Community 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

What Is on the Other Side of the Tracks? a Spatial Examination of Neighborhood Boundaries and Segregation
University of Pennsylvania ScholarlyCommons Publicly Accessible Penn Dissertations 1-1-2012 What is on the Other Side of the Tracks? A Spatial Examination of Neighborhood Boundaries and Segregation Rory Kramer University of Pennsylvania, [email protected] Follow this and additional works at: http://repository.upenn.edu/edissertations Part of the African American Studies Commons, Geography Commons, and the Sociology Commons Recommended Citation Kramer, Rory, "What is on the Other Side of the Tracks? A Spatial Examination of Neighborhood Boundaries and Segregation" (2012). Publicly Accessible Penn Dissertations. 532. http://repository.upenn.edu/edissertations/532 This paper is posted at ScholarlyCommons. http://repository.upenn.edu/edissertations/532 For more information, please contact [email protected]. What is on the Other Side of the Tracks? A Spatial Examination of Neighborhood Boundaries and Segregation Abstract Space has always been a critical component of the sociological study of racial inequality, yet it has rarely been the central focus of empirical projects. Studies of segregation, an inherently spatial concept, have relied on techniques that are aspatial introduce an unknown amount of error into their results. This project extends standard spatial analytic techniques to the sociological study of racial segregation, using Philadelphia as its case study. By introducing non-euclidean kernel density analysis to the study of racial segregation, the project explores how a more visual and more spatially informed -

©2019 Spencer T. Clayton ALL RIGHTS RESERVED
©2019 Spencer T. Clayton ALL RIGHTS RESERVED TAX ABATEMENTS AND GENTRIFICATION: HOW GOVERNMENT POLICY DISRUPTS COMMUNITIES by SPENCER T. CLAYTON A dissertation submitted to the Graduate School-Camden Rutgers, the State University of New Jersey In partial fulfillment of the requirements For the degree of Doctor of Philosophy Graduate Program in Public Affairs Written under the direction of Richard A. Harris, Ph.D. And approved by ____________________________________ Richard A. Harris, Ph.D., Committee Chair ____________________________________ Paul Jargowsky, Ph.D. ____________________________________ Lorraine C. Minnite, Ph.D. ____________________________________ Adam Okulicz-Kozaryn, Ph.D. Camden, New Jersey May 2019 ABSTRACT OF DISSERTATION Tax Abatements and Gentrification: How Government Policy Disrupts Communities by SPENCER T. CLAYTON Dissertation Director: Richard A. Harris, Ph.D. Urban municipal governments often face challenges when redeveloping their distressed centers. In 2000, the City Council of Philadelphia passed a series of bills modifying its existing residential tax abatement policies to expand their eligibility and to make them last for ten years. The timing of the passage of these bills also corresponded with Mayor John Street’s Neighborhood Transformation Initiative (NTI), which aimed to prepare land for redevelopment. The combination of the revised abatement policies and NTI created a series of competing interests for politicians, business owners, and community organizations. Utilizing a methodological design consisting a historical critical analysis based on urban regime theory, GIS, and regression analysis, this dissertation profiles the formulation, implementation, and impact of Philadelphia’s tax abatement policies from 2000 to 2010. It also proposes a mechanism by which government policies can facilitate or accelerate gentrification. Results show support for a relationship between the incidence of tax abatements and gentrification. -

