Rare Disease Registries in Europe
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
CADASIL Testing
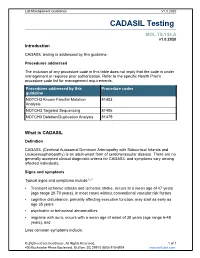
Lab Management Guidelines V1.0.2020 CADASIL Testing MOL.TS.144.A v1.0.2020 Introduction CADASIL testing is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline NOTCH3 Known Familial Mutation 81403 Analysis NOTCH3 Targeted Sequencing 81406 NOTCH3 Deletion/Duplication Analysis 81479 What is CADASIL Definition CADASIL (Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy) is an adult-onset form of cerebrovascular disease. There are no generally accepted clinical diagnostic criteria for CADASIL and symptoms vary among affected individuals. Signs and symptoms Typical signs and symptoms include1,2,3 Transient ischemic attacks and ischemic stroke, occurs at a mean age of 47 years (age range 20-70 years), in most cases without conventional vascular risk factors cognitive disturbance, primarily affecting executive function, may start as early as age 35 years psychiatric or behavioral abnormalities migraine with aura, occurs with a mean age of onset of 30 years (age range 6-48 years), and Less common symptoms include: © 2020 eviCore healthcare. All Rights Reserved. 1 of 7 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2020 recurrent seizures with onset in middle age, usually secondary to stroke acute encephalopathy, with a mean age of onset of 42 years Life expectancy for men with CADASIL is reduced by approximately five years and for women by 1 to 2 years.4 Diagnosis Brain Magnetic Resonance Imaging (MRI) findings include T2-signal-abnormalities in the white matter of the temporal pole and T2-signal-abnormalities in the external capsule and corpus callosum.1,2 CADASIL is suspected in an individual with the clinical signs and MRI findings. -

Glossary for Narrative Writing
Periodontal Assessment and Treatment Planning Gingival description Color: o pink o erythematous o cyanotic o racial pigmentation o metallic pigmentation o uniformity Contour: o recession o clefts o enlarged papillae o cratered papillae o blunted papillae o highly rolled o bulbous o knife-edged o scalloped o stippled Consistency: o firm o edematous o hyperplastic o fibrotic Band of gingiva: o amount o quality o location o treatability Bleeding tendency: o sulcus base, lining o gingival margins Suppuration Sinus tract formation Pocket depths Pseudopockets Frena Pain Other pathology Dental Description Defective restorations: o overhangs o open contacts o poor contours Fractured cusps 1 ww.links2success.biz [email protected] 914-303-6464 Caries Deposits: o Type . plaque . calculus . stain . matera alba o Location . supragingival . subgingival o Severity . mild . moderate . severe Wear facets Percussion sensitivity Tooth vitality Attrition, erosion, abrasion Occlusal plane level Occlusion findings Furcations Mobility Fremitus Radiographic findings Film dates Crown:root ratio Amount of bone loss o horizontal; vertical o localized; generalized Root length and shape Overhangs Bulbous crowns Fenestrations Dehiscences Tooth resorption Retained root tips Impacted teeth Root proximities Tilted teeth Radiolucencies/opacities Etiologic factors Local: o plaque o calculus o overhangs 2 ww.links2success.biz [email protected] 914-303-6464 o orthodontic apparatus o open margins o open contacts o improper -

Oral Health in Prevalent Types of Ehlers–Danlos Syndromes
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Ghent University Academic Bibliography J Oral Pathol Med (2005) 34: 298–307 ª Blackwell Munksgaard 2005 Æ All rights reserved www.blackwellmunksgaard.com/jopm Oral health in prevalent types of Ehlers–Danlos syndromes Peter J. De Coster1, Luc C. Martens1, Anne De Paepe2 1Department of Paediatric Dentistry, Centre for Special Care, Paecamed Research, Ghent University, Ghent; 2Centre for Medical Genetics, Ghent University Hospital, Ghent, Belgium BACKGROUND: The Ehlers–Danlos syndromes (EDS) Introduction comprise a heterogenous group of heritable disorders of connective tissue, characterized by joint hypermobility, The Ehlers–Danlos syndromes (EDS) comprise a het- skin hyperextensibility and tissue fragility. Most EDS erogenous group of heritable disorders of connective types are caused by mutations in genes encoding different tissue, largely characterized by joint hypermobility, skin types of collagen or enzymes, essential for normal pro- hyperextensibility and tissue fragility (1) (Fig. 1). The cessing of collagen. clinical features, modes of inheritance and molecular METHODS: Oral health was assessed in 31 subjects with bases differ according to the type. EDS are caused by a EDS (16 with hypermobility EDS, nine with classical EDS genetic defect causing an error in the synthesis or and six with vascular EDS), including signs and symptoms processing of collagen types I, III or V. The distribution of temporomandibular disorders (TMD), alterations of and function of these collagen types are displayed in dental hard tissues, oral mucosa and periodontium, and Table 1. At present, two classifications of EDS are was compared with matched controls. -

