Ovarian Fibroma with Serous Cystadenoma—An Unusual Combination: a Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Histological Tumour Type (Required)
Histological tumour type (Required) Reason/Evidentiary Support All ovarian epithelial malignancies and borderline tumours should be typed according to the WHO classification.1 There are 5 major subtypes of primary ovarian carcinoma, high‐grade serous, clear cell, endometrioid, mucinous and low‐ grade serous.2‐5 There are also other uncommon minor subtypes, those listed by the WHO including malignant Brenner tumour, seromucinous carcinoma and undifferentiated carcinoma.1 Carcinosarcoma is a mixed epithelial and mesenchymal malignancy but is included in the category of epithelial malignancies in this dataset since most are of epithelial origin and histogenesis.6 Although management of ovarian carcinoma is, at present, largely dependent on tumour stage and grade, accurate typing will almost certainly become more important in the future with the introduction of targeted therapies and specific treatments for different tumour types. This is in part because, although clinically often considered as one disease, there is an increasing realisation that the different morphological subtypes of ovarian carcinoma have a different pathogenesis, are associated with distinct molecular alterations and have a different natural history, response to traditional chemotherapy and prognosis.2‐5 Tumour typing may also be important in identifying or initiating testing for an underlying genetic predisposition; for example, high‐grade serous carcinoma may be associated with underlying BRCA1/2 mutation while endometrioid and clear cell carcinomas can occur in patients with Lynch syndrome.7 The most common ovarian carcinoma is high‐grade serous carcinoma (approximately 70%) followed by clear cell and endometrioid.8,9 Mucinous and low‐grade serous are less common. Approximately 90% of advanced stage ovarian carcinomas (stage III/IV) are high‐grade serous in type.8,9 Most primary tubal carcinomas are high‐grade serous or endometrioid and most primary peritoneal carcinomas are of high‐grade serous type. -

BSOG-FOGSI Quiz Preliminary Round Conducted on 24Th April at API
BSOG-FOGSI quiz preliminary round conducted on 24th April at API Bhavana South Zone Yuva Fogsi 2016 Quiz – BSOG round Topic- Gynecological Oncology 24th April, 2016 (60 marks) Name: Institution: Dear participants, Welcome to the FOGSI Quiz 2016 Thirty questions are to be answered in 30 minutes. Circle the right answer. Scratching and overwriting will get a negative marking even if the final answer is right. Each correct answer gets 2 marks and a wrong one gets a negative marking of minus 1.The top 2 scorers will represent BSOG in South Zone Yuva FOGSI 2016 in Madurai on 22nd May 2016. The decision of the Quiz Master is final. Happy Quizzing!!! 1. With regards to the staging of endometrial cancer, pick the wrong answer a. Stage 1a Endometrial Adenocarcinoma is confined to the uterus and involves less than half of the myometrium b. Stage 4a Endometrial Adenocarcinoma invades bladder mucosa c. Stage 4b Endometrial Adenocarcinoma involves inguinal lymph nodes d. Stage 3c2 Endometrial Adenocarcinoma involves more than half of myometrium and pelvic lymph nodes Ans: Stage 3c1 is involvement of pelvic nodes, Stage 3c2 is involvement of paraaortic nodes 2. The average time between HPV infection and pre-cancer is a. 2-5 years b. 15-20 years c. 7-10 years d. 20-25 years Novak 3. What factor does not contribute to persistence and progression of HPV infection? a. Smoking b. Contraceptive use c. STDs d. Drinking alcohol Novak 4. On Colposcopy, Adenocarcinoma has the following features a. Mosaic pattern b. Punctate lesions c. Abnormal vasculature d. -

