Community Health Needs Assessment Implementation Plan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

What Is on the Other Side of the Tracks? a Spatial Examination of Neighborhood Boundaries and Segregation
University of Pennsylvania ScholarlyCommons Publicly Accessible Penn Dissertations 1-1-2012 What is on the Other Side of the Tracks? A Spatial Examination of Neighborhood Boundaries and Segregation Rory Kramer University of Pennsylvania, [email protected] Follow this and additional works at: http://repository.upenn.edu/edissertations Part of the African American Studies Commons, Geography Commons, and the Sociology Commons Recommended Citation Kramer, Rory, "What is on the Other Side of the Tracks? A Spatial Examination of Neighborhood Boundaries and Segregation" (2012). Publicly Accessible Penn Dissertations. 532. http://repository.upenn.edu/edissertations/532 This paper is posted at ScholarlyCommons. http://repository.upenn.edu/edissertations/532 For more information, please contact [email protected]. What is on the Other Side of the Tracks? A Spatial Examination of Neighborhood Boundaries and Segregation Abstract Space has always been a critical component of the sociological study of racial inequality, yet it has rarely been the central focus of empirical projects. Studies of segregation, an inherently spatial concept, have relied on techniques that are aspatial introduce an unknown amount of error into their results. This project extends standard spatial analytic techniques to the sociological study of racial segregation, using Philadelphia as its case study. By introducing non-euclidean kernel density analysis to the study of racial segregation, the project explores how a more visual and more spatially informed -

PPC-Infographic.Pdf
Celebrating our 15th anniversary, Partnership for Patient Care (PPC) is the region’s premier patient safety and quality program driving health equity and high quality outcomes. 115th5th Anniversary 2006 – 2021 WHAT IS PARTNERSHIP FOR PATIENT CARE? Partnership for Patient Care (PPC) is a collaboration between Independence Blue Cross, Health Care Improvement Foundation and the region’s leading healthcare organizations and stakeholders to accelerate the adoption of evidence-based clinical best practices. PPC’s improvement efforts have enabled the region to foster partnerships among organizations that share a common desire for providing the safest and highest quality care to patients. PPC serves as an umbrella, under which several programs have been established during the past 15 years to support ongoing regional improvement. PPC PROGRAMS Health Equity Data Strategy (HEDS) NEW New in 2021, HEDS is a regional collaborative aimed at decreasing disparities in health outcomes with a focus on establishing recommendations for the implementation of a health equity data strategy. This program will support organizations in the accurate and reliable collection of REaL (ethnicity, and language) data, utilization of the data to evaluate health outcomes, identification of disparities across populations and health conditions; and implementation of targeted quality improvement strategies that promote health equity. Safety Forum 100% A forum of front-line patient safety leaders from hospitals across Southeastern PA that of participants rated promotes interactive discussions about safety hazards and vulnerabilities and a peer- the program as very good or excellent to-peer exchange of patient safety approaches, processes, and best practices. Pennsylvania Urologic Regional Collaborative (PURC) 142 PURC is a quality improvement initiative that brings urology practices together in a physician- participating physicians led, data-sharing and improvement collaborative aimed at advancing the quality of diagnosis 17,000+ and care for men with prostate cancer. -
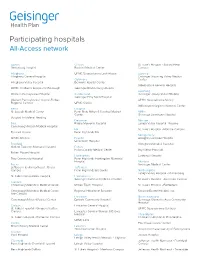
Participating Hospitals All-Access Network
