Oxygen Therapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oxygen Policy 2018
Oxygen Policy Document Control Title Oxygen Policy (Prescribing & Administration of Oxygen to Adults in Hospital Policy) Author Author’s job title Consultant Physician, Respiratory Medicine Clinical Development Facilitator Directorate Department Division of Medicine, A&E and Comm. Respiratory Hospitals Date Version Status Comment / Changes / Approval Issued June 0.1 Draft Draft presented to Medical Gases Committee. 2010 1.0 Jun Final Approved at Clinical Services Executive Committee 2010 (CSEC) in 14th June 2010. Approved by Drugs and Therapeutics Committee on July 1st 2010. 1.1 Dec Revision Minor amendments by Corporate Affairs to document 2010 control report, filename, header and footer, formatting for document map navigation. Hyperlinks to appendices and Trust procedural documents. Update to document control report. Amendments to section 8 and 24.1. 1.2 Dec Revision Appendix F added 2017 Re wording/re-ordering of most sections Minor alteration to section 5.2 Sepsis 6 added to section 5.2 Addition of endoscopy and ED to 5.8 1.3 June Revision Appendix G added 2018 Minor alteration to section 5.4 2.0 June Final Approved by all members of the Medical Gas Committee 2018 Main Contact Consultant Physician Tel: Direct Dial – 01271 349589 Level 5 Tel: Internal – Ext No. 3375 North Devon District Hospital Raleigh Park Barnstaple, EX31 4JB Lead Director Medical Director Superseded Documents Issue Date Review Date Review Cycle June 2018 June 2021 3 years Respiratory Team Oxygen Policy Page 1 of 39 Oxygen Policy Consulted with the following stakeholders: -
Oxygen Therapy and Oxygen Delivery (Pediatric) - CE
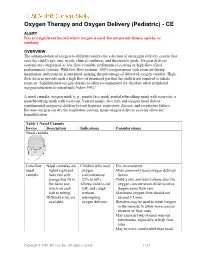
Oxygen Therapy and Oxygen Delivery (Pediatric) - CE ALERT Fire is a significant hazard where oxygen is used. Do not permit flames, sparks, or smoking. OVERVIEW The administration of oxygen to children requires the selection of an oxygen delivery system that suits the child’s age, size, needs, clinical condition, and therapeutic goals. Oxygen delivery systems are categorized as low-flow (variable performance) systems or high-flow (fixed performance) systems. With low-flow systems, 100% oxygen mixes with room air during inspiration, and room air is entrained, making the percentage of delivered oxygen variable. High- flow devices provide such a high flow of premixed gas that the child is not required to inhale room air. Supplemental oxygen therapy is often recommended for children when peripheral oxygen saturation is consistently below 94%.1 A nasal cannula, oxygen mask (e.g., simple face mask, partial rebreathing mask with reservoir, a nonrebreathing mask with reservoir, Venturi mask), face tent, and oxygen hood deliver supplemental oxygen to children to treat hypoxia, respiratory distress, and respiratory failure. Because oxygen can dry the respiratory system, many oxygen delivery systems allow for humidification. Table 1 Nasal Cannula Device Description Indications Considerations Nasal cannula Low-flow Nasal cannulas are Children who need FIO2 inconsistent. nasal lightweight and oxygen Most commonly used oxygen delivery cannula have two soft concentrations device. prongs that fit in 22% to 60%. Child’s size and tidal volume alter the the nares and Allows child to eat, oxygen concentration child receives attach on each talk, and cough despite same flow rate. side to tubing. without Maximum oxygen flow should not Different sizes are interrupting exceed 4 L/min. -

RSP-241 Neonatal and Pediatric Respiratory Care
Bergen Community College Division of Health Professions Department of Respiratory Care RSP-241 NEONATAL/PEDIATRIC RESPIRATORY CARE COURSE SYLLABUS Semester and Year: Course and Section Number: RSP-241 Lab sections 001-004 Meeting Times and Locations: Lecture Tuesday 8:20-10:15AM, Room HP-302. Labs: Monday 08:20-10:15, Monday 10:30-12:30PM, Tuesday 10:30-12:30, Wednesday 12:00-2:00PM. All labs are held in room HP-230. Instructor: Office Location: Phone: Departmental Secretary: Office Hours: Tuesday Email Address: Course Description List lecture hours, laboratory hours, and credits: 2.0 lectures, 2.0 labs, 3.0 credits List prerequisites and co-requisites: Prerequisites: RSP 110,119,121, 210,220, 222,225,226,231,240,250 Co-requisites: RSP 235, 260. Course Description: This course