The National Economic Burden of Rare Disease Study February 2021
Acknowledgements This study was sponsored by the EveryLife Foundation for Rare Diseases and made possible through the collaborative efforts of the national rare disease community and key stakeholders. The EveryLife Foundation thanks all those who shared their expertise and insights to provide invaluable input to the study including: the Lewin Group, the EveryLife Community Congress membership, the Technical Advisory Group for this study, leadership from the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health (NIH), the Undiagnosed Diseases Network (UDN), the Little Hercules Foundation, the Rare Disease Legislative Advocates (RDLA) Advisory Committee, SmithSolve, and our study funders. Most especially, we thank the members of our rare disease patient and caregiver community who participated in this effort and have helped to transform their lived experience into quantifiable data. LEWIN GROUP PROJECT STAFF Grace Yang, MPA, MA, Vice President Inna Cintina, PhD, Senior Consultant Matt Zhou, BS, Research Consultant Daniel Emont, MPH, Research Consultant Janice Lin, BS, Consultant Samuel Kallman, BA, BS, Research Consultant EVERYLIFE FOUNDATION PROJECT STAFF Annie Kennedy, BS, Chief of Policy and Advocacy Julia Jenkins, BA, Executive Director Jamie Sullivan, MPH, Director of Policy TECHNICAL ADVISORY GROUP Annie Kennedy, BS, Chief of Policy & Advocacy, EveryLife Foundation for Rare Diseases Anne Pariser, MD, Director, Office of Rare Diseases Research, National Center for Advancing Translational Sciences (NCATS), National Institutes of Health Elisabeth M. Oehrlein, PhD, MS, Senior Director, Research and Programs, National Health Council Christina Hartman, Senior Director of Advocacy, The Assistance Fund Kathleen Stratton, National Academies of Science, Engineering and Medicine (NASEM) Steve Silvestri, Director, Government Affairs, Neurocrine Biosciences Inc. -

COVID-19 Vaccine Janssen: Contraindication in Individuals with Previous Capillary Leak Syndrome and Update on Thrombosis with Thrombocytopenia Syndrome
Janssen Sciences Ireland UC Address: Airton Road, Tallaght, D24 WR89 Tel: +353 1 466 5200 Fax: +353 1 431 1058 www.janssen.ie 19the July 2021 COVID-19 Vaccine Janssen: Contraindication in individuals with previous capillary leak syndrome and update on thrombosis with thrombocytopenia syndrome Dear Healthcare Professional, Janssen-Cilag International NV in agreement with the European Medicines Agency and the Health Products Regulatory Authority (HPRA) would like to inform you of the following: Summary Capillary leak syndrome (CLS): • Very rare cases of capillary leak syndrome (CLS) have been reported in the first days after vaccination with COVID-19 Vaccine Janssen, in some cases with a fatal outcome. A history of CLS has been reported in at least one case. • COVID-19 Vaccine Janssen is now contraindicated in individuals who have previously experienced episodes of CLS. • CLS is characterised by acute episodes of oedema mainly affecting the limbs, hypotension, haemoconcentration and hypoalbuminaemia. Patients with an acute episode of CLS following vaccination require prompt recognition and treatment. Intensive supportive therapy is usually warranted. Thrombosis with thrombocytopenia syndrome (TTS): • Individuals diagnosed with thrombocytopenia within 3 weeks after vaccination with COVID-19 Vaccine Janssen should be actively investigated for signs of thrombosis. Similarly, individuals who present with thrombosis within 3 weeks of vaccination should be evaluated for thrombocytopenia. • TTS requires specialised clinical management. Healthcare professionals should consult applicable guidance and/ or consult specialists (e.g., haematologists, specialists in coagulation) to diagnose and treat this condition. Background on the safety concern COVID-19 Vaccine Janssen suspension for injection is indicated for active immunisation to prevent COVID-19 caused by SARS-CoV-2, in individuals 18 years of age and older. -