Seed Award Grant
PHILADELPHIA AUTISM PROJECT SEED AWARD GRANT 2021 Philadelphia Autism Project Seed Award Recipients The Philadelphia Autism Project is excited to announce the 2020-2021 seed award recipients. Please see below for group descriptions. Feel free to contact recipients directly to get involved. To learn more about all seed award groups, please visit: www.phillyautismproject.org/seed WHERE ARE THE PROJECTS? FAR NORTHEAST PHILADELPHIA Autism Friendly Environment GERMANTOWN/ Creative Arts CHESTNUT HILL OLNEY/ OAK LANE NORTHEAST Family Focused PHILADELPHIA Events ROXBOROUGH/ MANAYUNK UPPER NORTH PHILADELPHIA Life Skills LOWER NORTH KENSINGTON WEST PHILADELPHIA PHILADELPHIA Recreation CENTER CITY Social Skills SOUTH Support Group PHILADELPHIA SOUTHWEST Workshops/ PHILADELPHIA Training Efforts ADVOCATE FOR ME - MOMS NIGHT OUT Autism Mom’s Night Out is an event which honors mothers of children diagnosed on the autism spectrum. Contact: L’Vonne McMillen @AdvocateforMe1 Email: [email protected] Group: Moms Educating to Thrive On! Phone: 267.265.7792 @lvonne_mcmillan_advocateforme Website: lmadvocateforme.com Region Served: Southwest Philadelphia, South Philadelphia, West Philadelphia, North Philadelphia, Near Northeast Philadelphia, Far Northeast Philadelphia, Olney/Oak Lane ASCEND GROUP INC. - VIRTUAL PARENT SUPPORT GROUP The ASCEND Group provides monthly meetings for up to 20 parents with children with autism. Includes a licensed marriage and family therapist. Includes tools that help focus on behavior modification, building on existing strengths, reducing isolation, self-care, and maintaining positivity. Contact: Elena Perri Email: [email protected] @AscendPhilly Phone: 610-449-6776 @AscendGroupPhilly Website: ascendgroup.org @ascendgroup Region Served: Greater Philadelphia Area SIGN LANGUAGE FOR AUTISM Sign Language for Autism provides sign language workshops for children and their families. Sign language holds a unique promise for every child on the autism spectrum. -

Housing Markets and Social Capital: the Role of Participation, Institutions, and Diversity in Neighborhood Transformation
University of Pennsylvania ScholarlyCommons Culture Builds Community Culture Builds Community Evaluation—1997-2002 6-2001 Housing Markets and Social Capital: The Role of Participation, Institutions, and Diversity in Neighborhood Transformation Mark J. Stern University of Pennsylvania, [email protected] Follow this and additional works at: https://repository.upenn.edu/siap_culture_builds_community Part of the Arts and Humanities Commons, Social Policy Commons, Sociology Commons, and the Urban Studies and Planning Commons Stern, Mark J., "Housing Markets and Social Capital: The Role of Participation, Institutions, and Diversity in Neighborhood Transformation" (2001). Culture Builds Community. 14. https://repository.upenn.edu/siap_culture_builds_community/14 The release of the John Street administration’s Neighborhood Transformation Initiative (NTI) in April 2001 marked a bold step by city government and the private sector to address the long-term problems of economic and social decline in the city of Philadelphia. The plan called for a differentiated strategy of public-private partnership with the goal of reinvigorating housing markets throughout the city. According to the NTI housing market analysis, more than four out of five Philadelphians lived in the bottom three market clusters—transitional, distressed, and reclamation. SIAP's Culture Builds Community inquiry was undertaken from 1996 to 2001 with support by the William Penn Foundation. This paper is posted at ScholarlyCommons. https://repository.upenn.edu/siap_culture_builds_community/14 For more information, please contact [email protected]. Housing Markets and Social Capital: The Role of Participation, Institutions, and Diversity in Neighborhood Transformation Abstract This paper examines the housing markets described in the Philadelphia Neighborhood Transformation Initiative (NTI), launched by Mayor John Street in April 2001, through the lens of social capital indicators. -
Community 2019
Southeastern Pennsylvania Community 2019 SOUTHEASTERN PENNSYLVANIA SOUTHEASTERN PENNSYLVANIA HEALTH NEEDS ASSESSMENT Partnering Hospitals • Abington Hospital • Abington Lansdale Hospital • Chester County Hospital • Children’s Hospital of Philadelphia • Einstein Medical Center Montgomery NEEDS ASSESSMENT HEALTH COMMUNITY • Einstein Medical Center Philadelphia • Einstein Medical Center Elkins Park • Grand View Hospital • Holy Redeemer Hospital • Jefferson Bucks Hospital • Jefferson Frankford Hospital • Jefferson Torresdale Hospital • Thomas Jefferson University Hospital • Jefferson Hospital for Neuroscience • Jefferson Methodist Hospital • Hospital of the University of Pennsylvania • Pennsylvania Hospital • Penn Presbyterian Medical Center TABLE OF CONTENTS Executive Summary ........................................2 Philadelphia County, PA ..................................127 1. Center City .........................................................128 Partners ....................................................13 2. Far North Philadelphia ......................................130 1. Introduction .......................................................13 3. Far Northeast Philadelphia ...............................134 2. Participating Hospitals and Health Systems ....14 4. Lower Northeast Philadelphia ...........................138 a. Hospital Profiles 5. North Philadelphia – East .................................142 i. Overview of Hospital 6. North Philadelphia – West ................................146 ii. Past CHNA and Community 7. Northwest -

