Federal University Hospitals and Stochastic Frontier Model
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Health Professions Act: List of Approved Facilities for Purposes Of
114 No. 36936 GOVERNMENT GAZETTE, 16 OCTOBER 2013 No. 797 16 October 2017 HEALTH PROFESSIONS ACT, 1974 (ACT NO. 56 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY SPEECH LANGUAGE AND HEARING THERAPISTS IN THE YEAR 2014 The Minister of Health has, in terms of regulation 5.1 of the Regulations relating to Performance of Community Service by Persons Registering in terms of the Health Professions Act, 1974 (Act No. 56 of 1974), listed the following approved facilities for purposes of the profession of speech and hearing therapy. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE AMATOLE (Allocated professionals to rotate within the cluster) Buffalo City/Amahlathi Cluster Bhisho Hospital Cathcart Hospital Grey Hospital* Nompumelelo Hospital * S.S GidaHospital* East London Complex Cecilia Makiwane Hospital Empilweni Gompo Hospital Frere Hospital Bedfort Hospital Nkonkobe Cluster Fort Beaufort Hospital Victoria Hospital Tower Hospital(Psychiatry Hospital) Mbashe Cluster Madwaleni Hospital Butterworth Hospital Mnquma Cluster Ngqamakhwe CHC Tafalofefe Hospital ALFRED NZO (Allocated professionals to rotate within the cluster) Maluti Cluster Taylor Bequest(Matatiele) Umzimvubu Cluster Madzikane kaZulu Hospital Mt.Ayliff Hospital Sipetu Hospital CACADU (Allocated professionals to rotate within the cluster This gazette is also available free online at www.gpwonline.co.za STAATSKOERANT, 16 OKTOBER 2013 No. 36936 115 Cambedoo Cluster Andries Vosloo Hospital Midlands Hospital Kouga Cluster Humansdorp Hospital Makana -

Health Professions Act: List of Approved Facilities for the Purposes
STAATSKOERANT, 16 OKTOBER 2013 No. 36936 39 No. 791 16 October 2013 HEALTH PROFESSIONS ACT, 1974 (ACT NO. 56 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY MEDICAL PRACTITIONERS IN THE YEAR 2014 The Minister of Health has, in terms of regulation 5.1 of the Regulations relating to Performance of Community Service by Persons Registering in terms of the Health Professions Act, 1974 (Act No. 56 of 1974), listed the following approved facilities for purposes of the profession of medicine. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE Alfred Nzo Khotsong Hospital* Madzikane kaZulu Hospital ** Umzimvubu Cluster Mt Ayliff Hospital** Taylor Bequest Hospital* (Matatiele) Amathole Bhisho CHH Cathcart Hospital * Amahlathi/Buffalo City Cecilia Makiwane Hospital Cluster Dimbaza CHC Duncan Village Day Hospital Empilweni Gompo CHC Fort Grey TB Hospital Frere Hospital Grey Hospital * Komga Hospital Nkqubela TB Hospital Nompumelelo Hospital* SS Gida Hospital* Stutterheim FPA Hospital* Mnquma Sub-District Butterworth Hospital* Nqgamakwe CHC* Nkonkobe Sub-District Adelaide FPA Hospital Tower Hospital* Victoria Hospital * Mbashe /KSD District Elliotdale CHC* Idutywa CHC* Madwaleni Hospital* Chris Hani All Saints Hospital** Engcobo/IntsikaYethu Cofimvaba Hospital** Martjie Venter FPA Hospital This gazette is also available free online at www.gpwonline.co.za 40 No. 36936 GOVERNMENT GAZETTE, 16 OCTOBER 2013 Sub-District Mjanyana Hospital * InxubaYethembaSub-Cradock Hospital** Wilhelm Stahl Hospital** District Inkwanca -
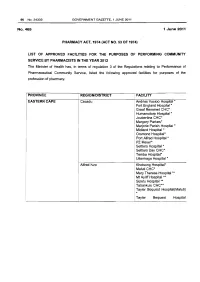
Health Professions Act: List of Approved Facilities for Community Service by Pharmacists in 2012
