Administering Medical Gases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Use of Heliox in Treating Decompression Illness
The Diving Medical Advisory Committee DMAC, Eighth Floor, 52 Grosvenor Gardens, London SW1W 0AU, UK www.dmac-diving.org Tel: +44 (0) 20 7824 5520 [email protected] The Use of Heliox in Treating Decompression Illness DMAC 23 Rev. 1 – June 2014 Supersedes DMAC 23, which is now withdrawn There are many ways of treating decompression illness (DCI) at increased pressure. In the past 20 years, much has been published on the use of oxygen and helium/oxygen mixtures at different depths. There is, however, a paucity of carefully designed scientific studies. Most information is available from mathematical models, animal experiments and case reports. During a therapeutic compression, the use of a different inert gas from that breathed during the dive may facilitate bubble resolution. Gas diffusivity and solubility in blood and tissue is expected to play a complex role in bubble growth and shrinkage. Mathematical models, supported by some animal studies, suggest that breathing a heliox gas mixture during recompression could be beneficial for nitrogen elimination after air dives. In humans, diving to 50 msw, with air or nitrox, almost all cases of DCI can be adequately treated at 2.8 bar (18 msw), where 100% oxygen is both safe and effective. Serious neurological and vestibular DCI with only partial improvements during initial compression at 18 msw on oxygen may benefit from further recompression to 30 msw with heliox 50:50 (Comex therapeutic table 30 – CX30). There have been cases successfully treated on 50:50 heliox (CX30), on the US Navy recompression tables with 80:20 and 60:40 heliox (USN treatment table 6A) instead of air and in heliox saturation. -

Optimal Breathing Gas Mixture in Professional Diving with Multiple Supply
Proceedings of the World Congress on Engineering 2021 WCE 2021, July 7-9, 2021, London, U.K. Optimal Breathing Gas Mixture in Professional Diving with Multiple Supply Orhan I. Basaran, Mert Unal compressors and cylinders, it was limited to surface air Abstract— Professional diving existed since antiquities when supply lines. In 1978, Fleuss introduced the first closed divers collected resources from the bottom of the seas and circuit oxygen breathing apparatus which removed carbon lakes. With technological advancements in the recent century, dioxide from the exhaled gas and did not form bubbles professional diving activities also increased significantly. underwater. In 1943, Cousteau and Gangan designed the Diving has many adverse effects on human physiology which first proper demand-regulated air supply from compressed are widely investigated in order to make dives safer. In this air cylinders worn on the back. The scuba equipment with study, we focus on optimizing the breathing gas mixture minimizing the dive costs while ensuring the safety of the the high-pressure regulator on the cylinder and a single hose divers. The methods proposed in this paper are purely to a demand valve was invented in Australia and marketed theoretical and divers should always have appropriate training by Ted Eldred in the early 1950s [1]. and certificates. Also, divers should never perform dives With the use of Siebe dress, the first cases of decompression without consulting professionals and medical doctors with expertise in related fields. sickness began to be documented. Haldane conducted several experiments on animal and human subjects in Index Terms—-professional diving; breathing gas compression chambers to investigate the causes of this optimization; dive profile optimization sickness and how it can be prevented. -

Preventing Breathing- Gas Contamination
RESEARCH, EDUCATION & MEDICINE // SAFETY 101 Preventing Breathing- STEPHEN FRINK Gas Contamination BY BRITTANY TROUT ncidents involving bad breathing gas — be it Recommendations for Compressor Operators air, nitrox, trimix or another mixture — are Compressor operators can help prevent gas rare, yet they do occur. Health effects on divers contamination and mitigate the risk of dive accidents vary depending on the contaminant breathed. in several ways. Among the most severe symptoms of breathing Attentive compressor maintenance. Proper contaminated gas are impaired judgment and loss of compressor maintenance helps ensure breathing-gas consciousness, both of which may be deadly underwater. quality as well as extends the life of the compressor. ISources of contamination include hydrocarbons Breathing-gas contamination is less likely in well- from compressor lubricants, carbon monoxide (CO) maintained and properly functioning compressors. from engine exhaust (or overheated compressor oil) If maintenance is neglected and the compressor and impurities from the surrounding environment such overheats, the lubricating oil may break down and as methane and carbon dioxide (CO2). Dust particles produce CO and other noxious byproducts. in breathing gas can also be hazardous, potentially Effective procedures. A fill checklist can help ensure impairing respiratory function or damaging diving safety procedures are remembered when cylinders equipment. Excessive moisture can cause corrosion are filled. Before starting to fill tanks, the operator in scuba cylinders and other dive gear and may cause should inspect the compressor’s filters for damage regulators to freeze due to adiabatic cooling (heat loss and note the presence of contaminants such as subsequent to increased gas volume). cigarette smoke, paint fumes or engine exhaust near the intake. -

