro-1-methyl-6-phenyl-4H-s-triazolo [4,3-α] [1,4] benzodiazepine. The structural formula is represented to the right: Alprazolam is a white crystalline powder, which is soluble in methanol or ethanol but which has no appreciable solubility in water at physiological pH. Each XANAX Tablet, for oral administration, contains 0.25, 0.5, 1 or 2 mg of alprazolam. XANAX Tablets, 2 mg, are multi-scored and may be divided as shown below: 1 Reference ID: 4029640 Inactive ingredients: Cellulose, corn starch, docusate sodium, lactose, magnesium stearate, silicon dioxide and sodium benzoate. In addition, the 0.5 mg tablet contains FD&C Yellow No. 6 and the 1 mg tablet contains FD&C Blue No. 2. CLINICAL PHARMACOLOGY Pharmacodynamics CNS agents of the 1,4 benzodiazepine class presumably exert their effects by binding at stereo specific receptors at several sites within the central nervous system. Their exact mechanism of action is unknown. Clinically, all benzodiazepines cause a dose-related central nervous system depressant activity varying from mild impairment of task performance to hypnosis.