96 No.34332 GOVERNMENT GAZETTE, 1 JUNE 2011 No.465 1 June 2011 PHARMACY ACT, 1974 (ACT NO. 53 OF 1974} LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY PHARMACISTS IN THE YEAR 2012 The Minister of Health has, in terms of regulation 3 of the Regulations relating to Performance of Pharmaceutical Community Service, listed the following approved facilities for purposes of the profession of pharmacy. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE Cacadu Andries Vosloo Hospital * Fort England Hospital* Graaf Reneinet CHC* Humansdorp Hospital * Joubertina CHC* Margery Parkes* Marjorie Parish Hospital* Midland Hospital * Orsmond Hospital* Port Alfred Hospital * PZ Meyer* Settlers Hospital * Settlers Day CHC* Temba Hospital• Uitenhage Hospital * Alfred Nzo Khotsong Hospital• Maluti CHC* Mary Theresa Hospital .... ! Mt Ayliff Hospital ** · Sipetu Hospital •• Tabankulu CHC*• Tayler Bequest Hospitai(Maluti) * Tayler Bequest Hospital STAATSKOERANT, 1 JUNIE 2011 No. 34332 97 (Matatiele )"' Chris Hani All Saints Hospital ..... Cala Hospital ** Cofimvaba Hospital ** Cradock Hospital ** Elliot Hospital ... Frontier Hospital * Glen Grey Hospital * Mjanyana Hospital ** NgcoboCHC* Ngonyama CHC* Nomzamo CHC* Sada CHC* Thornhill CHC* Wilhelm Stahl Hospital ..... ZwelakheDalasile CHC* Nelson Mandala Dora Nginza Hospital Elizabeth Donkin Hospital Jose Pearson Santa Hospital Kwazakhele Day Clinic Laetitia Bam CH C Livingstone Hospital Motherwell CHC New Brighton CHC PE Pharmaceutical Depot PE Provincial Hospital Amathole Bedford Hospital Bhisho Hospital Butterworth Hospital Cecilia Makiwane Hospital Cathcart Hospital Dimbaza CHC Duncan Village Day CHC Dutywa CHC Empilweni Gompo CHC Fort Beauford Hospital Fort Grey Hospital Frere Hospital Grey Hospital Middledrift CHC Nontyatyambo CHC Nompomelelo Hospital Ngqamakwe CHC SS Gida Hospita Tafalofefe Hospital Tower Hospital Victoria Hospital Winterberg Hospital Willowvale CHC 98 No. -

Health Professions Act: List of Approved Facilities for Purposes Of
40 No. 35624 GOVERNMENT GAZETTE, 27 AUGUST 2012 No. 676 27 August 2012 HEALTH PROFESSIONS ACT, 1974 (ACT NO. 56 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY MEDICAL PRACTITIONERS IN THE YEAR 2013 The Minister of Health has, in terms of regulation 5.1 of the Regulations relating to Performance of Community Service by Persons Registering in terms of the Health Professions Act, 1974 (Act No. 56 of 1974), listed the following facilities for purposes of the profession of medicine. PROVINCE REGION/DISTRICT FACILITY EASTERN CAPE Alfred Nzo Khotsong Hospital* Madzikane kaZulu Hospital ** Umzimvubu Cluster Mt Ayliff Hospital ** Taylor Bequest Hospital* (Matatiele) Amato le Cathcart Hospital * Cecilia Makiwane Hospital Amahlathi/Buffalo City Dimbaza CHC Cluster Fort Grey TB Hospital Grey Hospital * Komga Hospital Nkqubela TB Hospital Nompumelelo Hospital* SS Gida Hospital* Stutterheim FPA Hospital* Mnquma Sub-District Butterworth Hospital* Nqgamakhwe CHC* Nkonkobe Sub-District Adelaide FPA Hospital Tower Hospital* Victoria Hospital * Mbashe /KSD District Elliotdale CHC* Idutywa CHC* Madwaleni Hospital* Zitulele Hospital * Chris Hani All Saints Hospital ** Cofimvaba Hospital ** Engcobo/IntsikaYethu Martjie Venter FPA Hospital Sub-District Mjanyana Hospital * STAATSKOERANT, 27 AUGUSTUS 2012 No. 35624 41 lnxubaYethemba Sub-Cradock Hospital ** Wilhelm Stahl Hospital ** District Inkwanca Molteno FPA Hospital Lukhanji Frontier Hospital* Hewu Hospital * Komani Hospital* Sakhisizwe/Emalahleni Cala Hospital ** Dordrecht FPA Hospital Glen Grey Hospital ** Indwe FPA Hospital Ngonyama CHC* Nelson Mandela Metro Dora Nginza Hospital Empilweni TB Hospital PE Metro Jose Pearson TB Hospital Orsmond TB Hospital Letticia Barn CHC PE Provincial Uitenhage Hospital Kouga Sub-District Humansdorp Hospital BJ Voster FPA Hospital O.R.Tambo Dr Lizo Mpehle Memorial Hospital ** Nessie Knight Hospital ** Mhlontlo Sub-District Qaukeni North Sub-Greenville Hospital ** Holly Cross Hospital ** District Isipethu Hospital* Port St Johns CHC* St. -