Participating hospitals All-Access network Adams Clinton St. Luke’s Hospital - Sacred Heart Gettysburg Hospital Bucktail Medical Center Campus Allegheny UPMC Susquehanna Lock Haven Luzerne Allegheny General Hospital Geisinger Wyoming Valley Medical Columbia Center Allegheny Valley Hospital Berwick Hospital Center Wilkes-Barre General Hospital UPMC Children’s Hospital of Pittsburgh Geisinger Bloomsburg Hospital Lycoming Western Pennsylvania Hospital Cumberland Geisinger Jersey Shore Hospital Geisinger Holy Spirit Hospital Western Pennsylvania Hospital-Forbes UPMC Susquehanna Muncy Regional Campus UPMC Carlisle Williamsport Regional Medical Center Berks Dauphin St. Joseph Medical Center Penn State Milton S Hershey Medical Mifflin Center Geisinger Lewistown Hospital Surgical Institute of Reading Delaware Monroe Blair Riddle Memorial Hospital Lehigh Valley Hospital - Pocono Conemaugh Nason Medical Hospital Elk St. Luke’s Hospital - Monroe Campus Tyrone Hospital Penn Highlands Elk Montgomery UPMC Altoona Fayette Abington Lansdale Hospital Uniontown Hospital Bradford Abington Memorial Hospital Guthrie Towanda Memorial Hospital Fulton Fulton County Medical Center Bryn Mawr Hospital Robert Packer Hospital Huntingdon Lankenau Hospital Troy Community Hospital Penn Highlands Huntingdon Memorial Hospital Montour Bucks Geisinger Medical Center Jefferson Health Northeast - Bucks Jefferson Campus Penn Highlands Brookville Northampton Lehigh Valley Hospital - Muhlenberg St. Luke's Quakertown Hospital Lackawanna Geisinger Community Medical Center St. Luke’s Hospital - Anderson Campus Cambria Conemaugh Memorial Medical Center Moses Taylor Hospital St. Luke’s Hospital - Bethlehem Conemaugh Memorial Medical Center - Regional Hospital of Scranton Steward Easton Hospital, Inc. Lee Campus Lancaster Northumberland Conemaugh Miners Medical Center Ephrata Community Hospital Geisinger Shamokin Area Community Hospital Carbon Lancaster General Hospital St. Luke’s Hospital - Gnaden Huetten UPMC Susquehanna Sunbury Campus Lancaster General Women & Babies Hospital Philadelphia St. -

Employee Handbook
Employee Handbook You and Jefferson Thomas Jefferson University & Hospitals Stephen K. Klasko, MD, MBA President and CEO Thomas Jefferson University and Jefferson Health System Dear Colleague, Welcome to Thomas Jefferson University and Hospitals! In accepting your new position, you have joined a team committed to redefining healthcare. With a robust history and community roots dating back to 1824, Jefferson is a nationally influential and widely respected academic medical center. We deliver high quality, personalized and compassionate care, and you are now a vital part of our tradition of excellence. By selecting Jefferson, you will enjoy competitive pay, a broad selection of employee benefits from which to choose, opportunity for educational and developmental growth, and a challenging and interactive work environment. Congratulations and my best wishes as you assume your new responsibilities at Jefferson. Sincerely, Stephen K. Klasko, MD, MBA President and CEO Thomas Jefferson University and Jefferson Health System About This Handbook This employee handbook has been designed to provide you with general information about various policies, benefits, services and facilities of Jefferson which may be of interest to you in the course of your employment. Please understand that it only highlights these topics. More specific information may be obtained from your supervisor, the hospital intranet, where any specific policies cited here may be found or the Department of Human Resources at Suite 2150 Gibbon Building or Methodist Administration Suite. You are strongly encouraged to become acquainted with all Jefferson policies and procedures to make your employment as satisfying and productive as possible. The policies, procedures and benefits described in this handbook are not all-inclusive and may be amended or rescinded from time to time at the discretion of Jefferson, with or without notice. -

Resources for Philadelphia Families During Coronavirus (Covid-19)