Case Reports 95
r- CASE REPORTS 95 CASE REPORTS Past & family history were not contributory. General physical examination revealed no abnor mality. On abdominal examination- abdomen was overdistended, presenting part could not be made out, however there was suspicion of breech ABilA SINGH • NEERJA SETIII presentation. Fetal heart was not localised, mod erate uterine contractions were present. On per NEERA AGARWAL • K MISRA vaginum examination- cervix was fully effaced and 5 em dilated, soft irregular presenting part INTRODUCTION was felt high up at brim and liquor was blood 1 / Sacroccocygeal teratoma is a potentially stained. 2 2 hours later the patient delivered a 28 malignant congenital tumour. The incidence re weeks size still born female fetus weighing 850 ported in India is 1 in 30,000-40,000 live births. grns by breech. There was no PPH. Placenta These tumours present either as obstructed labour or dystocia. The case is reported because of its rare occurence. CASE REPORT Mrs. K. 22 year old unhooked, primigravida was admitted to G.T.B. Hospital with 7 months amenorrhoea and labour pains for 3 hours. Her antenatal period was uneventfull with no history of drug intake. Menstrual Cycles were regular. 'Dtpt. of 06Jt<t antf qynu, antf 'Patfw. ~cctp tttf for 'Pu6lication on 2216/ 91 fig. 1 96 JOURNAL OF OBSTETRICS AND GYNAECOLOGY weighed 120 gm. There was no gmss abnormal AIIMS as she was Rb -ve. She bad a diagnostic ity detected in the placenta. laparoscopy one year back at a private hospital Examination of the fetus showed a bilobed where a bicornuate uterus was diagnosed and massofl5x 17 cmarisingfromtbesacrococcygeal excision of complete longitudinal vaginal sep region with partial rupture of one lobe, cut tum was done. -

SNOMED CT Codes for Gynaecological Neoplasms
SNOMED CT codes for gynaecological neoplasms Authors: Brian Rous1 and Naveena Singh2 1Cambridge University Hospitals NHS Trust and 2Barts Health NHS Trusts Background (summarised from NHS Digital): • SNOMED CT is a structured clinical vocabulary for use in an electronic health record. It forms an integral part of the electronic care record, and serves to represent care information in a clear, consistent, and comprehensive manner. • The move to a single terminology, SNOMED CT, for the direct management of care of an individual, across all care settings in England, is recommended by the National Information Board (NIB), in “Personalised Health and Care 2020: A Framework for Action”. • SNOMED CT is owned, managed and licensed by SNOMED International. NHS Digital is the UK Member's National Release Centre for the creation of, and delegated authority to licence the SNOMED CT Edition and derivatives. • The benefits of using SNOMED CT in electronic care records are that it: • enables sharing of vital information consistently within and across health and care settings • allows comprehensive coverage and greater depth of details and content for all clinical specialities and professionals • includes diagnosis and procedures, symptoms, family history, allergies, assessment tools, observations, devices • supports clinical decision making • facilitates analysis to support clinical audit and research • reduces risk of misinterpretations of the record in different care settings • Implementation plans for England: • SNOMED CT must be implemented across primary care and deployed to GP practices in a phased approach from April 2018. • Secondary care, acute care, mental health, community systems, dentistry and other systems used in direct patient care must use SNOMED CT as the clinical terminology, before 1 April 2020. -

