Graduate Neuroanatomy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Impact of Precisely-Timed Inhibition of Gustatory Cortex On
1 Impact of precisely-timed inhibition of gustatory cortex 2 on taste behavior depends on single-trial ensemble 3 dynamics ∗1 2 y3 4 Narendra Mukherjee , Joseph Wachukta , and Donald B Katz 1,2,3 5 Program in Neuroscience, Brandeis University 1,2,3 6 Volen National Center for Complex Systems, Brandeis University 3 7 Department Of Psychology, Brandeis University 8 Abstract 9 Sensation and action are necessarily coupled during stimulus perception – while tasting, 10 for instance, perception happens while an animal decides to expel or swallow the substance 11 in the mouth (the former via a behavior known as “gaping”). Taste responses in the ro- 12 dent gustatory cortex (GC) span this sensorimotor divide, progressing through firing-rate 13 epochs that culminate in the emergence of action-related firing. Population analyses re- 14 veal this emergence to be a sudden, coherent and variably-timed ensemble transition that 15 reliably precedes gaping onset by 0.2-0.3s. Here, we tested whether this transition drives 16 gaping, by delivering 0.5s GC perturbations in tasting trials. Perturbations significantly 17 delayed gaping, but only when they preceded the action-related transition - thus, the same 18 perturbation impacted behavior or not, depending on the transition latency in that partic- 19 ular trial. Our results suggest a distributed attractor network model of taste processing, 20 and a dynamical role for cortex in driving motor behavior. ∗[email protected] [email protected] 1 21 1 Introduction 22 One of the primary purposes of sensory processing is to drive action, such that the source 23 of sensory information is either acquired or avoided (in the process generating new sensory 24 input, Prinz(1997), Wolpert and Kawato(1998), Wolpert and Ghahramani(2000)). -

Food, Food Chemistry and Gustatory Sense
Food, Food Chemistry and Gustatory Sense COOH N H María González Esguevillas MacMillan Group Meeting May 12th, 2020 Food and Food Chemistry Introduction Concepts Food any nourishing substance eaten or drunk to sustain life, provide energy and promote growth any substance containing nutrients that can be ingested by a living organism and metabolized into energy and body tissue country social act culture age pleasure election It is fundamental for our life Food and Food Chemistry Introduction Concepts Food any nourishing substance eaten or drunk to sustain life, provide energy and promote growth any substance containing nutrients that can be ingested by a living organism and metabolized into energy and body tissue OH O HO O O HO OH O O O limonin OH O O orange taste HO O O O 5-caffeoylquinic acid Coffee taste OH H iPr N O Me O O 2-decanal Capsaicinoids Coriander taste Chilli burning sensation Astray, G. EJEAFChe. 2007, 6, 1742-1763 Food and Food Chemistry Introduction Concepts Food Chemistry the study of chemical processes and interactions of all biological and non-biological components of foods biological substances areas food processing techniques de Man, J. M. Principles of Food Chemistry 1999, Springer Science Fennema, O. R. Food Chemistry. 1985, 2nd edition New York: Marcel Dekker, Inc Food and Food Chemistry Introduction Concepts Food Chemistry the study of chemical processes and interactions of all biological and non-biological components of foods biological substances areas food processing techniques carbo- hydrates water minerals lipids flavors vitamins protein food enzymes colors additive Fennema, O. R. Food Chemistry. -

Brain Sulci and Gyri: a Practical Anatomical Review
Journal of Clinical Neuroscience 21 (2014) 2219–2225 Contents lists available at ScienceDirect Journal of Clinical Neuroscience journal homepage: www.elsevier.com/locate/jocn Neuroanatomical study Brain sulci and gyri: A practical anatomical review ⇑ Alvaro Campero a,b, , Pablo Ajler c, Juan Emmerich d, Ezequiel Goldschmidt c, Carolina Martins b, Albert Rhoton b a Department of Neurological Surgery, Hospital Padilla, Tucumán, Argentina b Department of Neurological Surgery, University of Florida, Gainesville, FL, USA c Department of Neurological Surgery, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina d Department of Anatomy, Universidad de la Plata, La Plata, Argentina article info abstract Article history: Despite technological advances, such as intraoperative MRI, intraoperative sensory and motor monitor- Received 26 December 2013 ing, and awake brain surgery, brain anatomy and its relationship with cranial landmarks still remains Accepted 23 February 2014 the basis of neurosurgery. Our objective is to describe the utility of anatomical knowledge of brain sulci and gyri in neurosurgery. This study was performed on 10 human adult cadaveric heads fixed in formalin and injected with colored silicone rubber. Additionally, using procedures done by the authors between Keywords: June 2006 and June 2011, we describe anatomical knowledge of brain sulci and gyri used to manage brain Anatomy lesions. Knowledge of the brain sulci and gyri can be used (a) to localize the craniotomy procedure, (b) to Brain recognize eloquent areas of the brain, and (c) to identify any given sulcus for access to deep areas of the Gyri Sulci brain. Despite technological advances, anatomical knowledge of brain sulci and gyri remains essential to Surgery perform brain surgery safely and effectively. -

