Mechanistic Insights from Down Syndrome Europe PMC Funders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Utility of Genetic Risk Scores in Predicting the Onset of Stroke March 2021 6
DOT/FAA/AM-21/24 Office of Aerospace Medicine Washington, DC 20591 The Utility of Genetic Risk Scores in Predicting the Onset of Stroke Diana Judith Monroy Rios, M.D1 and Scott J. Nicholson, Ph.D.2 1. KR 30 # 45-03 University Campus, Building 471, 5th Floor, Office 510 Bogotá D.C. Colombia 2. FAA Civil Aerospace Medical Institute, 6500 S. MacArthur Blvd Rm. 354, Oklahoma City, OK 73125 March 2021 NOTICE This document is disseminated under the sponsorship of the U.S. Department of Transportation in the interest of information exchange. The United States Government assumes no liability for the contents thereof. _________________ This publication and all Office of Aerospace Medicine technical reports are available in full-text from the Civil Aerospace Medical Institute’s publications Web site: (www.faa.gov/go/oamtechreports) Technical Report Documentation Page 1. Report No. 2. Government Accession No. 3. Recipient's Catalog No. DOT/FAA/AM-21/24 4. Title and Subtitle 5. Report Date March 2021 The Utility of Genetic Risk Scores in Predicting the Onset of Stroke 6. Performing Organization Code 7. Author(s) 8. Performing Organization Report No. Diana Judith Monroy Rios M.D1, and Scott J. Nicholson, Ph.D.2 9. Performing Organization Name and Address 10. Work Unit No. (TRAIS) 1 KR 30 # 45-03 University Campus, Building 471, 5th Floor, Office 510, Bogotá D.C. Colombia 11. Contract or Grant No. 2 FAA Civil Aerospace Medical Institute, 6500 S. MacArthur Blvd Rm. 354, Oklahoma City, OK 73125 12. Sponsoring Agency name and Address 13. Type of Report and Period Covered Office of Aerospace Medicine Federal Aviation Administration 800 Independence Ave., S.W. -
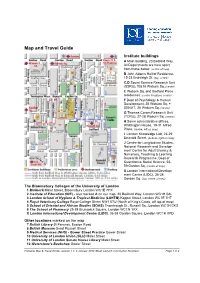
Map and Travel Guide
Map and Travel Guide Institute buildings A Main building, 20 Bedford Way. All Departments are here apart from those below. (centre of map) B John Adams Hall of Residence, 15-23 Endsleigh St. (top, centre) C,D Social Science Research Unit (SSRU),10&18 Woburn Sq. (centre) E Woburn Sq. and Bedford Place residences. (centre & bottom, centre) F Dept of Psychology & Human Development, 25 Woburn Sq. + SENJIT, 26 Woburn Sq. (centre) G Thomas Coram Research Unit (TCRU), 27-28 Woburn Sq. (centre) H Some administrative offices, Whittington House, 19-31 Alfred Place. (centre, left on map) I London Knowledge Lab, 23-29 Emerald Street. (bottom, right on map) J Centre for Longitudinal Studies, National Research and Develop- ment Centre for Adult Literacy & Numeracy, Teaching & Learning Research Programme, Dept of Quantitative Social Science, 55- 59 Gordon Sq. (centre of map) X London International Develop- ment Centre (LIDC), 36-38 (top, centre of map) Gordon Sq. The Bloomsbury Colleges of the University of London 1 Birkbeck Malet Street, Bloomsbury London WC1E 7HX 2 Institute of Education (IOE) - also marked A on our map, 20 Bedford Way, London WC1H 0AL 3 London School of Hygiene & Tropical Medicine (LSHTM) Keppel Street, London WC1E 7HT 4 Royal Veterinary College Royal College Street NW1 0TU (North of King's Cross, off top of map) 5 School of Oriental and African Studies (SOAS) Thornhaugh St., Russell Sq., London WC1H 0XG 6 The School of Pharmacy 29-39 Brunswick Square, London WC1N 1AX X London International Development Centre (LIDC), 36-38 Gordon -