Brenner Tumor with Serous Cystadenoma- an Unusual Combination: a Case Report
DOI: 10.5958/2319-5886.2015.00045.4 International Journal of Medical Research & Health Sciences www.ijmrhs.com Volume 4 Issue 1 Coden: IJMRHS Copyright @2014 ISSN: 2319-5886 Received: 6th Nov 2014 Revised: 28th Nov 2014 Accepted: 31st Dec 2014 Case report BRENNER TUMOR WITH SEROUS CYSTADENOMA- AN UNUSUAL COMBINATION: A CASE REPORT *Syam Sundar B1, Shanthi V1, Mohan Rao N1, Bhavana Grandhi2, Chidananda Reddy V 2, Swathi S2 1Associate Professor, 2Assistant professor, Department of Pathology, Narayana Medical College, Nellore, A.P, India *Corresponding author email: syam.byna&gmail.com ABSTRACT Surface epithelial tumors are most common, which comprise 58% of all ovarian tumors. Serous and mucinous cystadenoma are the most common epithelial tumors which accounts for about 35% of ovarian tumors. Different combinations of epithelial tumors can occur in ovary most common among them is Mucinous cystadenoma and Brenner tumor. We report a case of an ovarian tumor with rare combination Brenner tumor with serous cyst adenoma of ovary in 56 year old female patient. Only a few cases with this combination are very rarely reported in the literature. Keywords: Brenner Tumor, Serous cystadenoma. INTRODUCTION Surface epithelial tumors are the most important CASE REPORT group of neoplasm of ovary which are namely serous, mucinous, endometroid, clear cell and Brenner along A 56 year old female patient presented with a with combinations of these types1. Surface epithelial swelling in the lower abdomen with intermittent tumors occur at all ages with a peak incidence in 2nd abdominal pain over a period of 1 year. Clinically, to 5th decade of life. -
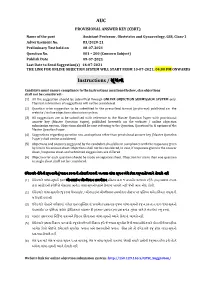
AUC Instructions / ૂચના
AUC PROVISIONAL ANSWER KEY (CBRT) Name of the post Assistant Professor, Obstetrics and Gynaecology, GSS, Class-1 Advertisement No. 83/2020-21 Preliminary Test held on 08-07-2021 Question No. 001 – 200 (Concern Subject) Publish Date 09-07-2021 Last Date to Send Suggestion(s) 16-07-2021 THE LINK FOR ONLINE OBJECTION SYSTEM WILL START FROM 10-07-2021; 04:00 PM ONWARDS Instructions / ૂચના Candidate must ensure compliance to the instructions mentioned below, else objections shall not be considered: - (1) All the suggestion should be submitted through ONLINE OBJECTION SUBMISSION SYSTEM only. Physical submission of suggestions will not be considered. (2) Question wise suggestion to be submitted in the prescribed format (proforma) published on the website / online objection submission system. (3) All suggestions are to be submitted with reference to the Master Question Paper with provisional answer key (Master Question Paper), published herewith on the website / online objection submission system. Objections should be sent referring to the Question, Question No. & options of the Master Question Paper. (4) Suggestions regarding question nos. and options other than provisional answer key (Master Question Paper) shall not be considered. (5) Objections and answers suggested by the candidate should be in compliance with the responses given by him in his answer sheet. Objections shall not be considered, in case, if responses given in the answer sheet /response sheet and submitted suggestions are differed. (6) Objection for each question should be made on separate sheet. Objection for more than one question in single sheet shall not be considered. ઉમેદવાર નીચેની ૂચનાઓું પાલન કરવાની તકદાર રાખવી, અયથા વાંધા- ૂચન ગે કરલ રૂઆતો યાને લેવાશે નહ (1) ઉમેદવાર વાંધાં- ૂચનો ફત ઓનલાઈન ઓશન સબમીશન સીટમ ારા જ સબમીટ કરવાના રહશે. -

Rotana Alsaggaf, MS
Neoplasms and Factors Associated with Their Development in Patients Diagnosed with Myotonic Dystrophy Type I Item Type dissertation Authors Alsaggaf, Rotana Publication Date 2018 Abstract Background. Recent epidemiological studies have provided evidence that myotonic dystrophy type I (DM1) patients are at excess risk of cancer, but inconsistencies in reported cancer sites exist. The risk of benign tumors and contributing factors to tu... Keywords Cancer; Tumors; Cataract; Comorbidity; Diabetes Mellitus; Myotonic Dystrophy; Neoplasms; Thyroid Diseases Download date 07/10/2021 07:06:48 Link to Item http://hdl.handle.net/10713/7926 Rotana Alsaggaf, M.S. Pre-doctoral Fellow - Clinical Genetics Branch, Division of Cancer Epidemiology & Genetics, National Cancer Institute, NIH PhD Candidate – Department of Epidemiology & Public Health, University of Maryland, Baltimore Contact Information Business Address 9609 Medical Center Drive, 6E530 Rockville, MD 20850 Business Phone 240-276-6402 Emails [email protected] [email protected] Education University of Maryland – Baltimore, Baltimore, MD Ongoing Ph.D. Epidemiology Expected graduation: May 2018 2015 M.S. Epidemiology & Preventive Medicine Concentration: Human Genetics 2014 GradCert. Research Ethics Colorado State University, Fort Collins, CO 2009 B.S. Biological Science Minor: Biomedical Sciences 2009 Cert. Biomedical Engineering Interdisciplinary studies program Professional Experience Research Experience 2016 – present Pre-doctoral Fellow National Cancer Institute, National Institutes -