Frontier Nursing Service, 1925-1940
CULTURE AND THE PROVISION OF CARE: FRONTIER NURSING SERVICE 1925-1940 by Barbara Ann Criss A dissertation submitted to the faculty of The University of Utah in partial fulfillment of the requirements for the degree of Doctor of Philosophy Department of Nursing The University of Utah August 1988 THE UNIVERSITY OF UTAH GRADUATE SCHOOL SUPERVISORY COlVIlVIITrrEE APPROVAL of a dissertation submitted by Barbara Ann criss This dissertation has beel! read by each melllber of the following supervisory committee alld by majority vote has been found to be satisfactory. Chair: Patr �cia C. Albers Ronald G. Coleman 19t 7 IfI THE Ur\!VERSITY OF l'TAH GRADUATE SCHOOL FINAL READING APPROVAL To the Graduate Council of The Universitv of Utah: Barbara Ann Criss I have read the dissertation of in its final form and have found that (1) its format, citations, and bibliographic style are consistent and acceptable; (2) its illustrative materials including figures, tables, and charts are in place; and (3) the final manuscript is satisfactorr to the Supervis ory Committee and is ready for submission to the Graduate School. J / rl·I · f� Chairpenon. Supervisory Committee Approved for the Major Department Linda K. Amos Chairman I Dean Approved for the Graduate Council B. Gale Dick Dean or The Graduate School Copyright © Barbara Ann Criss 1988 All Rights Reserved ABSTRACT The purpose of this ethnohistorical research was to study the first fifteen years of the Frontier Nursing Service in Hyden, Kentucky, the years 1925 to 1940. This time span was chosen for several reasons. First, the founding of the Kentucky Committee for Mothers and Babies (the name was changed to Frontier Nursing Service in 1928) occurred in 1925. -

Cohsasa News Sept 06
CohsasaThe Newsletter The Council for Health Service Accreditation of Southern Africa TECHNOLOGY UPDATE OCTOBER 2006 New information system is a treasure map COHSASA – in partnership with Xylaco Software – has developed a unique application, which will provide a 360-degree view of strengths, weaknesses and Ten South African urgent improvements needed in health facilities enrolled in COHSASA’s quality hospices accredited improvement and accreditation programmes. Ten hospices in the country, all members of the Hospice Palliative Care Association of Examining 37 areas of operation and measuring both clinical and non- South Africa, have been accredited clinical performance indicators, the new database, migrated from for two years, having met the COHSASA’s multiple legacy databases, will be able to provide professional quality standards clients with quick and easy access to a treasure trove of of COHSASA. information about their hospitals. A total of 47 members of Want to know how your hospital shapes up with regard to the Association entered the infection control? Get your access code, connect on-line and accreditation programme. the COHSASA information system will tell you exactly how Grahamstown Hospice you stand against professional standards, how various was the first to be departments associated with infection control are managing, accredited, followed by what criteria they are meeting and urgent deficiencies that nine others, which have met must be promptly addressed. stringent requirements for Moreover, if you are in the COHSASA Facilitated REWARDING QUALITY: Chairman of COHSASA, the provision of palliative care. Accreditation Programme, you can monitor staff progress and Albert Ramukumba, hands over the accreditation award to the Nursing Services Director of St Francis They were rated on standards pinpoint the bottlenecks and delays. -