Oxygen Policy 2018
Oxygen Policy Document Control Title Oxygen Policy (Prescribing & Administration of Oxygen to Adults in Hospital Policy) Author Author’s job title Consultant Physician, Respiratory Medicine Clinical Development Facilitator Directorate Department Division of Medicine, A&E and Comm. Respiratory Hospitals Date Version Status Comment / Changes / Approval Issued June 0.1 Draft Draft presented to Medical Gases Committee. 2010 1.0 Jun Final Approved at Clinical Services Executive Committee 2010 (CSEC) in 14th June 2010. Approved by Drugs and Therapeutics Committee on July 1st 2010. 1.1 Dec Revision Minor amendments by Corporate Affairs to document 2010 control report, filename, header and footer, formatting for document map navigation. Hyperlinks to appendices and Trust procedural documents. Update to document control report. Amendments to section 8 and 24.1. 1.2 Dec Revision Appendix F added 2017 Re wording/re-ordering of most sections Minor alteration to section 5.2 Sepsis 6 added to section 5.2 Addition of endoscopy and ED to 5.8 1.3 June Revision Appendix G added 2018 Minor alteration to section 5.4 2.0 June Final Approved by all members of the Medical Gas Committee 2018 Main Contact Consultant Physician Tel: Direct Dial – 01271 349589 Level 5 Tel: Internal – Ext No. 3375 North Devon District Hospital Raleigh Park Barnstaple, EX31 4JB Lead Director Medical Director Superseded Documents Issue Date Review Date Review Cycle June 2018 June 2021 3 years Respiratory Team Oxygen Policy Page 1 of 39 Oxygen Policy Consulted with the following stakeholders: -
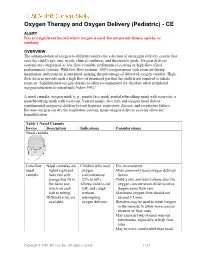
Oxygen Therapy and Oxygen Delivery (Pediatric) - CE
Oxygen Therapy and Oxygen Delivery (Pediatric) - CE ALERT Fire is a significant hazard where oxygen is used. Do not permit flames, sparks, or smoking. OVERVIEW The administration of oxygen to children requires the selection of an oxygen delivery system that suits the child’s age, size, needs, clinical condition, and therapeutic goals. Oxygen delivery systems are categorized as low-flow (variable performance) systems or high-flow (fixed performance) systems. With low-flow systems, 100% oxygen mixes with room air during inspiration, and room air is entrained, making the percentage of delivered oxygen variable. High- flow devices provide such a high flow of premixed gas that the child is not required to inhale room air. Supplemental oxygen therapy is often recommended for children when peripheral oxygen saturation is consistently below 94%.1 A nasal cannula, oxygen mask (e.g., simple face mask, partial rebreathing mask with reservoir, a nonrebreathing mask with reservoir, Venturi mask), face tent, and oxygen hood deliver supplemental oxygen to children to treat hypoxia, respiratory distress, and respiratory failure. Because oxygen can dry the respiratory system, many oxygen delivery systems allow for humidification. Table 1 Nasal Cannula Device Description Indications Considerations Nasal cannula Low-flow Nasal cannulas are Children who need FIO2 inconsistent. nasal lightweight and oxygen Most commonly used oxygen delivery cannula have two soft concentrations device. prongs that fit in 22% to 60%. Child’s size and tidal volume alter the the nares and Allows child to eat, oxygen concentration child receives attach on each talk, and cough despite same flow rate. side to tubing. without Maximum oxygen flow should not Different sizes are interrupting exceed 4 L/min. -