Statistical Analysis Plan
Cover Page for Statistical Analysis Plan Sponsor name: Novo Nordisk A/S NCT number NCT03061214 Sponsor trial ID: NN9535-4114 Official title of study: SUSTAINTM CHINA - Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Document date: 22 August 2019 Semaglutide s.c (Ozempic®) Date: 22 August 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL Clinical Trial Report Status: Final Appendix 16.1.9 16.1.9 Documentation of statistical methods List of contents Statistical analysis plan...................................................................................................................... /LQN Statistical documentation................................................................................................................... /LQN Redacted VWDWLVWLFDODQDO\VLVSODQ Includes redaction of personal identifiable information only. Statistical Analysis Plan Date: 28 May 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL UTN:U1111-1149-0432 Status: Final EudraCT No.:NA Page: 1 of 30 Statistical Analysis Plan Trial ID: NN9535-4114 Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Author Biostatistics Semaglutide s.c. This confidential document is the property of Novo Nordisk. No unpublished information contained herein may be disclosed without prior written approval from Novo Nordisk. Access to this document must be restricted to relevant parties.This -

Fertility-Sparing Management and Obstetric Outcomes in a 20-Year-Old Patient with a Sertoli-Leydig Cell Tumor of the Ovary: a Case Report and Review of the Literature
ONCOLOGY LETTERS 12: 1079-1082, 2016 Fertility-sparing management and obstetric outcomes in a 20-year-old patient with a Sertoli-Leydig cell tumor of the ovary: A case report and review of the literature THOMAS STAVRAKIS1, IOANNIS KALOGIANNIDIS1, STAMATIOS PETOUSIS1, CHRISOULA TSOMPANIDOU2, DIMITRIS DELKOS1, NIKOLAOS PRAPAS1 and DAVID ROUSSO1 1Third Department of Obstetrics and Gynecology, Aristotle University of Thessaloniki, 54642 Thessaloniki; 2Department of Pathology, ‘Agios Dimitrios’ General Hospital, 54634 Thessaloniki, Greece Received November 24, 2014; Accepted November 26, 2015 DOI: 10.3892/ol.2016.4695 Abstract. Sertoli-Leydig cell tumors (SLCTs) are an located in one ovary (1,2). SLCTs may produce androgens or uncommon subtype of sex-cord stromal tumors of the ovary, estrogens, and their prognosis is associated with tumor differ- which most commonly arise in women of reproductive age, entiation and disease stage (1). creating an issue with regard to the preservation of fertility. SLCTs are most commonly diagnosed in young women, The clinical manifestation of SLCTs varies widely, ranging creating an issue with regard to the preservation of fertility (3). from an asymptomatic clinical profile to extreme viriliza- Oncologists should consider the risk of infertility in women of tion. Correct diagnosis of SLCT is crucial and is primarily reproductive age who undergo treatment for SLCTs. Patients based on histopathological results. The current study presents must be thoroughly informed about the conservative treatment the case of a 20-year-old woman who underwent unilateral alternatives for genital tract preservation, as well as the poten- salpingo-oophorectomy and adjuvant chemotherapy due to the tial risk of recurrent disease. -

Ovarian Fibrothecoma - a Diagnostic Dilemma
Obstetrics & Gynecology International Journal Case Report Open Access Ovarian fibrothecoma - a diagnostic dilemma Abstract Volume 10 Issue 3 - 2019 Background: The presentation of ovarian fibrothecoma is highly deceptive and it may Nikita Kumari,1 Bindu Bajaj2 be undiagnosed till histopathology reveals the actual diagnosis. Hence, the clinician 1 must be aware of such cases which may present as a diagnostic dilemma. Attending Consultant at Sitaram Bhartia Institute of Science and Research, Ex Senior Resident at VMMC and Safdarjung Introduction: Ovarian fibrothecomas are rare ovarian neoplasm. We report a case Hospital, India where clinical presentation was highly deceptive and suggestive of malignant tumor. 2Associate Professor at VMMC and Safdarjung Hospital, New However, ascitic fluid cytology revealed absent malignant cells. On histopathological Delhi, India examination, it was diagnosed as benign fibrothecoma with cystic changes. Postoperative follow-up for about six months was uneventful. Correspondence: Nikita Kumari, Attending Consultant at Sitaram Bhartia Institute of Science and Research, Ex Senior Case: A 45 year old female presented with large abdominal lump of 20 weeks size Resident at VMMC and Safdarjung Hospital, New Delhi, India, Tel associated with pain abdomen. She was admitted for management and evaluation. 9654251653, Email Hematological and biochemical parameters were normal. USG revealed a large multilocular, predominantly cystic lesion 20.9x9.6x11.4 cm in pelvis. CECT revealed Received: May 27, 2019 | Published: June 13, 2019 ovarian cystadenocarcinoma left ovary with locoregional mass effect, mild ascites and suspicious metastasis to internal iliac lymph nodes. Hence panhysterectomy and omentectomy was performed as radiological and preoperative clinical diagnosis was malignant ovarian tumor. On gross examination, a well encapsulated, multinodular cystic tumor of left ovary about 17x14x7 cm was identified. -