Spinal Tracts.Pdf
Spinal Tracts Andreas Talgø Lie Illustrations by: Peder Olai Skjeflo Holman Previous material: Maja Solbakken Definitions to bring home Nerve Ganglion Neuron Nucleus Tract Collection neurons Collection of nerve A single cell Collection of Collection of axons that transmits cell bodies in the transmitting nerve cell bodies in traveling up or sensation or motor PNS, typically linked electrical impluses. the CNS, typically down the spinal impulses depending by synapses. linked by synapses. cord, depending on the function and Location: both on function destination. Location: PNS Location: CNS and destination. Location: PNS Location: CNS - does it matter? Tract - highway to pass anatomy exam? • Highway = Tract • Lane = Neuron • Car = Signal Slow... Fast!! Just to make sure... • Ipsilateral or contralateral • Ventral = anterior • Dorsal = posterior High yield points to understand • What does the tract transmit - Motor or sensory? If sensory: which sensation? • Where does the neurones synapse - 1.st, 2nd and 3rd order neron? Which ganglion/nuclei? • Where there are decussations - If there are any decussations at all? ASCENDING / SENSORY TRACTS Sensations * Temperature NOT transmitted by the tracts: * Pressure * Visualization * Pain * Audition * Fine touch * Olfaction * Crude touch * Gustation * Proprioception * Vibration Sensations Precise sensation Primitive sensation Fine touch Crude touch Pressure Pain Vibration Temperature Proprioception Other: sexual, itching, tickling Ascending tracts / Sensory tracts Dorsal coulmn Lat. Spinothalamic Ant. -
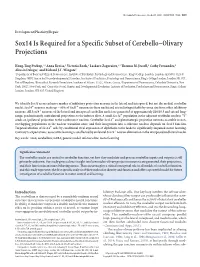
Sox14 Is Required for a Specific Subset of Cerebello–Olivary Projections
The Journal of Neuroscience, October 31, 2018 • 38(44):9539–9550 • 9539 Development/Plasticity/Repair Sox14 Is Required for a Specific Subset of Cerebello–Olivary Projections Hong-Ting Prekop,1,2 Anna Kroiss,1 Victoria Rook,2 Laskaro Zagoraiou,3,4 Thomas M. Jessell,4 Cathy Fernandes,5 Alessio Delogu,1 and Richard J.T. Wingate2 1Department of Basic and Clinical Neuroscience, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, SE5 9NU, United Kingdom, 2MRC Centre for Neurodevelopmental Disorders, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London SE1 1UL, United Kingdom, 3Biomedical Research Foundation Academy of Athens, 11527, Athens, Greece, 4Department of Neuroscience, Columbia University, New York, 10027, New York, and 5Centre for Social, Genetic and Developmental Psychiatry, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, SE5 8AF, United Kingdom We identify Sox14 as an exclusive marker of inhibitory projection neurons in the lateral and interposed, but not the medial, cerebellar nuclei. Sox14؉ neurons make up ϳ80% of Gad1؉ neurons in these nuclei and are indistinguishable by soma size from other inhibitory -neurons. All Sox14؉ neurons of the lateral and interposed cerebellar nuclei are generated at approximately E10/10.5 and extend long ”range, predominantly contralateral projections to the inferior olive. A small Sox14؉ population in the adjacent vestibular nucleus “Y -sends an ipsilateral projection to the oculomotor nucleus. Cerebellar -