Respiration (Physiology) 1 Respiration (Physiology)
Respiration (physiology) 1 Respiration (physiology) In physiology, respiration (often mistaken with breathing) is defined as the transport of oxygen from the outside air to the cells within tissues, and the transport of carbon dioxide in the opposite direction. This is in contrast to the biochemical definition of respiration, which refers to cellular respiration: the metabolic process by which an organism obtains energy by reacting oxygen with glucose to give water, carbon dioxide and ATP (energy). Although physiologic respiration is necessary to sustain cellular respiration and thus life in animals, the processes are distinct: cellular respiration takes place in individual cells of the animal, while physiologic respiration concerns the bulk flow and transport of metabolites between the organism and the external environment. In unicellular organisms, simple diffusion is sufficient for gas exchange: every cell is constantly bathed in the external environment, with only a short distance for gases to flow across. In contrast, complex multicellular animals such as humans have a much greater distance between the environment and their innermost cells, thus, a respiratory system is needed for effective gas exchange. The respiratory system works in concert with a circulatory system to carry gases to and from the tissues. In air-breathing vertebrates such as humans, respiration of oxygen includes four stages: • Ventilation, moving of the ambient air into and out of the alveoli of the lungs. • Pulmonary gas exchange, exchange of gases between the alveoli and the pulmonary capillaries. • Gas transport, movement of gases within the pulmonary capillaries through the circulation to the peripheral capillaries in the organs, and then a movement of gases back to the lungs along the same circulatory route. -

Development of Ventilatory Response to Transient Hypercapnia and Hypercapnic Hypoxia in Term Infants
0031-3998/04/5502-0302 PEDIATRIC RESEARCH Vol. 55, No. 2, 2004 Copyright © 2004 International Pediatric Research Foundation, Inc. Printed in U.S.A. Development of Ventilatory Response to Transient Hypercapnia and Hypercapnic Hypoxia in Term Infants SIGNE SØVIK AND KRISTIN LOSSIUS Department of Physiology, Institute of Basic Medical Sciences, University of Oslo, NO-0317 Oslo [S.S.], and Section of Neonatology, Department of Pediatrics, Rikshospitalet, NO–0027 Oslo [K.L.], Norway ABSTRACT Whereas peripheral chemoreceptor oxygen sensitivity in- was unchanged for hypoxia. Response magnitude was unchanged creases markedly after birth, previous studies of ventilatory for hypercapnia, but increased for the two hypoxic stimuli. In responses to CO2 in term infants have shown no postnatal conclusion, an interaction between the effects of hypercapnia and development. However, the hypercapnic challenges applied have hypoxia on ventilatory response rate emerged between postnatal usually been long-term, which meant that the effect of central d 2 and wk 8 in term infants. Concomitantly, stimulus-response chemoreceptors dominated. Oscillatory breathing, apneas, and time to hypercapnic stimuli declined markedly. The development sighs cause transient PCO2 changes, probably primarily stimulat- of a prompt response to transient hypercapnia may be important ing peripheral chemoreceptors. We wanted to assess whether the for infant respiratory stability. (Pediatr Res 55: 302–309, 2004) immediate ventilatory responses to step changes in inspired CO2 and O2 in term infants undergo postnatal developmental changes. Twenty-six healthy term infants were studied during natural Abbreviations sleep 2 d and 8 wk postnatally. Ventilatory responses to a FiCO2, fraction of inspired carbon dioxide randomized sequence of 15 s hypercapnia (3% CO2), hypoxia fR, respiratory rate ϩ (15% O2), and hypercapnic hypoxia (3% CO2 15% O2) were PaCO2, partial pressure of arterial carbon dioxide recorded breath-by-breath using a pneumotachometer. -