School Desegregation, the Philadelphia Experience
DOCUMENT RESUME ED 103 546 UD 014 920 AUTHOR Herron, William P. TITLE School Desegregation, the Philadelphia Experience. PUB DATE 75 NOTE 33p.; Paper presented at the Annual Meeting of the American Educational Association (Washington, D.C., March 1975) EDRS PRICE MF-$0.76 HC-$1.95 PLUS POSTAGE DESCRIPTORS Bus Transportation; Educational Policy; Integration Litigation; *Integration Methods; *Integration Plans; Integration Studies; Public Policy; Public Schools; Racial Integration; School Districts; *School Integration; Student Transportation; Transfer Programs; *Urban Schools IDENTIFIERS Pennsylvania; *Philadelphia ABSTRACT The Philadelphia experience very strongly indicates that at least in Philadelphia, and very probably in most large cities in the northeastern U.S., several factors--notably the geographic separation of the races within the city and the existence of a sizable non-public school system (Usually (Usually parochial)--preclude the effective desegregation of the public schools without large scale busing of the pupils or without some kind of mixing of white suburban populations with black central city populations. Thus, those who espouse the use of desegregation tools such as changing feeder areas, pairing adjacent schools, and offering voluntary magnet programs at particular locations to achieve racial balance in the public schools of such cities may well be deluding themselves. As of mid-February 1975, the Pennsylvania Human Relations Commission is attempting to develop a desegregation plan for the Philadelphia schools. At the same time, the school district staff committee is also preparing a plan which will contain several elements from previews plans as well as the 'Academy' concept. The situation at the present time represents a significant departure in that this is the first time that the Commission has been ordered to prepare a plan. -

Philadelphia Housing Authority
THE PHILLY PRIMER: Housing Resources for People with Disabilities WINTER 2009 THE PHILLY PRIMER: Housing Resources for People with Disabilities Fourth Printing — December 2009 A Publication of the Technical Assistance Program (TAP) Written by: Maggie B. McCullough, MBMconsulting Revised by: Diana T. Myers and Associates, Inc. Edited by: Diana Myers, Diana T. Myers and Associates, Inc. Diana T. Myers and Associates, Inc. 6 South Easton Road, Glenside, PA 19038 This publication was funded by the City of Philadelphia’s Office of Housing and Community Development, and is available online at the TAP website: www.newsontap.org/primer.html. Acknowledgements Information included in this Guide was obtained from a number of organizations, their publications and web sites. The Office of Housing and Community Development wishes to recognize the following organi- zations and resources, in particular, for their invaluable contributions to this Guide: Philadelphia Association of Community Development Corporations (PACDC) Philadelphia Corporation on Aging (PCA) Housing Resources for the Elderly in Philadelphia Philadelphia Housing Authority (PHA) Pennsylvania Housing Finance Agency (PHFA) Pennsylvania Department of Public Welfare, Office of Mental Health and Substance Abuse Services Compendium of Housing Programs in Pennsylvania Self-Determination Housing Project of Pennsylvania My Own Keys CHOICES: A Housing Resource Guide Homeownership Training Program for People with Disabilities TAIG Development Services Corporation and Liberty Resources, Inc. The Philadelphia Homeownership Demonstration Project for Persons with Disabilities U.S. Department of Housing and Urban Development (HUD) Diana T. Myers and Associates would also like to thank the people who reviewed draft versions of this guide to ensure that all of the information provided here is up-to-date. -