The Superior and Inferior Colliculi of the Mole (Scalopus Aquaticus Machxinus)
THE SUPERIOR AND INFERIOR COLLICULI OF THE MOLE (SCALOPUS AQUATICUS MACHXINUS) THOMAS N. JOHNSON' Laboratory of Comparative Neurology, Departmmt of Amtomy, Un&versity of hfiehigan, Ann Arbor INTRODUCTION This investigation is a study of the afferent and efferent connections of the tectum of the midbrain in the mole (Scalo- pus aquaticus machrinus). An attempt is made to correlate these findings with the known habits of the animal. A subterranean animal of the middle western portion of the United States, Scalopus aquaticus machrinus is the largest of the genus Scalopus and its habits have been more thor- oughly studied than those of others of this genus according to Jackson ('15) and Hamilton ('43). This animal prefers a well-drained, loose soil. It usually frequents open fields and pastures but also is found in thin woods and meadows. Following a rain, new superficial burrows just below the surface of the ground are pushed in all directions to facili- tate the capture of worms and other soil life. Ten inches or more below the surface the regular permanent highway is constructed; the mole retreats here during long periods of dry weather or when frost is in the ground. The principal food is earthworms although, under some circumstances, larvae and adult insects are the more usual fare. It has been demonstrated conclusively that, under normal conditions, moles will eat vegetable matter. It seems not improbable that they may take considerable quantities of it at times. A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the University of Michigan. -

Basal Ganglia & Cerebellum
1/2/2019 This power point is made available as an educational resource or study aid for your use only. This presentation may not be duplicated for others and should not be redistributed or posted anywhere on the internet or on any personal websites. Your use of this resource is with the acknowledgment and acceptance of those restrictions. Basal Ganglia & Cerebellum – a quick overview MHD-Neuroanatomy – Neuroscience Block Gregory Gruener, MD, MBA, MHPE Vice Dean for Education, SSOM Professor, Department of Neurology LUHS a member of Trinity Health Outcomes you want to accomplish Basal ganglia review Define and identify the major divisions of the basal ganglia List the major basal ganglia functional loops and roles List the components of the basal ganglia functional “circuitry” and associated neurotransmitters Describe the direct and indirect motor pathways and relevance/role of the substantia nigra compacta 1 1/2/2019 Basal Ganglia Terminology Striatum Caudate nucleus Nucleus accumbens Putamen Globus pallidus (pallidum) internal segment (GPi) external segment (GPe) Subthalamic nucleus Substantia nigra compact part (SNc) reticular part (SNr) Basal ganglia “circuitry” • BG have no major outputs to LMNs – Influence LMNs via the cerebral cortex • Input to striatum from cortex is excitatory – Glutamate is the neurotransmitter • Principal output from BG is via GPi + SNr – Output to thalamus, GABA is the neurotransmitter • Thalamocortical projections are excitatory – Concerned with motor “intention” • Balance of excitatory & inhibitory inputs to striatum, determine whether thalamus is suppressed BG circuits are parallel loops • Motor loop – Concerned with learned movements • Cognitive loop – Concerned with motor “intention” • Limbic loop – Emotional aspects of movements • Oculomotor loop – Concerned with voluntary saccades (fast eye-movements) 2 1/2/2019 Basal ganglia “circuitry” Cortex Striatum Thalamus GPi + SNr Nolte. -

Toward a Common Terminology for the Gyri and Sulci of the Human Cerebral Cortex Hans Ten Donkelaar, Nathalie Tzourio-Mazoyer, Jürgen Mai
Toward a Common Terminology for the Gyri and Sulci of the Human Cerebral Cortex Hans ten Donkelaar, Nathalie Tzourio-Mazoyer, Jürgen Mai To cite this version: Hans ten Donkelaar, Nathalie Tzourio-Mazoyer, Jürgen Mai. Toward a Common Terminology for the Gyri and Sulci of the Human Cerebral Cortex. Frontiers in Neuroanatomy, Frontiers, 2018, 12, pp.93. 10.3389/fnana.2018.00093. hal-01929541 HAL Id: hal-01929541 https://hal.archives-ouvertes.fr/hal-01929541 Submitted on 21 Nov 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. REVIEW published: 19 November 2018 doi: 10.3389/fnana.2018.00093 Toward a Common Terminology for the Gyri and Sulci of the Human Cerebral Cortex Hans J. ten Donkelaar 1*†, Nathalie Tzourio-Mazoyer 2† and Jürgen K. Mai 3† 1 Department of Neurology, Donders Center for Medical Neuroscience, Radboud University Medical Center, Nijmegen, Netherlands, 2 IMN Institut des Maladies Neurodégénératives UMR 5293, Université de Bordeaux, Bordeaux, France, 3 Institute for Anatomy, Heinrich Heine University, Düsseldorf, Germany The gyri and sulci of the human brain were defined by pioneers such as Louis-Pierre Gratiolet and Alexander Ecker, and extensified by, among others, Dejerine (1895) and von Economo and Koskinas (1925). -