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

Noelia Díaz Blanco
Effects of environmental factors on the gonadal transcriptome of European sea bass (Dicentrarchus labrax), juvenile growth and sex ratios Noelia Díaz Blanco Ph.D. thesis 2014 Submitted in partial fulfillment of the requirements for the Ph.D. degree from the Universitat Pompeu Fabra (UPF). This work has been carried out at the Group of Biology of Reproduction (GBR), at the Department of Renewable Marine Resources of the Institute of Marine Sciences (ICM-CSIC). Thesis supervisor: Dr. Francesc Piferrer Professor d’Investigació Institut de Ciències del Mar (ICM-CSIC) i ii A mis padres A Xavi iii iv Acknowledgements This thesis has been made possible by the support of many people who in one way or another, many times unknowingly, gave me the strength to overcome this "long and winding road". First of all, I would like to thank my supervisor, Dr. Francesc Piferrer, for his patience, guidance and wise advice throughout all this Ph.D. experience. But above all, for the trust he placed on me almost seven years ago when he offered me the opportunity to be part of his team. Thanks also for teaching me how to question always everything, for sharing with me your enthusiasm for science and for giving me the opportunity of learning from you by participating in many projects, collaborations and scientific meetings. I am also thankful to my colleagues (former and present Group of Biology of Reproduction members) for your support and encouragement throughout this journey. To the “exGBRs”, thanks for helping me with my first steps into this world. Working as an undergrad with you Dr. -

The Complex SNP and CNV Genetic Architecture of the Increased Risk of Congenital Heart Defects in Down Syndrome
Downloaded from genome.cshlp.org on September 24, 2021 - Published by Cold Spring Harbor Laboratory Press Research The complex SNP and CNV genetic architecture of the increased risk of congenital heart defects in Down syndrome M. Reza Sailani,1,2 Periklis Makrythanasis,1 Armand Valsesia,3,4,5 Federico A. Santoni,1 Samuel Deutsch,1 Konstantin Popadin,1 Christelle Borel,1 Eugenia Migliavacca,1 Andrew J. Sharp,1,20 Genevieve Duriaux Sail,1 Emilie Falconnet,1 Kelly Rabionet,6,7,8 Clara Serra-Juhe´,7,9 Stefano Vicari,10 Daniela Laux,11 Yann Grattau,12 Guy Dembour,13 Andre Megarbane,12,14 Renaud Touraine,15 Samantha Stora,12 Sofia Kitsiou,16 Helena Fryssira,16 Chariklia Chatzisevastou-Loukidou,16 Emmanouel Kanavakis,16 Giuseppe Merla,17 Damien Bonnet,11 Luis A. Pe´rez-Jurado,7,9 Xavier Estivill,6,7,8 Jean M. Delabar,18 and Stylianos E. Antonarakis1,2,19,21 1–19[Author affiliations appear at the end of the paper.] Congenital heart defect (CHD) occurs in 40% of Down syndrome (DS) cases. While carrying three copies of chromosome 21 increases the risk for CHD, trisomy 21 itself is not sufficient to cause CHD. Thus, additional genetic variation and/or environmental factors could contribute to the CHD risk. Here we report genomic variations that in concert with trisomy 21, determine the risk for CHD in DS. This case-control GWAS includes 187 DS with CHD (AVSD = 69, ASD = 53, VSD = 65) as cases, and 151 DS without CHD as controls. Chromosome 21–specific association studies revealed rs2832616 and rs1943950 as CHD risk alleles (adjusted genotypic P-values <0.05). -