Non-Syndromic Occurrence of True Generalized Microdontia with Mandibular Mesiodens - a Rare Case Seema D Bargale* and Shital DP Kiran
Bargale and Kiran Head & Face Medicine 2011, 7:19 http://www.head-face-med.com/content/7/1/19 HEAD & FACE MEDICINE CASEREPORT Open Access Non-syndromic occurrence of true generalized microdontia with mandibular mesiodens - a rare case Seema D Bargale* and Shital DP Kiran Abstract Abnormalities in size of teeth and number of teeth are occasionally recorded in clinical cases. True generalized microdontia is rare case in which all the teeth are smaller than normal. Mesiodens is commonly located in maxilary central incisor region and uncommon in the mandible. In the present case a 12 year-old boy was healthy; normal in appearance and the medical history was noncontributory. The patient was examined and found to have permanent teeth that were smaller than those of the average adult teeth. The true generalized microdontia was accompanied by mandibular mesiodens. This is a unique case report of non-syndromic association of mandibular hyperdontia with true generalized microdontia. Keywords: Generalised microdontia, Hyperdontia, Permanent dentition, Mandibular supernumerary tooth Introduction [Ullrich-Turner syndrome], Chromosome 13[trisomy 13], Microdontia is a rare phenomenon. The term microdontia Rothmund-Thomson syndrome, Hallermann-Streiff, Oro- (microdentism, microdontism) is defined as the condition faciodigital syndrome (type 3), Oculo-mandibulo-facial of having abnormally small teeth [1]. According to Boyle, syndrome, Tricho-Rhino-Phalangeal, type1 Branchio- “in general microdontia, the teeth are small, the crowns oculo-facial syndrome. short, and normal contact areas between the teeth are fre- Supernumerary teeth are defined as any supplementary quently missing” [2] Shafer, Hine, and Levy [3] divided tooth or tooth substance in addition to usual configuration microdontia into three types: (1) Microdontia involving of twenty deciduous and thirty two permanent teeth [7]. -

Spectrum of PEX1 and PEX6 Variants in Heimler Syndrome
European Journal of Human Genetics (2016) 24, 1565–1571 Official Journal of The European Society of Human Genetics www.nature.com/ejhg ARTICLE Spectrum of PEX1 and PEX6 variants in Heimler syndrome Claire EL Smith1, James A Poulter1, Alex V Levin2,3,4, Jenina E Capasso4, Susan Price5, Tamar Ben-Yosef6, Reuven Sharony7, William G Newman8,9, Roger C Shore10, Steven J Brookes10, Alan J Mighell1,11,12 and Chris F Inglehearn*,1,12 Heimler syndrome (HS) consists of recessively inherited sensorineural hearing loss, amelogenesis imperfecta (AI) and nail abnormalities, with or without visual defects. Recently HS was shown to result from hypomorphic mutations in PEX1 or PEX6,both previously implicated in Zellweger Syndrome Spectrum Disorders (ZSSD). ZSSD are a group of conditions consisting of craniofacial and neurological abnormalities, sensory defects and multi-organ dysfunction. The finding of HS-causing mutations in PEX1 and PEX6 shows that HS represents the mild end of the ZSSD spectrum, though these conditions were previously thought to be distinct nosological entities. Here, we present six further HS families, five with PEX6 variants and one with PEX1 variants, and show the patterns of Pex1, Pex14 and Pex6 immunoreactivity in the mouse retina. While Ratbi et al. found more HS-causing mutations in PEX1 than in PEX6, as is the case for ZSSD, in this cohort PEX6 variants predominate, suggesting both genes play a significant role in HS. The PEX6 variant c.1802G4A, p.(R601Q), reported previously in compound heterozygous state in one HS and three ZSSD cases, was found in compound heterozygous state in three HS families. -