provides a comprehensive overview of pediatric and neonatal respiratory care. Special considerations of respiratory care practice unique to pediatrics and neonatology are discussed. Topics include pediatric anatomy and physiology, fetal development, clinical assessment, oxygen therapy, airway management, mechanical ventilation, resuscitation, cardiopulmonary pathophysiology and disorders specific to this specialty profession within respiratory care. Course Content 1 This course is intended to introduce students to the basic fundamental concepts of neonatal-pediatric respiratory therapy. The course begins with the foundations of respiratory care such as patient assessment skills of the neonate and pediatric patient. The course then covers basic therapeutics including infant and child CPR, airway management, medical gas therapy and delivery, aerosol and humidity therapy, aerosol drug therapy, lung expansion therapy and bronchial hygiene therapy. The course culminates to provide an in depth understanding of all aspects of fetal development, circulation, neonatal and pediatric airway diseases, mechanical ventilation, nasal CPAP management and homecare of the neonatal/pediatric patient. -

Administering Medical Gases
CHAPTER 2 Administering Medical Gases Joseph Lewarski Teresa Volsko © Anna RubaK/ShutterStock, Inc. RubaK/ShutterStock, © Anna OBJECTIVES 13. Describe the operation and uses of nitric oxide. 14. Describe the operation and uses of carbon dioxide/oxygen 1. Describe the basic operation of single-stage and multistage therapy. regulators. 15. Describe the basic function of an oxygen concentrator. 2. Describe the basic operation of a Thorpe tube flowmeter. 3. Compare pressure-compensated devices to non– KEY TERMS pressure-compensated devices. 4. Describe the basic operation of a Bourdon gauge. air-entrainment mask nitric oxide 5. Discuss the operation and uses of oxygen blenders. air/oxygen blender nonrebreathing mask 6. List the indications for and hazards of oxygen therapy. Bourdon gauge oxygen concentrator 7. Define low-flow oxygen therapy, list the devices that provide carbogen oxygen-conserving low-flow therapy, and state the flow and FIO2 specifications flowmeter device (OCD) for these devices. flow restrictor oxygen tent 8. Discuss how the FIO2 from a low-flow device is determined. heliox reducing valve 9. Describe the basic operation of oxygen-conserving devices. high flow reservoir cannula 10. Define high-flow oxygen therapy and list the specifications for high-flow nasal simple mask each device. cannula (HFNC) Thorpe tube 11. Explain the operation and uses of reservoir delivery devices. low flow transtracheal oxygen 12. Describe the operation and uses of helium/oxygen therapy. nasal cannula catheter 33 © Jones & Bartlett Learning LLC, an Ascend Learning Company. NOT FOR SALE OR DISTRIBUTION. 9781284196290_CH02.indd 33 16/07/20 7:09 PM 34 CHAPTER 2 Administering Medical Gases Introduction level. -

Respiratory Care Student Handbook
Respiratory Care Program 2020 – 2021 PROGRAM FACULTY Dr. Christine Blaski, MD - Medical Director Jane Schweizer, MSEd, RRT – Program Director Christopher Mayo, MSc, RRT - Clinical Coordinator Patricia N. Adam, RRT - Instructor Albert Alpuerto, RRT - Clinical Instructor Shaun O’Donnell, RRT - Clinical Instructor Scott Stache, RRT - Clinical Instructor Christine Whitman, RRT - Clinical Instructor Table of Contents Welcome …………………...………………………………………..... 5 Organizational chart…...…………………………………………….. 6 Faculty Information …………………………………………………. 7 Academic Calendar ………………………………………………….. 8 Course Sequence/Graduation Requirements ………………….…... 9 Tuition/Fees/Costs of Program ………………………………………. 10 Definition of Respiratory Care ……………………………………… 11 NSCC Mission Statement ……………………………………………. 12 NSCC Vision Statement ……………………………………………... 12 Strategic Plan Core Values ………………………………………….. 12 Division Mission Statement …………………………………...…….. 13 Program Information Respiratory Care Program Mission Statement………………........... 13 Program Goal ………………………………………………………... 13 Program Outcomes …...……………………………………………… 13 Clinical Affiliates …...…………………………………………………. 14 AARC Statement of Ethics and Professional Conduct ……………... 15 AARC Cultural Diversity Statement ……………………………..….. 16 AARC Scope of Practice for Respiratory Care ….………………….. 17 AARC Tobacco Use Controlled ……………………………… 18 Institutional and Programmatic Accreditation…...…………………. 19 Location of Instruction of RC Students ……………………………... 20 Academic Policies Attendance..……………………………………………………... 21 Professional conduct…………………………………………….. -