Supplementary Data
Supplementary Fig. 1 A B Responder_Xenograft_ Responder_Xenograft_ NON- NON- Lu7336, Vehicle vs Lu7466, Vehicle vs Responder_Xenograft_ Responder_Xenograft_ Sagopilone, Welch- Sagopilone, Welch- Lu7187, Vehicle vs Lu7406, Vehicle vs Test: 638 Test: 600 Sagopilone, Welch- Sagopilone, Welch- Test: 468 Test: 482 Responder_Xenograft_ NON- Lu7860, Vehicle vs Responder_Xenograft_ Sagopilone, Welch - Lu7558, Vehicle vs Test: 605 Sagopilone, Welch- Test: 333 Supplementary Fig. 2 Supplementary Fig. 3 Supplementary Figure S1. Venn diagrams comparing probe sets regulated by Sagopilone treatment (10mg/kg for 24h) between individual models (Welsh Test ellipse p-value<0.001 or 5-fold change). A Sagopilone responder models, B Sagopilone non-responder models. Supplementary Figure S2. Pathway analysis of genes regulated by Sagopilone treatment in responder xenograft models 24h after Sagopilone treatment by GeneGo Metacore; the most significant pathway map representing cell cycle/spindle assembly and chromosome separation is shown, genes upregulated by Sagopilone treatment are marked with red thermometers. Supplementary Figure S3. GeneGo Metacore pathway analysis of genes differentially expressed between Sagopilone Responder and Non-Responder models displaying –log(p-Values) of most significant pathway maps. Supplementary Tables Supplementary Table 1. Response and activity in 22 non-small-cell lung cancer (NSCLC) xenograft models after treatment with Sagopilone and other cytotoxic agents commonly used in the management of NSCLC Tumor Model Response type -

N6AMT1 / HEMK2 (1-214, His-Tag) Human Protein – AR51691PU-N
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for AR51691PU-N N6AMT1 / HEMK2 (1-214, His-tag) Human Protein Product data: Product Type: Recombinant Proteins Description: N6AMT1 / HEMK2 (1-214, His-tag) human recombinant protein, 0.1 mg Species: Human Expression Host: E. coli Tag: His-tag Predicted MW: 25.3 kDa Concentration: lot specific Purity: >85% by SDS - PAGE Buffer: Presentation State: Purified Buffer System: Liquid, In Phosphate buffered saline (pH7.4) containing 20% glycerol, 1mM DTT. Protein Description: Recombinant human N6ATM1 protein, fused to His-tag at N-terminus, was expressed in E.coli and purified by using conventional chromatography techniques. Storage: Store undiluted at 2-8°C for one week or (in aliquots) at -20°C to -80°C for longer. Avoid repeated freezing and thawing. Stability: Shelf life: one year from despatch. RefSeq: NP_037372 Locus ID: 29104 UniProt ID: Q9Y5N5 Cytogenetics: 21q21.3 Synonyms: C21orf127; HEMK2; KMT9; m.HsaHemK2P; MTQ2; N6AMT; PRED28; PrmC Summary: This gene encodes an N(6)-adenine-specific DNA methyltransferase. The encoded enzyme may be involved in the methylation of release factor I during translation termination. This enzyme is also involved in converting the arsenic metabolite monomethylarsonous acid to the less toxic dimethylarsonic acid. Alternative splicing pf this gene results in multiple transcript variants. A related pseudogene has been identified on chromosome 11. [provided by RefSeq, Jul 2014] Protein Families: Druggable Genome This product is to be used for laboratory only. -

N6AMT1 Rabbit Pab
Leader in Biomolecular Solutions for Life Science N6AMT1 Rabbit pAb Catalog No.: A7201 Basic Information Background Catalog No. This gene encodes an N(6)-adenine-specific DNA methyltransferase. The encoded A7201 enzyme may be involved in the methylation of release factor I during translation termination. This enzyme is also involved in converting the arsenic metabolite Observed MW monomethylarsonous acid to the less toxic dimethylarsonic acid. Alternative splicing pf 23KDa this gene results in multiple transcript variants. A related pseudogene has been identified on chromosome 11. Calculated MW 19kDa/22kDa Category Primary antibody Applications WB, IHC, IF Cross-Reactivity Human, Mouse, Rat Recommended Dilutions Immunogen Information WB 1:500 - 1:2000 Gene ID Swiss Prot 29104 Q9Y5N5 IHC 1:50 - 1:200 Immunogen 1:50 - 1:100 IF Recombinant fusion protein containing a sequence corresponding to amino acids 1-186 of human N6AMT1 (NP_877426.3). Synonyms N6AMT1;C21orf127;HEMK2;MTQ2;N6AMT;PRED28;m.HsaHemK2P Contact Product Information www.abclonal.com Source Isotype Purification Rabbit IgG Affinity purification Storage Store at -20℃. Avoid freeze / thaw cycles. Buffer: PBS with 0.02% sodium azide,50% glycerol,pH7.3. Validation Data Western blot analysis of extracts of Rat kidney, using N6AMT1 antibody (A7201) at 1:1000 dilution. Secondary antibody: HRP Goat Anti-Rabbit IgG (H+L) (AS014) at 1:10000 dilution. Lysates/proteins: 25ug per lane. Blocking buffer: 3% nonfat dry milk in TBST. Detection: ECL Basic Kit (RM00020). Exposure time: 90s. Immunohistochemistry of paraffin- Immunohistochemistry of paraffin- Immunofluorescence analysis of PC-12 embedded rat brain using N6AMT1 embedded human kidney using N6AMT1 cells using N6AMT1 Rabbit pAb (A7201) at Antibody (A7201) at dilution of 1:100 (40x Antibody (A7201) at dilution of 1:100 (40x dilution of 1:100 (40x lens). -