Neuronal Organization in the Inferior Colliculus Revisited with Cell-Type- Dependent Monosynaptic Tracing
This Accepted Manuscript has not been copyedited and formatted. The final version may differ from this version. Research Articles: Systems/Circuits Neuronal organization in the inferior colliculus revisited with cell-type- dependent monosynaptic tracing Chenggang Chen1, Mingxiu Cheng1,2, Tetsufumi Ito3 and Sen Song1 1Tsinghua Laboratory of Brain and Intelligence (THBI) and Department of Biomedical Engineering, Beijing Innovation Center for Future Chip, Center for Brain-Inspired Computing Research, McGovern Institute for Brain Research, Tsinghua University, Beijing, 100084, China 2National Institute of Biological Sciences, Beijing, 102206, China 3Anatomy II, School of Medicine, Kanazawa Medical University, Uchinada, Ishikawa, 920-0293, Japan DOI: 10.1523/JNEUROSCI.2173-17.2018 Received: 31 July 2017 Revised: 2 February 2018 Accepted: 7 February 2018 Published: 24 February 2018 Author contributions: C.C., T.I., and S.S. designed research; C.C. and M.C. performed research; C.C. and T.I. analyzed data; C.C. wrote the first draft of the paper; C.C., T.I., and S.S. edited the paper; C.C., T.I., and S.S. wrote the paper. Conflict of Interest: The authors declare no competing financial interests. This work was supported by funding from the National Natural Science Foundation of China (31571095, 91332122, for S.S.), Special Fund of Suzhou-Tsinghua Innovation Leading Action (for S.S.), Beijing Program on the Study of Brain-Inspired Computing System and Related Core Technologies (for S.S.), Beijing Innovation Center for Future Chip (for S.S.), and Chinese Academy of Sciences Institute of Psychology Key Laboratory of Mental Health Open Research Grant (KLMH2012K02, for S.S.), grants from Ministry of Education, Science, and Culture of Japan (KAKENHI grant, Grant numbers 16K07026 and 16H01501; for T.I.), and Takahashi Industrial and Economic Research Foundation (for T.I.). -
L4-Physiology of Motor Tracts.Pdf
: chapter 55 page 667 Objectives (1) Describe the upper and lower motor neurons. (2) Understand the pathway of Pyramidal tracts (Corticospinal & corticobulbar tracts). (3) Understand the lateral and ventral corticospinal tracts. (4) Explain functional role of corticospinal & corticobulbar tracts. (5) Describe the Extrapyramidal tracts as Rubrospinal, Vestibulospinal, Reticulospinal and Tectspinal Tracts. The name of the tract indicate its pathway, for example Corticobulbar : Terms: - cortico: cerebral cortex. Decustation: crossing. - Bulbar: brainstem. Ipsilateral : same side. *So it starts at cerebral cortex and Contralateral: opposite side. terminate at the brainstem. CNS influence the activity of skeletal muscle through two set of neurons : 1- Upper motor neurons (UMN) 2- lower motor neuron (LMN) They are neurons of motor cortex & their axons that pass to brain stem and They are Spinal motor neurons in the spinal spinal cord to activate: cord & cranial motor neurons in the brain • cranial motor neurons (in brainstem) stem which innervate muscles directly. • spinal motor neurons (in spinal cord) - These are the only neurons that innervate - Upper motor neurons (UMN) are the skeletal muscle fibers, they function as responsible for conveying impulses for the final common pathway, the final link voluntary motor activity through between the CNS and skeletal muscles. descending motor pathways that make up by the upper motor neurons. Lower motor neurons are classified based on the type of muscle fiber the innervate: There are two UMN Systems through which 1- alpha motor neurons (UMN) control (LMN): 2- gamma motor neurons 1- Pyramidal system (corticospinal tracts ). 2- Extrapyramidal system The activity of the lower motor neuron (LMN, spinal or cranial) is influenced by: 1. -