COVID-19 Sentinel Hospital Surveillance Weekly Update on Hospitalized Hcws
COVID-19 Sentinel Hospital Surveillance Weekly Update on Hospitalized HCWs Update: Week 36, 2020 Compiled by: Epidemiology and Surveillance Division National Institute for Occupational Health 25 Hospital Street, Constitution Hill, Johannesburg This report summarises data of COVID-19 cases admitted to sentinel hospital surveillance sites in all 1 provinces. The report is based on data collected from 5 March to 5 September 2020 on the DATCOV platform. HIGHLIGHTS As of 5 September 2020, 2 686 (4.2%) of the 64 705 COVID-19 hospital admissions recorded on the DATCOV surveillance database, were health care workers (HCWs), reported from 247 facilities (81 public-sector and 166 private-sector) in all nine provinces of South Africa. Among 801/2686 (29.8%) HCWs with available data on type of work, 391/801 (48.8%) were nurses, 168/801 (21.0%) were categorized as other HCWs, 111/801 (13.9%) porters or administrators, 57/801 (7.1%) allied HCWs, 52/801 (6.5%) doctors, 15/801 (1.9%) paramedics, and 7/801 (0.9%) laboratory scientists. There was an increase of 157 new HCW admissions since week 35. There were 360 (13.4%) and 2326 (86.6%) admissions reported in the public and private sector, respectively. The majority of HCW admissions were reported in Gauteng (834, 31.1%), KwaZulu-Natal (656, 24.4%), Eastern Cape (465, 17.3%) and Western Cape (281, 10.5%). The median age of COVID-19 HCW admissions was 49 years, there were 482 (17.9%) admissions in HCWs aged 60 years and older. A total of 1912 (71.2%) were female. -

2016 Province District List of Facilities Number of Posts 1. Eastern
Available funded posts for Pharmacist Community Service -2016 Number Province District List of facilities of posts 1. Eastern Cape Amathole Adelaide Hospital (1) Komga Hospital (1) Stutterheim Hospital (1) Bedford Hospital (1) Madwaleni Hospital (1) Tafalofefe Hospital (1) Butterworth Hospital (1) Nompumelelo Hospital (1) Tower TB Hospital (1) Carthcart Hospital (1) Nqamakhwe CHC (1) Victoria Hospital (1) 14 Fort Beaufort Hospital (1) SS Gida Hospital (1) Alfred Nzo Maluti CHC (1) Mount Ayliff Hospital (1) Taylor Bequest Hospital (1) 03 Buffalo City Bhisho (1) Empilweni Gompo Day Grey Hospital (1) Dimbaza CHC (1) Hospital (1) Nkqubela TB Hospital (1) Duncan Village Day Fort Grey (1) 07 Hospital (1) Cacadu Andries Vosloo (1) Midlands Hospital (1) Settlers CHC (1) Fort England Hospital (1) Port Alfred Hospital (1) Temba TB Hospital (1) Humansdorp Hospital (1) PZ Meyer TB Hospital (1) Wilhelm Stahl Hospital (1) 12 Margery Parkes (1) Settlers Hospital (1) Willowmore Hospital (1) Chris Hani All Saints Hospital (1) Dordrecht Hospital (1) Indwe Hospital (1) Cala Hospital (1) Elliot Hospital (1) Komani Hospital (1) Cofimvaba Hospital (1) Frontier Hospital (1) Maclear Hospital (1) 12 Cradock Hospital (1) Clen Grey Hospital (1) Moltena Hospital (1) Joe Gqabi Aliwal North Hospital (1) Empilisweni Hospital (1) Tayler Bequest Hospital (1) Burgersdorp Hospital (1) Lady Grey Hospital (1) Umlamli Hospital (1) 07 Cloete Jourbet Hospital (1) Nelson Mandela PE Pharmaceutical Depot (1) Kwa Zwakhele CHC (1) Orsmond TB Hospital (1) Metro Empilweni Hospital -

Prof Lungile Pepeta (16 July 1974 - 7 August 2020)