Leydig Cell Tumour
Non-germ cell tumours of the testis Testis: non-germ cell tumours . Sex cord-stromal tumours Dr Jonathan H Shanks . Haemolymphoid neoplasms . Other neoplasms The Christie NHS . Tumour-like conditions Foundation Trust, Manchester, UK . Metastases The Christie NHS Foundation Trust The Christie NHS Foundation Trust Testis: sex cord-stromal tumours . Leydig cell tumour . Sertoli cell tumour, NOS . Sclerosing Sertoli cell tumour . Large cell calcifying Sertoli cell tumour . Granulosa cell tumour, adult-type . Juvenile granulosa cell tumour . Fibroma . Brenner tumour . Sertoli-Leydig cell tumours (exceptionally rare in testis) Leydig cell tumour . Sex cord-stromal tumour, unclassified . Mixed germ cell-sex cord stromal tumour - gonadoblastoma - unclassified (some may be sex cord stromal tumours with entrapped germ cells – see Ulbright et al., 2000) - collision tumour The Christie NHS Foundation Trust The Christie NHS Foundation Trust Differential diagnosis of Leydig cell TTAGS tumour . Testicular tumour of adrenogenital syndrome (TTAGS) . Multifocal/bilateral lesions (especially in a child/young adult) . Seen in patients with congenital adrenal hyperplasia . Leydig cell hyperplasia (<5mm) . 21 hydroxylase deficience most common . Large cell calcifying Sertoli cell tumour . Elevated serum ACTH . Sertoli cell tumour . Seminoma (rare cases with cytoplasmic clearing) . Benign lesion treated with steroids; partial orchidectomy reserved for steroid unresponsive cases . Mixed sex cord stromal tumours . Sex cord stromal tumour unclassified . Fibrous bands; lipofuscin pigment ++; nuclear pleomorphism but no mitosis . Metastasis e.g. melanoma The Christie NHS Foundation Trust The Christie NHS Foundation Trust Immunohistochemistry of testicular Histopathological and immunophenotypic features of testicular tumour of adrenogenital Leydig cell tumour syndrome Wang Z et al. Histopathology 2011;58:1013-18 McCluggage et al Amin, Young, Scully . -

Brenner Tumor of Ovary: an Incidental Finding: a Case Report
International Journal of Reproduction, Contraception, Obstetrics and Gynecology Jodha BS et al. Int J Reprod Contracept Obstet Gynecol. 2017 Mar;6(3):1132-1135 www.ijrcog.org pISSN 2320-1770 | eISSN 2320-1789 DOI: http://dx.doi.org/10.18203/2320-1770.ijrcog20170600 Case Report Brenner tumor of ovary: an incidental finding: a case report Bhanwar Singh Jodha, Richa Garg* Department of Obstetrics and Gynecology, Umaid Hospital, Regional Institute of Maternal and Child Health, Dr. S. N. Medical College, Jodhpur, Rajasthan, India Received: 20 December 2016 Accepted: 31 January 2017 *Correspondence: Dr. Richa Garg, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Brenner tumor of the ovary is very rare, mostly benign, small, and unilateral. Malignant brenner tumor is much rarer. Malignant brenner tumor of ovary closely resembles the transitional cell carcinoma of ovary. These tumors are believed to arise from urothelial metaplasia of ovarian surface epithelium. However the latter has a worse prognosis. Here we present a case of Brenner tumor of ovary in a postmenopausal woman treated surgically and its features are briefly discussed. Keywords: Brenner tumor, Ovarian neoplasm, Ultrasonography INTRODUCTION bladder epithelium.7 The Brenner tumors are usually small, solid, firm grayish knots up to 2 cm in size, Ovarian tumors are common forms of neoplasia in however, they may also be quite big, and in such cases women and it accounts for about 30.0% of female genital they usually have cystic components as a result of cystic cancers.1 Ovarian carcinoma is the fourth most common degeneration and necrosis.