RESOURCES FOR PHILADELPHIA FAMILIES DURING CORONAVIRUS (COVID-19) Are you pregnant or a parent/caregiver of a young child? We know there is a lot of fear and change right now because of Coronavirus (COVID-19) so we want to share important information about supplies and resources to care for you and your child. Please visit phila.gov/(COVID-19) or call 1-800-722-7112 for more information. Note: Please call organizations first for updated services and hours. Breastfeeding Support Pacify: https://www.pacify.com/ • A FREE mobile app that provides on-demand access to lactation specialists right from your smartphone • Get the “Pacify” app in the Apple Store or Google Play • Enter the enrollment code PHILLY at signup for FREE 24/7 access Breast pumps: You can reach out to your insurance provider to request a breast pump delivered to your home Baby Supplies (Diapers, Formula, and Food) WIC: http://northwic.org/ • Resource: WIC EBT card • Note: Participants will now be seen outside of the office for safety reasons using a new card exchange system. Please call on arrival to the office. WIC has stopped the requirement of infants, children, and/or pregnant women having to come in for their WIC benefits – participants can send someone to come in for them if they tell WIC staff over the phone who will be coming to pick up their benefits and that person needs to bring photo identification. • Sites: − North Philadelphia WIC Office: 215-229-3786, 1300 W Lehigh Ave #104, Phila, PA 19132 − South Philadelphia WIC Office: 215-463-5571, 1165 S Broad St, Phila, -
Restructuring the MLH/Jefferson Partnership
Main Line Health Physician Restructuring the MLH/Jefferson partnership Surviving Sepsis: The future of Hepatology: SUMMER 2014 ED success moves health care at From Hep C to Inside: to inpatient Exton Square Mall transplant care Main Line Health Physician Medical staff education initiative BY ANGUS GILLIS, MD The Main Line Health medical staff structure is an integrated model that encompasses private practice MESSAGES | 2 physicians who are on staff, hospital-employed physicians, and physicians/physician groups who are under contract for provision of services to the Hospital System. Medical staff functions have traditionally included initial credentialing, reappointment, and approval of privileges for new procedures. Tools used to fulfill these tasks include focused and ongoing professional practice evaluation (FPPE and OPPE). The staff is responsible for peer review, including case study and quality concerns. By-law and policy issues such as investigations, interventions, confidentiality, and physician rights are also areas in which the medical staff is involved. The staff has administrative functions related to patient safety, infection control, pharmacy and therapeutics, medical records, and behavioral issues like disruptive behavior and practitioner health. This is only a partial list of the responsibilities of the medical staff. Ultimate responsibility for approval and implementation of any recommendations by the staff’s Medical Executive Committee lies with the Board of Main Line Health. In addition to the above functions, the medical staff also takes an active role in continuing medical education. Your medical staff dues have always funded clinical educational efforts, such as Grand Rounds, at our various locations. A new additional effort is the Medical Executive Committee’s budgeting of dedicated monies for physician education, which will enable members to carry out these medical staff responsibilities. -

Gail Farmer Director of Education
Gail Farmer Director of Education Children spend 1% of their free time outdoors Hofferth, S. and Sandberg, J. ( 1999). Changes in American Children’s Time, 1981-1997, University of Michigan Institute for Social Research. Children spend 7.5 hours per day in front of screens. Rideout, VJ et al. Kaiser Family Foundation Report. 2010 Angora Park 57th St. & Baltimore Ave. Childhood has Retreated Indoors “...we will not fight to save what we do not love” -Stephen Jay Gould Angora Park 57th St. & Baltimore Ave. Childhood has Retreated Indoors Sitting is the New Smoking Diabetes Hypertension Asthma Obesity Depression Vitamin D deficiency Angora Park 57th St. & Baltimore Ave. Childhood has Retreated Indoors Nature Rx Big Goal and Potential Outcomes Nature Rx Big Goal and Potential Outcomes Value of urban Green space Get more Healthy Social Phila families Behaviors Capital active in green spaces Nature connection Nature Rx Systems Thinking Urban planning Environmental Municipalities Orgs Social workers Clinicians Municipalities Urban planning Public health agencies and Health orgs – Social workers social orgs determinants of health Environmental Orgs Nature Rx Strategic Planning & Implementation Stakeholder & Partner Organizations Non-Profit Organizations National Environmental Education Foundation Smith Memorial Playground The Circuit Coalition Philadelphia Play Works Bicycle Coalition of Greater Philadelphia The Workshop School Health Promotion Council Physicians for Social Responsibility Dela. Valley Assoc. for the Education of Young Children -