IN MEMORIAM Prof Lungile Pepeta (16 July 1974 - 7 August 2020) Professor Lungile Pepeta was born and bred in Ludeke, a village just outside Bizana, Eastern Cape, South Africa, where he grew up attending to cattle like all young men in the villages. He received his primary and secondary education in Bizana and matriculated from Bizana Village High School in 1991. Lungile was drawn into the field of Medicine immediately after matricu- lating. He joined the Faculty of Health Sciences at the University of Transkei (now Walter Sisulu University) in 1992 as a medical student, graduating at the top of his class with his MBChB degree in 1997. After qualifying as a medical doctor, he went on to do his internship at the Mthatha General Hospital (now Nelson Mandela Academic Hospital) in 1998. The internship was followed by community service as a medical officer undertaken at the Frontier Hospital in Queenstown and Dordrecht Hospital in 1999. It was then that he developed a passion for paediatrics and went on to complete a Diploma in Child Health Examination with the Colleges of Medicine of South Africa in October 1999. After community service, Lungile took up a position as a Medical Officer in Paediatrics at King Edward VIII Hospital in January 2000. In July 2000, he joined the Registrar Training Programme in Paediatrics at the University of KwaZulu-Natal (UKZN). He was admitted as a Fellow of Paediatricians by the College of Paediatrics, obtaining an FC Paed (SA) certificate after passing his exit written and oral exami- nations in 2003. After qualifying as a paediatrician, he moved back to the Eastern Cape to take the position as Head of Paediatrics Department at Frontier Hospital in July 2004. -
Inside Cape Town
While COHSASA’s 10 years have been marked by triumphs and setbacks, it’s moments like these when Wentworth Hospital in Durban celebrated its THE COUNCIL accreditation at the start of the new millennium FOR HEALTH that linger forever… SERVICE ACCREDITATION OF SOUTHERN We’ve come a long way AFRICA COHSASA HAS been working in demonstrated the value of this local recognition that COHSASA meets the field of quality improvement in approach in improving the delivery of agreed international standards South African healthcare facilities quality health care to all our citizens. specifically developed and tested for over 10 years. Part of the for healthcare external evaluation In the past ten years of operation, Proudly South African movement, bodies. with COHSASA’s work in 595 COHSASA has achieved global In August 2004 COHSASA facilities in both the public and recognition and is one of only a became the first organisation in private sector, the following handful of internationally accredited the world to undertake the milestones have been reached: accrediting bodies recognised by development of standards for the the International Society for Quality In 1994, the Pilot Accreditation evaluation and management of HIV in Health Care (ISQua). Programme for South African and AIDS within a district and Health Services was launched as a across the continuum of care – from Since its inception, COHSASA has research and development prevention and VCT to terminal care. focused on providing South African programme in the Faculty of (Continued on page 2) solutions for South African problems. Medicine at the University of This has resulted in the development Stellenbosch under the of facilitated accreditation directorship of Dr Stuart programmes for South African Whittaker. -

Health Professions Act (56/1974): List of Approved Facilities for the Purposes of Performing Community Service by Physiotherapists in the Year 2016 39070