The Problem of the Ages: Prostitution in the Philadelphia Imagination, 1880-1940
THE PROBLEM OF THE AGES: PROSTITUTION IN THE PHILADELPHIA IMAGINATION, 1880-1940 A Dissertation Submitted to The Temple University Graduate Board in Partial Fulfillment of the Requirements for the Degree DOCTOR OF PHILOSOPHY by James H. Adams May, 2009 ii © by James H. Adams 2009 All Rights Reserved iii ABSTRACT Title: The Problem of the Ages: Prostitution in the Philadelphia Imagination, 1880-1940 Candidates Name: James H. Adams Degree: Doctor of Philosophy Temple University, 2009 Doctoral Advisory Committee Chair: Mark Haller An ever-present figure throughout much of the nineteenth century, the prostitute existed in a state divorced from “traditional” womanhood as a shadowy yet “necessary” evil, and was largely seen as a static element of the city. The archetypes of the “endangered maiden” and the “fallen woman” were discursive creations evolving from an inchoate form to a more sharply defined state that were designed to explain the prostitute’s continued existence despite the moral objections voiced by religious and social reformers. These archetypes functioned in an agrarian/proto-industrial society; however, under pressures of urbanization, industrialization, and population mobility, these archetypes were gradually supplanted by sharper, more emotionally loaded archetypes such as the “White Slave” and the trope of the “Vice Syndicate” to explain the prostitute. In this manner Progressive-Era social and moral reformers could interpret prostitution in general and the prostitute in particular within the framework of their understanding of a contentious social environment. In moving away from a religious framework towards a more scientific interpretation, the concept of prostitution evolved from a moral failing to a status analogous to a disease that infected the social body of the state. -

Philadelphia
A report from March 2016 Katye Martens/The Pew Charitable Trusts Philadelphia: The State of the City A 2016 Update Overview Philadelphia in 2016 is a growing city undergoing a sweeping transformation, most evident in the age and diversity of those who live here. The city’s population has risen for nine consecutive years, up another 5,880 in the most recent count. The increase since 2006 stands at 78,732, a stark reversal after a decrease of nearly 600,000 over the previous five decades. More compelling, though, are some of the factors that underlie the city’s growth. One is age. As the United States has gotten older, Philadelphia has become younger—largely because of the growth of the city’s young adult population, the much-discussed millennials. A decade ago, Philadelphia had a median age of 35.3, only a year below the nation’s 36.4. In the most recent census, the city’s age was down to 33.8, while the national figure had risen to 37.7—a difference of nearly four years. Remarkably, this happened over a time in which the number of children in the city was declining. Philadelphia is again a city of immigrants, as it had been for most of its history—but not for much of the 20th century. As recently as 1990, Philadelphia had barely more than 100,000 foreign-born residents. Today, it has in excess of 200,000, mostly from Asia, Latin America, and the Caribbean, with no single nationality accounting for more than 13 percent of the whole. -