Methyltransferase (AS3MT) and N-6 Adenine-Specific DNA Methyltransferase 1 (N6AMT1) Polymorphisms, Arsenic Metabolism, and Cancer Risk in a Chilean Population
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Environ Manuscript Author Mol Mutagen. Author Manuscript Author manuscript; available in PMC 2018 July 01. Published in final edited form as: Environ Mol Mutagen. 2017 July ; 58(6): 411–422. doi:10.1002/em.22104. Associations between arsenic (+3 oxidation state) methyltransferase (AS3MT) and N-6 adenine-specific DNA methyltransferase 1 (N6AMT1) polymorphisms, arsenic metabolism, and cancer risk in a Chilean population Rosemarie de la Rosa1, Craig Steinmaus1, Nicholas K Akers1, Lucia Conde1, Catterina Ferreccio2, David Kalman3, Kevin R Zhang1, Christine F Skibola1, Allan H Smith1, Luoping Zhang1, and Martyn T Smith1 1Superfund Research Program, School of Public Health, University of California, Berkeley, CA 2Pontificia Universidad Católica de Chile, Santiago, Chile, Advanced Center for Chronic Diseases, ACCDiS 3School of Public Health, University of Washington, Seattle, WA Abstract Inter-individual differences in arsenic metabolism have been linked to arsenic-related disease risks. Arsenic (+3) methyltransferase (AS3MT) is the primary enzyme involved in arsenic metabolism, and we previously demonstrated in vitro that N-6 adenine-specific DNA methyltransferase 1 (N6AMT1) also methylates the toxic iAs metabolite, monomethylarsonous acid (MMA), to the less toxic dimethylarsonic acid (DMA). Here, we evaluated whether AS3MT and N6AMT1 gene polymorphisms alter arsenic methylation and impact iAs-related cancer risks. We assessed AS3MT and N6AMT1 polymorphisms and urinary arsenic metabolites (%iAs, %MMA, %DMA) in 722 subjects from an arsenic-cancer case-control study in a uniquely exposed area in northern Chile. Polymorphisms were genotyped using a custom designed multiplex, ligation-dependent probe amplification (MLPA) assay for 6 AS3MT SNPs and 14 tag SNPs in the N6AMT1 gene. -

Gene Expression Profiling in Pachyonychia Congenita Skin
15 March 2005 Use of Articles in the Pachyonychia Congenita Bibliography The articles in the PC Bibliography may be restricted by copyright laws. These have been made available to you by PC Project for the exclusive use in teaching, scholar- ship or research regarding Pachyonychia Congenita. To the best of our understanding, in supplying this material to you we have followed the guidelines of Sec 107 regarding fair use of copyright materials. That section reads as follows: Sec. 107. - Limitations on exclusive rights: Fair use Notwithstanding the provisions of sections 106 and 106A, the fair use of a copyrighted work, including such use by reproduction in copies or phonorecords or by any other means specified by that section, for purposes such as criticism, comment, news reporting, teaching (including multiple copies for classroom use), scholarship, or research, is not an infringement of copyright. In determining whether the use made of a work in any particular case is a fair use the factors to be considered shall include - (1) the purpose and character of the use, including whether such use is of a commercial nature or is for nonprofit educational purposes; (2) the nature of the copyrighted work; (3) the amount and substantiality of the portion used in relation to the copyrighted work as a whole; and (4) the effect of the use upon the potential market for or value of the copyrighted work. The fact that a work is unpublished shall not itself bar a finding of fair use if such finding is made upon consideration of all the above factors. -