Mir-124 Regulates Early Neurogenesis in the Optic Vesicle and Forebrain, Targeting Neurod1
Published online 3 December 2010 Nucleic Acids Research, 2011, Vol. 39, No. 7 2869–2879 doi:10.1093/nar/gkq904 MiR-124 regulates early neurogenesis in the optic vesicle and forebrain, targeting NeuroD1 Kaili Liu1,2,3, Ying Liu1,2,*, Weichuan Mo1,3, Rong Qiu1, Xiumei Wang1,2, Jane Y. Wu1,4 and Rongqiao He1,3,5,* 1The State Key Laboratory of Brain and Cognitive Science, 2Key Laboratory of Noncoding RNA, Institute of Biophysics, Chinese Academy of Sciences, 15 Datun Road, Chaoyang District, Beijing 100101, 3Graduate University of Chinese Academy of Sciences, Beijing 100049, China, 4Department of Neurology, Lurie Comprehensive Cancer Center, Center for Genetic Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL 60611, USA and 5Key Laboratory of Mental Health, Chinese Academy of Sciences, Beijing 100101, China Received April 23, 2010; Revised September 5, 2010; Accepted September 23, 2010 ABSTRACT post-transcriptional mechanisms controlling their expres- sion are poorly understood. In recent years, systematic MicroRNAs (miRNAs) are involved in the fine control studies in zebrafish and mouse have determined specific of cell proliferation and differentiation during the microRNAs (miRNAs) expressed in the developing eye development of the nervous system. MiR-124, a and brain (1,2). MiR-7 and let-7 have been shown to be neural specific miRNA, is expressed from the begin- involved in Drosophila eye development (3,4). In Xenopus, ning of eye development in Xenopus, and has been miR-24a has been reported to play an essential role in shown to repress cell proliferation in the optic cup, repressing apoptosis in the developing neural retina (5). -

Functional MRI, DTI and Neurophysiology in Horizontal Gaze Palsy with Progressive Scoliosis
Neuroradiology (2008) 50:453–459 DOI 10.1007/s00234-007-0359-1 FUNCTIONAL NEURORADIOLOGY Functional MRI, DTI and neurophysiology in horizontal gaze palsy with progressive scoliosis Sven Haller & Stephan G. Wetzel & Jürg Lütschg Received: 19 August 2007 /Accepted: 14 December 2007 /Published online: 24 January 2008 # Springer-Verlag 2008 Abstract suspected HGPPS, any technique appears appropriate for Introduction Horizontal gaze palsy with progressive scoliosis further investigation. Auditory fMRI suggests that a (HGPPS) is an autosomal recessive disease due to a mutation monaural auditory system with bilateral auditory activations in the ROBO3 gene. This rare disease is of particular interest might be a physiological advantage as compared to a because the absence, or at least reduction, of crossing of the binaural yet only unilateral auditory system, in analogy to ascending lemniscal and descending corticospinal tracts in the anisometropic amblyopia. Moving-head fMRI studies in the medulla predicts abnormal ipsilateral sensory and motor future might show whether the compensatory head move- systems. ments instead of normal eye movements activate the eye- Methods We evaluated the use of functional magnetic movement network. resonance imaging (fMRI) for the first time in this disease and compared it to diffusion tensor imaging (DTI) Keywords Functional MRI . HGPPS . ROBO3 tractography and neurophysiological findings in the same patient with genetically confirmed ROBO3 mutation. Abbreviations Results As expected, motor fMRI, somatosensory evoked BAEP brainstem auditory evoked potentials potentials (SSEP) and motor evoked potentials (MEP) were BOLD blood oxygenation level dependent dominantly ipsilateral to the stimulation side. DTI tractography DTI diffusion tensor imaging revealed ipsilateral ascending and descending connectivity in fMRI functional magnetic resonance imaging the brainstem yet normal interhemispheric connections in the FEF frontal eye field corpus callosum.