STAATSKOERANT, 6 AUGUSTUS 2015 No. 39070 31 DEPARTMENT OF HEALTH NO. 684 06 AUGUST 2015 684 Health Professions Act (56/1974): List Of Approved Facilities For The Purposes Of Performing Community Service By Physiotherapists In The Year 2016 39070 HEALTH PROFESSIONS ACT, 1974 (ACT NO. 56 OF 1974) LIST OF APPROVED FACILITIES FOR THE PURPOSES OF PERFORMING COMMUNITY SERVICE BY PHYSIOTHERAPISTS IN THE YEAR 2016 The Minister of Health has, in terms of regulation 5.1 of the Regulations relating to Performance of Community Service by Persons Registering in terms of the Health Professions Act, 1974 (Act No. 56 of 1974), listed the following approved facilities for purposes of the profession of physiotherapy PROVINCE REGION /DISTRICT FACILITY EASTERN Amatole Mbhashe Sub -District CAPE o Idut a CHH * Madwaleni Hospital * e Tafalofefe Hospital Mnquma Sub -District Butterworth Hospital e Ngqamakhwe CHH Nkonkobe Sub -District e Adelaide FPAH * Bedford CHH Fort Beaufort CHH * Tower Psychiatric Hospital Victoria Hospital * This gazette is also available free online at www.gpwonline.co.za 32 No. 39070 GOVERNMENT GAZETTE, 6 AUGUST 2015 Alfred Nzo Green Ville CHH Madzikane ka Zulu Hospital Mt AyI iff CHH * St Patricks Hospital * Taylor Bequest Hospital (Matatiele) * Buffalo City Metro Bisho Hospital * Cathcart CHH * ® Cecilia Makiwane Hospital ® Empilweni Gompo CHC Frere Hospital Fort Grey TB Hospital Grey Hospital Komgha FPAH Nompumelelo Hospital S.S.Gida CHH * Stuttherheim CHH * Cacadu Camdeboo Sub -District Andries Vosloo Hospital ® Abardeen FPAH Midlands Hospital * Sawas FPAH Kouga Sub -District BJ Forster FPAH Humansdorp Hospital * e Joubertina CHC * Makana Sub -District s Fort England Psychaitric Hospital * e Majorie Parish TB Hospital * o Port Alfred Hospital * This gazette is also available free online at www.gpwonline.co.za STAATSKOERANT, 6 AUGUSTUS 2015 No. -

Sentinel Hospital Surveillance Week 34
COVID-19 SENTINEL HOSPITAL SURVEILLANCE UPDATE SOUTH AFRICA WEEK 34 2020 OVERVIEW This report summarises data of COVID-19 cases admitted to sentinel hospital surveillance sites in all provinces. The report is based on data collected from 5 March to 22 August 2020. HIGHLIGHTS discharged), the case fatality ratio (CFR) ∙ As of 22 August, 58 594 COVID-19 admissions was 19%. On multivariable analysis, factors were reported from 414 facilities (173 public- associated with in-hospital mortality were sector and 241 private-sector) in all nine older age groups; male sex; Black African, provinces of South Africa. There was an Coloured and Indian race; admission in increase of 9 466 admissions reported since the public sector; and having comorbid the last report, and 34 additional hospitals (29 hypertension, diabetes, chronic cardiac public-sector and 5 private-sector) reporting disease, chronic renal disease, malignancy, COVID-19 admissions. There were 19 247 HIV, current tuberculosis alone or both (33%) and 39 347 (67%) admissions reported current and past tuberculosis, and obesity. in public and private sector respectively. Compared to the Western Cape province, The majority of COVID-19 admissions were individuals hospitalised in Eastern Cape, reported from four provinces, 16 983 (29%) Free State, Gauteng, Limpopo and North in Western Cape, 16 090 (28%) in Gauteng, West provinces were more likely to die in- 9 347 (16%) in KwaZulu-Natal and 6 937 hospital. (12%) in Eastern Cape. Admissions in the Western Cape, Eastern Cape and Gauteng have decreased and there are indications of slowing of the rate of increase in admissions in the other provinces over the past three weeks.