Hotel Folks Hold Farewell Assembly
The Home Paper For Home News, m il Lest Yon Forget, Remember Between Seasons There’s Nothing The Home Paper With Your Printing Like News of the Grove At First Hands, The Times Gives It. Vol. XXXIII-No. 2 5 , 1 9 2 5 OCEAN GROVE, N. FRIDAY, SEPTEMBER f o u r c e n t s - x f t w t NEPTUNE TOWNSHIP ROADS HOTEL FOLKS HOLD DISCl/SSED BY COMMITTEE TENTATIVE PROGRAM BRANDT LECTURE ON c' T, v o 5 ° - ~ 29. i 14 SOCIAL SERVICE § At the Neptune township committee With Mrs. Laura B. Bimbler, of i FAREWELL ASSEMBLY meeting Tuesday evening, a short ses FOR SEASON OF 1 9 2 6 FUTURE OF AMERICA Bradley Beach, in the chair, the fall j sion, only routine business was trans convention of the . Monmouth C<-unty ! GROUPS ORGANIZED f t acted—reports of committees, pass Woman’s Christian Temperance Jnion — — age of bills, etc; ' BEFORE SEPARATING FOR will be held Tuesday of next week in o n m m T ir p n r a *™-™-. Whim the calendar had been cleared OPENING SUNDAY, JUNE 13; BROADSIDE AGAINST BOOZE the Methodist Protestant church; Avon, “GHEDULE-PLANNED IS FOR IS FALL AND WINTER and Clerk Knox gave way to Auditor CLOSING SEPT. 12 There will be a morning session a t) Reynolds, an informal discussion of SELLING IN JERSEY 10.30, an afternoon session at 2.30 and MONMOUTH COUNTY civic matters drew from Committee £ii evening session at 8.00. Following man Hulshart the statement that the is the program in detail. -
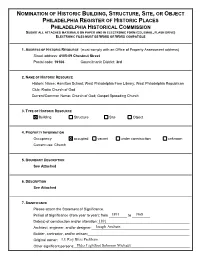
Nomination of Historic Building, Structure, Site, Or
NOMINATION OF HISTORIC BUILDING, STRUCTURE, SITE, OR OBJECT PHILADELPHIA REGISTER OF HISTORIC PLACES PHILADELPHIA HISTORICAL COMMISSION SUBMIT ALL ATTACHED MATERIALS ON PAPER AND IN ELECTRONIC FORM (CD, EMAIL, FLASH DRIVE) ELECTRONIC FILES MUST BE WORD OR WORD COMPATIBLE 1. ADDRESS OF HISTORIC RESOURCE (must comply with an Office of Property Assessment address) Street address: 4105-09 Chestnut Street Postal code: 19106 Councilmanic District: 3rd 2. NAME OF HISTORIC RESOURCE Historic Name: Hamilton School; West Philadelphia Free Library; West Philadelphia Republican Club; Radio Church of God Current/Common Name: Church of God; Gospel Spreading Church 3. TYPE OF HISTORIC RESOURCE Building Structure Site Object 4. PROPERTY INFORMATION Occupancy: occupied vacant under construction unknown Current use: Church 5. BOUNDARY DESCRIPTION See Attached 6. DESCRIPTION See Attached 7. SIGNIFICANCE Please attach the Statement of Significance. Period of Significance (from year to year): from _________1891 to _________1968 Date(s) of construction and/or alteration:_____________________________________1891 _________ Architect, engineer, and/or designer:________________________________________Joseph Anshutz _________ Builder, contractor, and/or artisan:__________________________________________ _________ Original owner:_________________________________________________________LE Roy Bliss Peckham _________ Other significant persons:_________________________________________________Elder Lightfoot Solomon Michaux _________ CRITERIA FOR DESIGNATION: The historic -

Faith on the Avenue
FAITH ON THE AVENUE DDay200613OUS.indday200613OUS.indd i 110/29/20130/29/2013 99:47:25:47:25 PPMM DDay200613OUS.indday200613OUS.indd iiii 110/29/20130/29/2013 99:47:26:47:26 PPMM FAITH ON THE AVENUE Religion on a City Street Katie Day Photographs by Edd Conboy 1 DDay200613OUS.indday200613OUS.indd iiiiii 110/29/20130/29/2013 99:47:26:47:26 PPMM 1 Oxford University Press is a department of the University of Oxford. It furthers the University’s objective of excellence in research, scholarship, and education by publishing worldwide. Oxford New York Auckland Cape Town Dar es Salaam Hong Kong Karachi Kuala Lumpur Madrid Melbourne Mexico City Nairobi New Delhi Shanghai Taipei Toronto With offi ces in Argentina Austria Brazil Chile Czech Republic France Greece Guatemala Hungary Italy Japan Poland Portugal Singapore South Korea Switzerland Th ailand Turkey Ukraine Vietnam Oxford is a