Carbon Monoxide Poisoning Claims Impact Upon a Number of Parties Including Owner Occupiers, Gas Engineers, House Builders and Housing Authorities
CARBON MONOXIDE POISONING OCCUPATIONAL DISEASE GUIDE 8 OCCUPATIONAL DISEASE OCCUPATIONAL Carbon Monoxide Poisoning Occupational disease series – Guide 8 Contents Introduction 1. Insurance 2. Damages and the Reserve 3. The Landlord’s Duty 4. Investigations 5. Medical Causation 6. Expert evidence 7. CRU 8. Making a decision 1 Introduction Carbon monoxide (“CO”) is a colourless, tasteless, odourless non-irritant gas which, if inhaled, is acutely toxic. It can be formed when any type of fuel, such as gas, wood or coal, is burned. As a result, any fuel-burning appliance, such as a fireplace, woodstove and gas appliance, has the potential to produce dangerous levels of CO. Whilst only very small amounts of CO are produced by gas appliances which have been installed and maintained correctly, dangerous levels of CO can be emitted if gas burns incompletely – this is known as incomplete combustion. This can occur, for example, if the appliance has inadequate ventilation. There are a number of potential sources for the production of CO within the home (see figure 1), and given the difficulty in detecting the fumes, CO poisoning is a major domestic health hazard and a leading cause of death by poisoning throughout the world. The NHS estimates that CO poisoning causes approximately 50 deaths in the home per year in the UK. There are over 200 cases of non-fatal injuries per year including temporary or permanent brain damage. Incidents increase during the winter when the use of gas boilers and fires escalates. This guide is drafted from the perspective of a landlord/tenant claim. However, carbon monoxide poisoning claims impact upon a number of parties including owner occupiers, gas engineers, house builders and housing authorities. -

RSP-241 Neonatal and Pediatric Respiratory Care
Bergen Community College Division of Health Professions Department of Respiratory Care RSP-241 NEONATAL/PEDIATRIC RESPIRATORY CARE COURSE SYLLABUS Semester and Year: Course and Section Number: RSP-241 Lab sections 001-004 Meeting Times and Locations: Lecture Tuesday 8:20-10:15AM, Room HP-302. Labs: Monday 08:20-10:15, Monday 10:30-12:30PM, Tuesday 10:30-12:30, Wednesday 12:00-2:00PM. All labs are held in room HP-230. Instructor: Office Location: Phone: Departmental Secretary: Office Hours: Tuesday Email Address: Course Description List lecture hours, laboratory hours, and credits: 2.0 lectures, 2.0 labs, 3.0 credits List prerequisites and co-requisites: Prerequisites: RSP 110,119,121, 210,220, 222,225,226,231,240,250 Co-requisites: RSP 235, 260. Course Description: This course provides a comprehensive overview of pediatric and neonatal respiratory care. Special considerations of respiratory care practice unique to pediatrics and neonatology are discussed. Topics include pediatric anatomy and physiology, fetal development, clinical assessment, oxygen therapy, airway management, mechanical ventilation, resuscitation, cardiopulmonary pathophysiology and disorders specific to this specialty profession within respiratory care. Course Content 1 This course is intended to introduce students to the basic fundamental concepts of neonatal-pediatric respiratory therapy. The course begins with the foundations of respiratory care such as patient assessment skills of the neonate and pediatric patient. The course then covers basic therapeutics including infant and child CPR, airway management, medical gas therapy and delivery, aerosol and humidity therapy, aerosol drug therapy, lung expansion therapy and bronchial hygiene therapy. The course culminates to provide an in depth understanding of all aspects of fetal development, circulation, neonatal and pediatric airway diseases, mechanical ventilation, nasal CPAP management and homecare of the neonatal/pediatric patient. -

(CH 13) Part 2 – Control of Breathing / Gas Exchange and Transport *Normal Breathing Is Rhythmic and Involuntary
NOTES: Respiratory System (CH 13) Part 2 – Control of Breathing / Gas Exchange and Transport *Normal breathing is rhythmic and involuntary. Respiratory Center: ● the respiratory center is in the brain stem and includes portions of the PONS and MEDULLA OBLONGATA FACTORS AFFECTING BREATHING: 1) respiratory center in the brain 2) chemical concentrations (gases, ions, pH, etc.) 3) stretching of lung tissue 4) emotional state EXAMPLES: *when chemoreceptors in the walls of certain large arteries detect low O2 levels (or high CO2 levels), breathing rate increases *fear and pain typically increase the normal breathing pattern ALVEOLAR GAS EXCHANGES *Gas exchange between air and blood occurs in the alveoli. ● ALVEOLI: tiny air sacs in the lungs clustered at the ends of alveolar ducts ALVEOLAR GAS EXCHANGES ● Gases (O2 and CO2) diffuse from regions of HIGH concentration (and partial pressure) to regions of LOW concentration (partial pressure) ● OXYGEN diffuses from alveolar air into blood ● CARBON DIOXIDE diffuses from blood into alveolar air Partial Pressure in Partial Pressure in Gas Action Blood Alveolar Space Carbon Dioxide 45 mm Hg exit 40 mm Hg enter Oxygen 40 mm Hg 104 mm Hg blood GAS TRANSPORT IN THE BLOOD / BODY *Blood transports gases between the lungs and body cells. OXYGEN TRANSPORT: ● oxygen binds to the protein hemoglobin in the blood - heme = group that surrounds an atom of iron - globin = protein made up 574 amino acids in 4 polypeptide chains ● the resulting molecule, oxyhemoglobin, is unstable and readily releases oxygen in regions -