State Transportation Commission 2015 Twelve Year Program Development Regional Results of the Survey and Public Feedback From
State Transportation Commission 2015 Twelve Year Program Development Regional results of the survey and public feedback from August thru November 2013 Delaware Valley Regional Planning Commission (DVRPC) Version 01-2014 Delaware Valley Regional Planning Commission MPO Total Visitors 730 Mobility Concerns Traffic congestion is growing and resources are limited to build additional capacity. As a result, transportation agencies are exploring ways to manage demand, operate efficiently, and improve capacity. Using a scale of 1-5, for each mobility concern, please rank how important each mobility concern is to you, with one being ‘Not Important’ and 5 being ‘Very Important’. Passenger Ridership on the Keystone Corridor has doubled since 2000 making it !mtrak’s fourth-busiest route in the Rail nation. Rail infrastructure improvements are critical to timely service. Responded With an Average Rank of 4.35 Congestion Relieve traffic congestion by addressing bottlenecks and other traffic relief measures. Responded With an Average Rank of 4.26 Transit Implementing new technologies improves service. Responded With an Average Rank of 4.15 Signals Modernization of traffic signals streamlines traffic flow and reduces fuel costs for motorists. Responded With an Average Rank of 4.07 Incident This legislation would allow for the safe, quick clearance of traffic incidents from the roadway. Responded With an Average Rank of 3.59 Freight Rail $500 billion in goods and services travel through PA each year. That investment would grow with upgrades to accommodate intermodal changes such as emerging needs from the natural gas industry and double- stack train access to our ports. Responded With an Average Rank of 3.53 Real T ime This involves the use of dynamic message signs, PennDOT’s 511P!.com system and social media. -
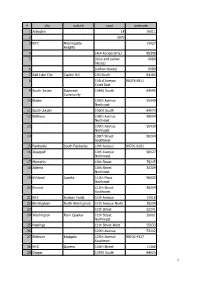
SQL Abfragenergebnis
# city suburb road postcode 1 Arlington 14 76011 2 2870 3 NYC Morningside 10027 Heights 4 (4x4 Access Only) 85396 5 (lbue and yellow 6089 blazes) 6 (yellow blazes) 6089 7 Salt Lake City Capitol Hill 100 South 84180 8 103rd Avenue 98375-9511 Court East 9 South Jordan Daybreak 10460 South 84095 Community 10 Blaine 105th Avenue 55449 Northeast 11 South Jordan 10600 South 84070 12 Bellevue 106th Avenue 98004 Northeast 13 109th Avenue 55434 Northeast 14 109th Street 98204 Southwest 15 Fairbanks South Fairbanks 10th Avenue 99701-6161 16 Issaquah 10th Avenue 98027 Northwest 17 Memphis 10th Street 79245 18 Atlanta 10th Street 30309 Northeast 19 Kirkland Juanita 110th Place 98033 Northeast 20 Everett 112th Street 98204 Southwest 21 NYC Hudson Yards 11th Avenue 10018 22 Birmingham North Birmingham 11th Avenue North 35234 23 11th Street 52241 24 Washington Penn Quarter 11th Street 20001 Northwest 25 Hastings 11th Street West 55033 26 120th Avenue 53142 27 Bellevue Eastgate 125th Avenue 98005-4317 Southeast 28 NYC Queens 126th Street 11368 29 Draper 12970 South 84020 1 # city suburb road postcode 30 NYC Chelsea 12th Avenue 10001 31 Nashville-Davidson East Nashville 12th Avenue South 37203 32 12th Street 54904 33 Marina Marina 13th Street 93933 34 Atlanta Rockdale 13th Street 30309 Northeast 35 NYC Queens 144th Street 11435 36 Cincinnati Over-The-Rhine 14th St 45202 37 Miami Beach 14th Street 33139 38 Washington Columbia Heights 14th Street 20011 Northwest 39 150th Avenue 56073 40 151st Street 60452 41 152nd Street 60445 42 153rd Street East 98360 -

Philadelphia 2021: the State of the City April 2021 About This Report
Philadelphia The the State 2021: of City Report April 2021 April 2021 Philadelphia 2021 The State of the City About this report The annual “State of the City” report is part of The Pew Charitable Trusts’ ongoing work in Philadelphia. Staff members Katie Martin, Jason Hachadorian, and Donna Leong gathered the data and assembled the report. Larry Eichel, senior adviser for Pew’s Philadelphia research and policy initiative, helped write and edit the publication, along with Elizabeth Lowe and Erika Compart. Ned Drummond and Cara Bahniuk created the graphics and designed the report. Contact: Elizabeth Lowe, communications officer Email: [email protected] Phone: 215-575-4812 Project website: pewtrusts.org/philaresearch The Pew Charitable Trusts is driven by the power of knowledge to solve today’s most challenging problems. Pew applies a rigorous, analytical approach to improve public policy, inform the public, and invigorate civic life. Contents 1 A Troubling Year 15 Demographics 27 Education 35 Government 43 Health 57 Housing 69 Jobs and the Economy 81 Public Safety 91 Transportation, Infrastructure, and the Environment 98 Photo Captions A Troubling Year In so many ways, 2020 was a troubling year for Philadelphia, one that raised profound questions about its future. The numbers tell the story of a city facing tremendous challenges, not just from the pandemic and its economic impact but from rising drug overdose deaths and gun violence as well. Philadelphia recorded more than 96,000 COVID-19 cases and 2,500 deaths from the virus in 2020, with the death toll surpassing 3,000 by mid-February 2021.