registered trademark of Oxford University Press in the UK and certain other countries. Published in the United States of America by Oxford University Press 198 Madison Avenue, New York, NY 10016 © Oxford University Press 2014 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, without the prior permission in writing of Oxford University Press, or as expressly permitted by law, by license, or under terms agreed with the appropriate reproduction rights organization. Inquiries concerning reproduction outside the scope of the above should be sent to the Rights Department, Oxford University Press, at the address above. You must not circulate this work in any other form and you must impose this same condition on any acquirer. -
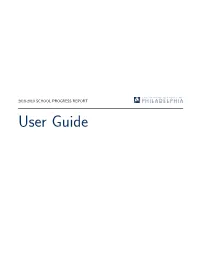
User Guide 2018-2019 School Progress Report User Guide
2018-2019 SCHOOL PROGRESS REPORT User Guide 2018-2019 School Progress Report User Guide Welcome This guide is intended to help you understand the various components that make up the SPR and will cover the following topics: Topic Content Page SPR Components This section provides an overview of the SPR layout and its main 3 & Scoring Overview components. It also provides details on how each metric and domain are scored. Report Types There are four SPR report types. This section explains how a 7 school's report type is determined. Domains The SPR is organized into four domains: Achievement, Progress, 8 Climate, and (for high schools only) College & Career. This section provides a brief overview of each domain. Domain Weights This section explains how each domain is weighted. Because the 9 District is committed to ensuring that all students are learning, the Progress domain is weighted most heavily. Performance Tiers This section explains how a school's progress at the overall, 10 domain, and metric levels is categorized into four performance tiers: Intervene, Watch, Reinforce, and Model. Appendices Additional information on metric definitions; floors, targets, and 11 points possible; peer groups; and schools with consecutive years of overall score improvement. Page 1 2018-2019 School Progress Report User Guide SPR Components & Scoring Overview School Demographics & Performance Tiers Each School Progress Report begins with some basic information about the specific school being evalu- ated. It is formatted as in the sample below. School Name, Address, and The left side of the school demographics section provides all relevant contact Contact Information information for the school being evaluated, including address, phone and fax numbers, and the school's website. -

Fqhcs in Philadelphia Federally Qualified Health Centers
FQHCs in Philadelphia Federally Qualified Health Centers Federally Qualified Health Centers (FQHCs) are “safety net” providers such as community health centers. The main purpose of the FQHC Program is to enhance the provision of primary care services in underserved communities. Any Philadelphia resident is eligible for free or low cost care at the City’s AHS Health Centers. North Philadelphia Facility Address Zip Code Phone AHS Health Center #5 1900 N. 20th St 19121 215-685-2933 AHS Health Center #6 301 W. Girard Ave 19123 215-685-3803 Strawberry Mansion Health Center 2840 Dauphin St 19132 215-685-2401 DVCH Fairmount Primary Care Center 1412 Fairmount Ave 19130 215-235-9600 QCHC Cooke Family Health Center 1300 W. Louden St 19141 215-457-6902 QCHC Family Health Center 2501 W. Lehigh Ave 19132 215-227-0300 QCHC Meade Family Health Center 1600 N. 18th St 19121 215-765-9501 GPHA Hunting Park Health Center 1999 W. Hunting Park Ave 19140 215-228-9300 GPHA Medical Suite At Temple 3223 North Broad St 19140 215-226-3789 DVCH Maria De Los Santos Health Center 401 W. Allegheny Ave 19133 215-291-2500 Esperanza Health Center – Kensington 3156 Kensington Ave 19134 215-831-1100 Esperanza Health Center – N. 5th St. 2940 N. 5th St 19133 215-221-6633 Esperanza Health Center – N. 6th St. 4417 N. 6th St 19134 215-302-3600 PHMC Health Connection 1900 N 9th St 19122 215-765-6690 PHMC Health Center at Temple 3401 North Broad St 19140 215-731-7144 PHMC Congreso 412 W. Lehigh Ave 19133 267-765-2272 Project Home-Stephen Klein Wellness Ctr 2144 Cecil B Moore Ave 19121 215-320-6187 Spectrum Broad St Health Center 1415 N.