A Jurisdictional Review of the Profession of Respiratory Therapy
55 St. Clair Avenue West Suite 806 Box 18 Toronto, Ontario, Canada M4V 2Y7 Toll-Free: 1-888-377-7746 Telephone: 416-326-1550 Fax: 416-326-1549 Web: www.hprac.org Prescribing and Use of Drugs by Non-Physician Health Professionals: A Jurisdictional Review of the Profession of Respiratory Therapy November 2008 Non-Physician Prescribing and Use of Drugs Jurisdictional Review for Profession of Respiratory Therapy November, 2008 Ontario Regulatory Body College of Respiratory Therapy of Ontario Governing Legislation Regulated Health Professions Act Respiratory Therapy Act, 1991 and regulations under the Act Authority to Prescribe/Administer Drugs: Administer only Scope of Practice Respiratory Therapy Act, 1991 3. The practice of respiratory therapy is the providing of oxygen therapy, cardio- respiratory equipment monitoring and the assessment and treatment of cardio-respiratory and associated disorders to maintain or restore ventilation. 1991, c. 39, s. 3; 1998, c. 18, Sched. G, s. 44 (2). Authorized Acts under the Respiratory Therapy Act, 1991 4. In the course of engaging in the practice of respiratory therapy, a member is authorized, subject to the terms, conditions and limitations imposed on his or her certificate of registration, to perform the following: 1. Performing a prescribed procedure below the dermis. 2. Intubation beyond the point in the nasal passages where they normally narrow or beyond the larynx. 3. Suctioning beyond the point in the nasal passages where they normally narrow or beyond the larynx. 4. Administering a substance by injection or inhalation. 1991, c. 39, s. 4; 1998, c. 18, Sched. G, s. 44 (2). Additional requirements for authorized acts 5. -

Respiratory Care (RESC) 1
Respiratory Care (RESC) 1 RESC 3011. Introduction to Patient Assessment. 5 Credit Hours. RESPIRATORY CARE (RESC) This course will introduce the student to the fundamentals of respiratory assessment to include review of existing data in the patient record, Courses patient history, physical examination, oximetry, blood gases, respiratory RESC 3002. Fundamentals of Respiratory Care. 5 Credit Hours. monitoring, pulmonary function assessment, laboratory studies, chest The course will present the principles of chemistry and physics as they and upper airway radiographs, ventilation/perfusion scans, bedside EKG apply to respiratory care. Students will have the opportunity to gain interpretation, cardiovascular monitoring, and nutritional assessment. hands-on experience with basic respiratory care equipment. Specific The student will be introduced to the concepts associated with chronic types of therapy are examined to understand the principles of application care and disease management. to patients, indications, hazards, contraindications, select, assemble, and RESC 3018. Diseases Affecting the Respiratory System. 4 Credit Hours. troubleshoot equipment. Equipment will include oxygen delivery services, The course provides a comprehensive approach to etiology, aerosol generators, medication delivery devices, pressure ventilators, gas pathophysiology, clinical manifestations, diagnosis, treatment, and delivery, metering and analyzing devices, percussor, positive pressure prognosis of common pulmonary diseases and syndromes. Main devices, environmental devices, manometers, gauges, and vacuum topics include obstructive and restrictive pulmonary and cardiovascular systems. disorders. Non-respiratory disorders impacting cardiopulmonary function RESC 3005. Respiratory Care Pharmacology. 3 Credit Hours. commonly encountered in the critical care unit will be discussed. This course introduces the physiologic and pharmacologic basis of RESC 3019. Clinical Practice 1. 3 Credit Hours. pulmonary and cardiac medications. -

Respiratory Care Technology Mississippi Curriculum Framework