Advances in Understanding the Genetics of Syndromes Involving Congenital Upper Limb Anomalies
Review Article Page 1 of 10 Advances in understanding the genetics of syndromes involving congenital upper limb anomalies Liying Sun1#, Yingzhao Huang2,3,4#, Sen Zhao2,3,4, Wenyao Zhong1, Mao Lin2,3,4, Yang Guo1, Yuehan Yin1, Nan Wu2,3,4, Zhihong Wu2,3,5, Wen Tian1 1Hand Surgery Department, Beijing Jishuitan Hospital, Beijing 100035, China; 2Beijing Key Laboratory for Genetic Research of Skeletal Deformity, Beijing 100730, China; 3Medical Research Center of Orthopedics, Chinese Academy of Medical Sciences, Beijing 100730, China; 4Department of Orthopedic Surgery, 5Department of Central Laboratory, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing 100730, China Contributions: (I) Conception and design: W Tian, N Wu, Z Wu, S Zhong; (II) Administrative support: All authors; (III) Provision of study materials or patients: All authors; (IV) Collection and assembly of data: Y Huang; (V) Data analysis and interpretation: L Sun; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Wen Tian. Hand Surgery Department, Beijing Jishuitan Hospital, Beijing 100035, China. Email: [email protected]. Abstract: Congenital upper limb anomalies (CULA) are a common birth defect and a significant portion of complicated syndromic anomalies have upper limb involvement. Mostly the mortality of babies with CULA can be attributed to associated anomalies. The cause of the majority of syndromic CULA was unknown until recently. Advances in genetic and genomic technologies have unraveled the genetic basis of many syndromes- associated CULA, while at the same time highlighting the extreme heterogeneity in CULA genetics. Discoveries regarding biological pathways and syndromic CULA provide insights into the limb development and bring a better understanding of the pathogenesis of CULA. -

Capillary Leak Syndrome
The Medicine Forum Volume 17 Article 8 2016 Case Report: Uncontrolled Anasarca: Capillary Leak Syndrome Ankita Mehta, MD Thomas Jefferson University Hospital, [email protected] Mansi Shah, MD Jefferson Hospital Ambulatory Practice, Thomas Jefferson University Hospital, [email protected] Follow this and additional works at: https://jdc.jefferson.edu/tmf Part of the Internal Medicine Commons, and the Oncology Commons Let us know how access to this document benefits ouy Recommended Citation Mehta, MD, Ankita and Shah, MD, Mansi (2016) "Case Report: Uncontrolled Anasarca: Capillary Leak Syndrome," The Medicine Forum: Vol. 17 , Article 8. DOI: https://doi.org/10.29046/TMF.017.1.009 Available at: https://jdc.jefferson.edu/tmf/vol17/iss1/8 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in The Medicine Forum by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Mehta, MD and Shah, MD: Case Report: Uncontrolled Anasarca: Capillary Leak Syndrome ONCOLOGY Case Report: Uncontrolled Anasarca: Capillary Leak Syndrome Ankita Mehta, MD, and Mansi Shah, MD INTRODUCTION progression of her pancreatic cancer. She was ultimately discharged home with hospice care. -

Saethre-Chotzen Syndrome
Saethre-Chotzen syndrome Authors: Professor L. Clauser1 and Doctor M. Galié Creation Date: June 2002 Update: July 2004 Scientific Editor: Professor Raoul CM. Hennekam 1Department of craniomaxillofacial surgery, St. Anna Hospital and University, Corso Giovecca, 203, 44100 Ferrara, Italy. [email protected] Abstract Keywords Disease name and synonyms Excluded diseases Definition Prevalence Management including treatment Etiology Diagnostic methods Genetic counseling Antenatal diagnosis Unresolved questions References Abstract Saethre-Chotzen Syndrome (SCS) is an inherited craniosynostotic condition, with both premature fusion of cranial sutures (craniostenosis) and limb abnormalities. The most common clinical features, present in more than a third of patients, consist of coronal synostosis, brachycephaly, low frontal hairline, facial asymmetry, hypertelorism, broad halluces, and clinodactyly. The estimated birth incidence is 1/25,000 to 1/50,000 but because the phenotype can be very mild, the entity is likely to be underdiagnosed. SCS is inherited as an autosomal dominant trait with a high penetrance and variable expression. The TWIST gene located at chromosome 7p21-p22, is responsible for SCS and encodes a transcription factor regulating head mesenchyme cell development during cranial tube formation. Some patients with an overlapping SCS phenotype have mutations in the FGFR3 (fibroblast growth factor receptor 3) gene; especially the Pro250Arg mutation in FGFR3 (Muenke syndrome) can resemble SCS to a great extent. Significant intrafamilial -