NRF1) Coordinates Changes in the Transcriptional and Chromatin Landscape Affecting Development and Progression of Invasive Breast Cancer
Florida International University FIU Digital Commons FIU Electronic Theses and Dissertations University Graduate School 11-7-2018 Decipher Mechanisms by which Nuclear Respiratory Factor One (NRF1) Coordinates Changes in the Transcriptional and Chromatin Landscape Affecting Development and Progression of Invasive Breast Cancer Jairo Ramos [email protected] Follow this and additional works at: https://digitalcommons.fiu.edu/etd Part of the Clinical Epidemiology Commons Recommended Citation Ramos, Jairo, "Decipher Mechanisms by which Nuclear Respiratory Factor One (NRF1) Coordinates Changes in the Transcriptional and Chromatin Landscape Affecting Development and Progression of Invasive Breast Cancer" (2018). FIU Electronic Theses and Dissertations. 3872. https://digitalcommons.fiu.edu/etd/3872 This work is brought to you for free and open access by the University Graduate School at FIU Digital Commons. It has been accepted for inclusion in FIU Electronic Theses and Dissertations by an authorized administrator of FIU Digital Commons. For more information, please contact [email protected]. FLORIDA INTERNATIONAL UNIVERSITY Miami, Florida DECIPHER MECHANISMS BY WHICH NUCLEAR RESPIRATORY FACTOR ONE (NRF1) COORDINATES CHANGES IN THE TRANSCRIPTIONAL AND CHROMATIN LANDSCAPE AFFECTING DEVELOPMENT AND PROGRESSION OF INVASIVE BREAST CANCER A dissertation submitted in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY in PUBLIC HEALTH by Jairo Ramos 2018 To: Dean Tomás R. Guilarte Robert Stempel College of Public Health and Social Work This dissertation, Written by Jairo Ramos, and entitled Decipher Mechanisms by Which Nuclear Respiratory Factor One (NRF1) Coordinates Changes in the Transcriptional and Chromatin Landscape Affecting Development and Progression of Invasive Breast Cancer, having been approved in respect to style and intellectual content, is referred to you for judgment. -

Dark Proteome Database: Studies on Dark Proteins
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 21 January 2019 doi:10.20944/preprints201901.0198.v1 Dark Proteome Database: Studies on Dark Proteins Nelson Perdigão 1,2,* 1 Instituto Superior Técnico, Universidade de Lisboa, 1049-001 Lisbon, Portugal 2 Instituto de Sistemas e Robótica, 1049-001 Lisbon, Portugal. * Correspondence: [email protected] Abstract: The dark proteome as we define it, is the part of the proteome where 3D structure has not been observed either by homology modeling or by experimental characterization in the protein universe. From the 550.116 proteins available in Swiss-Prot (as of July 2016) 43.2% of the Eukarya universe and 49.2% of the Virus universe are part of the dark proteome. In Bacteria and Archaea, the percentage of the dark proteome presence is significantly less, with 12.6% and 13.3% respectively. In this work, we present the map of the dark proteome in Human and in other model organisms. The most significant result is that around 40%- 50% of the proteome of these organisms are still in the dark, where the higher percentages belong to higher eukaryotes (mouse and human organisms). Due to the amount of darkness present in the human organism being more than 50%, deeper studies were made, including the identification of ‘dark’ genes that are responsible for the production of the so-called dark proteins, as well as, the identification of the ‘dark’ organs where dark proteins are over represented, namely heart, cervical mucosa and natural killer cells. This is a step forward in the direction of the human dark proteome.