Respiratory Care Technology Mississippi Curriculum Framework Program CIP: 51.0908– Respiratory Care Therapist/Therapy November 2014 Published by: Mississippi Community College Board Division of Workforce, Career, and Technical Education 3825 Ridgewood Road Jackson, MS 39211 Phone: 601-432-6155 Email: [email protected] 1 FACULTY WRITING TEAM MEMBERS Willie Lockett, Coahoma Community College Doug Treanor, Coahoma Community College Walton Wilson, Copiah-Lincoln Community College Shirley Jenkins, Hinds Community College Therese Winschel, Hinds Community College Adam Denton, Itawamba Community College Steve Arinder, Meridian Community College Beverly Prince, Northeast Mississippi Community College John Shelburne, Northeast Mississippi Community College Regina Clark, Northwest Mississippi Community College Lori Anderson, Pearl River Community College ADMINISTRATOR WRITING TEAM MEMBERS Christy Bokros, Assistant Dean for Allied Health Dean of Jackson Campus, Hinds Community College Sherry Franklin, Dean of Career/Technical Education of Rankin Campus, Hinds Community College BUSINESS AND INDUSTRY WRITING TEAM MEMBERS Stan Grantham, Director of Respiratory Care, Wesley Medical Center Linda Croff-Poole, Director and Assistant Professor, Department of Health Sciences, University of Mississippi Medical Center OFFICE OF CURRICULUM AND INSTRUCTION TEAM MEMBERS Elmira Ratliff, Curriculum Specialist, Office of Curriculum and Instruction, Mississippi Community College Board Robin Parker, Director of Curriculum and Instruction, Office of Curriculum and Instruction, Mississippi Community College Board 2 The Office of Curriculum and Instruction (OCI) was founded in 2013 under the Division of Workforce, Career, and Technical Education at the Mississippi Community College Board (MCCB). The office is funded through a partnership with The Mississippi Department of Education (MDE), who serves as Mississippi’s fiscal agent for state and federal Career and Technical Education (CTE) Funds. -

Departmental Syllabus Form
Bergen Community College Division of Health Professions Department of Respiratory Care RSP-119 INTRODUCTION TO RESPIRATORY CARE Semester and Year: Course and Section Number: RSP-119 Lab sections 001-004 Meeting Times and Locations: Lecture Thursday, Friday 0800-0915 room HP-126 All labs in room HP-230 Instructor: Office Location: Phone: Departmental Secretary: Office Hours: Email Address: Course Description List lecture hours, laboratory hours, and credits: 3.0 lectures, 3.0 labs, 4.0 credits List co-requisites: RSP-110, RSP-121. Course Description: Introduction to Respiratory Therapy is a study of the respiratory therapist's role as a member of the medical team. Gas laws, physics, physiology, medical equipment terminology are taught. In addition, it provides the student with an in depth understanding of medical gas administration, humidity and aerosol therapy, safety systems, airway management and infection control. Students will also learn the mechanical devices utilized to maintain patent airways and the various utilities in the treatment of respiratory and cardiac arrest. Laboratory exercises provide students with an opportunity to develop skills in the application of all equipment modalities, and to demonstrate their skills in resuscitation and airway management. Course Content This course is intended to introduce students to the fundamental concepts of respiratory therapy. The course begins with the foundations of respiratory care such as history, patient safety, communication, record keeping, and principles of infection control, ethics, gas laws and physics. Gas exchange, 02 transport, and regulation of breathing, patient assessment skills are covered. The course then covers basic therapeutics including CPR, medical gas therapy and delivery, aerosol and humidity therapy, aerosol drug therapy, lung expansion therapy and bronchial hygiene therapy. -
Introduction to Medical Gases
CHAPTER 1 Introduction to Medical Gases Teresa Volsko Keith Hirst © Anna RubaK/ShutterStock, Inc. RubaK/ShutterStock, © Anna OBJECTIVES KEY TERMS 1. Define a medical gas. American National Pin Index Safety 2. Describe the types of gases used in respiratory care. Standards Institute System (PISS) 3. Explain how medical gases are delivered to the patient. (ANSI) piston compressor 4. Describe how liquid oxygen is formed. American Standard Safety pressure-relief valve 5. Describe how liquid oxygen is delivered to the patient. System (ASSS) quick-connect adapter 6. Differentiate between liquid and compressed gas. Diameter Index Safety rotary compressor 7. Describe the piping system used in acute care facilities. System (DISS) rupture disk 8. Discuss the use of station outlets and the types of diaphragm compressor spring-loaded device connectors used. direct-acting valve terminal unit 9. Explain the various methods of testing the hospital gas fractional distillation Wood’s metal distribution system. fusible plug zone valve 10. Identify problems with a hospital piping system. indirect-acting valve 11. Discuss how medical gases are stored and transported. 