6. TOXICOKINETICS and METABOLISM 6.1 Introduction
6. TOXICOKINETICS AND METABOLISM 6.1 Introduction The binding of carbon monoxide to haemoglobin, producing car- boxyhaemoglobin, decreases the oxygen carrying capacity of blood and interferes with oxygen release at the tissue level; these two main mechanisms of action underlie the potentially toxic effects of low- level carbon monoxide exposure. Impaired delivery of oxygen can interfere with cellular respiration and result in tissue hypoxia. Hypoxia of sensitive tissues, in turn, can affect the function of many organs, including the lungs. The effects would be expected to be more pronounced under conditions of stress, as with exercise, for example. Although the principal cause of carbon monoxide-induced toxicity at low exposure levels is thought to be increased carboxyhaemoglobin formation, the physiological response to carbon monoxide at the cellu- lar level and its related biochemical effects are still not fully under- stood. Other mechanisms of carbon monoxide-induced toxicity have been hypothesized and assessed, such as hydroxyl radical production (Piantadosi et al., 1997) and lipid peroxidation (Thom, 1990, 1992, 1993) in the brain of carbon monoxide-poisoned rats, but none has been demonstrated to operate at relatively low (near-ambient) carbon monoxide exposure levels. 6.2 Endogenous carbon monoxide production In addition to exogenous sources, humans are also exposed to small amounts of carbon monoxide produced endogenously. In the process of natural degradation of haemoglobin to bile pigments, in concert with the microsomal reduced nicotinamide adenine dinucleo- tide phosphate (NADPH) cytochrome P-450 reductase, two haem oxygenase isoenzymes, HO-1 and HO-2, catalyse the oxidative break- down of the "-methene bridge of the tetrapyrrol ring of haem, leading to the formation of biliverdin and carbon monoxide. -

COVID-19 Technical Specifications for Procurement of Oxygen Therapy and Monitoring Devices
WHO/2020-nCoV/MedDev/TS/O2T.V1 17 June 2020 Final draft 10-07-2020 pending integration to a single publication with all other technical specifications COVID-19 Technical specifications for procurement of oxygen therapy and monitoring devices Contents Abbreviations 1. Context and considerations 2. Definitions and intended use 2.1 Oxygen sources devices Oxygen concentrator Oxygen cylinder 2.2 Oxygen delivery devices Nasal oxygen cannula with prongs Mask with reservoir bag Venturi mask 2.3 Devices for oxygen regulation and conditioning Flowmeter, Thorpe tube Flow splitter Non-heated bubble humidifier Tubing (for medical gases) 2.4 Manual ventilation devices Self-inflating resuscitation bag with mask Heat and moisture exchanger filter (HMEF) Colourimetric end-tidal CO2 (EtCO2) detector 2.5 Patient monitoring devices Pulse oximeter: handheld; tabletop; fingertip Patient monitor multiparametric: basic; intermediate; advanced 3. Technical specifications for procurement 3.1 Oxygen sources devices Oxygen concentrator Oxygen cylinder 3.2 Oxygen delivery devices Nasal oxygen cannula with prongs Mask with reservoir bag Venturi mask 3.3 Devices for oxygen regulation and conditioning Flowmeter, Thorpe tube Flow splitter 1 WHO/2020-nCoV/MedDev/TS/O2T.V1 17 June 2020 Final draft 10-07-2020 pending integration to a single publication with all other technical specifications COVID-19 Technical specifications for procurement of oxygen therapy and monitoring devices Non-heated bubble humidifier Tubing (for medical gases) 3.4 Manual ventilation devices Self-inflating resuscitation bag with mask Heat and moisture exchanger filter (HMEF) Colourimetric end-tidal CO2 (EtCO2) detector 3.5 Patient monitoring devices Pulse oximeter: handheld; tabletop; fingertip Patient monitor multiparametric: basic; intermediate; advanced 4.