Molecular Delineation of Small Supernumerary Marker
Zhou et al. Molecular Cytogenetics (2020) 13:19 https://doi.org/10.1186/s13039-020-00486-2 RESEARCH Open Access Molecular delineation of small supernumerary marker chromosomes using a single nucleotide polymorphism array Lili Zhou1, Zhaoke Zheng1, Lianpeng Wu2, Chenyang Xu1, Hao Wu1, Xueqin Xu1 and Shaohua Tang1,2* Abstract Background: Defining the phenotype-genotype correlation of small supernumerary marker chromosomes (sSMCs) remains a challenge in prenatal diagnosis. We karyotyped 20,481 amniotic fluid samples from pregnant women and explored the molecular characteristics of sSMCs using a single nucleotide polymorphism (SNP) array. Results: Out of the 20,481 samples, 15 abnormal karyotypes with sSMC were detected (frequency: 0.073%) and the chromosomal origin was successfully identified by SNP array in 14 of them. The origin of sSMCs were mainly acrocentric-derived chromosomes and the Y chromosome. Two cases of sSMC combined with uniparental disomy (UPD) were detected, UPD(1) and UPD(22). More than half of the cases of sSMC involved mosaicism (8/15) and pathogenicity (9/15) in prenatal diagnosis. A higher prevalence of mosaicism for non-acrocentric chromosomes than acrocentric chromosomes was also revealed. One sSMC derived from chromosome 3 with a neocentromere revealed a 24.99-Mb pathogenic gain of the 3q26.31q29 region on the SNP array, which presented as an abnormal ultrasound indicating nasal bone hypoplasia. Conclusion: The clinical phenotypes of sSMCs are variable and so further genetic testing and parental karyotype analysis are needed to confirm the characteristics of sSMCs. The SNP array used here allows a detailed characterisation of the sSMC and establishes a stronger genotype-phenotype correlation, thus allowing detailed genetic counselling for prenatal diagnosis. -

MEDICAL GENETICS RESIDENCY PROGRAM Department of Pediatrics
MEDICAL GENETICS RESIDENCY PROGRAM Department of Pediatrics University of Michigan Health Systems (734) 763-6767 1500 E. Medical Center Drive (734) 763-6561 (fax) D5240 MPB Ann Arbor, MI 48109-5718 Biochemical Genetics Goals and Objectives Director: Drs. Ayesha Ahmad and Shane C. Quinonez The goals and objectives of the Biochemical Genetics Clinic rotation in the Medical Genetics Residency Program are to provide the resident with exposure to all aspects of care of metabolic disease and counseling in accordance with the Residency Review Committee for Medical Genetics expectations and to fulfill criteria for board eligibility by the American Board of Medical Genetics. Patient Care The resident will become familiar with the evaluation, diagnosis and management of urea cycle disorders, organic acidemias, disorders of carbohydrate and lipid metabolism and numerous other inborn errors of metabolism (IEMs). Residents will gain exposure in performing and expertise in interpreting biochemical analyses relevant to the diagnosis and management of human genetic diseases. By the end of the rotation the resident should be able to identify signs and symptoms of IEMs, formulate a differential diagnosis, order appropriate tests and recognize normal variants and complex patterns of metabolites. Residents will be able to manage acute metabolic crises and provide chronic management of patients with an IEM. Residents should be able to interpret NBS results, collaborate with the primary provider to act upon results in a timely manner, develop a differential diagnosis and order appropriate confirmatory testing and communicate results to families. Medical Knowledge Through coursework and didactic sessions with attending physicians, residents will become familiar with fundamental concepts, molecular biology and biochemistry relevant to IEMs.