12. Identify the various cylinder sizes and colors and how they relate to the particular medical gas contents. 13. Discuss how oxygen concentrators work. 1 © Jones & Bartlett Learning LLC, an Ascend Learning Company. NOT FOR SALE OR DISTRIBUTION. 9781284196290_CH01.indd 1 20/06/20 10:28 AM 2 CHAPTER 1 Introduction to Medical Gases Introduction calibration; for example, oxygen mixtures are used in the calibration of gas cylinders for transcutaneous oxy- Respiratory therapists have a wide range of medical gen monitors. gases at their disposal. -

Bsc Respiratory Therapy Curriculum
A Multi Campus University with ‘A’ Grade Accreditation by NAAC AMRITA SCHOOL OF MEDICINE Amrita Centre for Allied Health Sciences AIMS Ponekk ara PO, Kochi – 682 041 Tel: 0484 – 2858131, 2858375, 2858845 Fax: 0484-2858382 Email: [email protected] Web: www.amrita.edu CURRICULUM BSc Respiratory Therapy (Revised with effect from 2014-2015 onwards) Our A Super Speciality Tertiary Care Hospital Accredited by ISO 9001-2008, NABL & NABH B.Sc Respiratory Therapy Page 1 of 56 Our Chancellor SPIRITUAL PRINCIPLES IN EDUCATION “In the gurukulas of ancient rishis, when the master spoke it was love that spoke; and at the receiving end disciple absorbed of nothing but love. Because of their love for their Master, the disciples’ hearts were like a fer- tile field, ready to receive the knowledge imparted by the Master. Love given and love received. Love made them open to each other. True giving and receiving take place where love is present. Real listening and ‘sradd- ha’ is possible only where there is love, otherwise the listener will be closed. If you are closed you will be easily dominated by anger and re- sentment, and nothing can enter into you”. “Satguru Mata Amritanandamayi Devi” B.Sc Respiratory Therapy Page 2 of 56 Introducing AIMS India is the second most populous nation on earth. This means that India’s health prob- lems are the world’s health problems. And by the numbers, these problems are stagger- ing 41 million cases of diabetes, nearly half the world’s blind population, and 60% of the world’s incidences of heart disease. -
Development and Implementation of Respiratory Care Plans
CHAPTER © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION 2NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC DevelopmentNOT FOR SALE OR DISTRIBUTIONand ImplementationNOT FOR SALE OR DISTRIBUTION of Respiratory Care Plans © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DavidDISTRIBUTION C. Shelledy, Jay I.NOT Peters FOR SALE OR DISTRIBUTION © Toria/Shutterstock © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION CHAPTER OUTLINE 11. Design a respiratory care plan to mobilize secretions. 12. Propose a respiratory care plan for the treatment and/or Overview © Jones & Bartlett Learning, LLC prevention of atelectasis and© pneumonia. Jones & Bartlett Learning, LLC Introduction to RespiratoryNOT Care Plans FOR SALE OR DISTRIBUTION13. Give examples of types of respiratoryNOT FOR care plans SALE used inOR the DISTRIBUTION Common Conditions Requiring Care Plan Development intensive care unit. Respiratory Care Plan Development 14. Explain the role of diagnostic testing in the development of a Maintain Adequate Tissue Oxygenation respiratory care plan. Treat and/or Prevent Bronchospasm and Mucosal Edema Assessment and Treatment of COPD KEY TERMS Mobilize© Jones and Remove & SecretionsBartlett Learning, LLC © Jones & Bartlett Learning, LLC ProvideNOT Lung FOR Expansion SALE Therapy OR DISTRIBUTION acute respiratoryNOT distress FOR SALEhistory OR DISTRIBUTION Critical Care and Mechanical Ventilation syndrome (ARDS) hypoxemia Diagnostic Testing acute respiratory incentive spirometry (IS) Respiratory Care Plan Format failure (ARF) inhaled corticosteroid acute ventilatory (ICS) CHAPTER OBJECTIVES failure (AVF) intermittent positive © Jones & Bartlett Learning, LLC © Jonesairway &clearance Bartlett Learning,pressure LLC breathing 1.