Toxic Alcohols
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
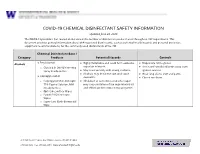
EH&S COVID-19 Chemical Disinfectant Safety Information
COVID-19 CHEMICAL DISINFECTANT SAFETY INFORMATION Updated June 24, 2020 The COVID-19 pandemic has caused an increase in the number of disinfection products used throughout UW departments. This document provides general information about EPA-registered disinfectants, such as potential health hazards and personal protective equipment recommendations, for the commonly used disinfectants at the UW. Chemical Disinfectant Base / Category Products Potential Hazards Controls ● Ethyl alcohol Highly flammable and could form explosive Disposable nitrile gloves Alcohols ● ● vapor/air mixtures. ● Use in well-ventilated areas away from o Clorox 4 in One Disinfecting Spray Ready-to-Use ● May react violently with strong oxidants. ignition sources ● Alcohols may de-fat the skin and cause ● Wear long sleeve shirt and pants ● Isopropyl alcohol dermatitis. ● Closed toe shoes o Isopropyl Alcohol Antiseptic ● Inhalation of concentrated alcohol vapor 75% Topical Solution, MM may cause irritation of the respiratory tract (Ready to Use) and effects on the central nervous system. o Opti-Cide Surface Wipes o Powell PII Disinfectant Wipes o Super Sani Cloth Germicidal Wipe 201 Hall Health Center, Box 354400, Seattle, WA 98195-4400 206.543.7262 ᅵ fax 206.543.3351ᅵ www.ehs.washington.edu ● Formaldehyde Formaldehyde in gas form is extremely Disposable nitrile gloves for Aldehydes ● ● flammable. It forms explosive mixtures with concentrations 10% or less ● Paraformaldehyde air. ● Medium or heavyweight nitrile, neoprene, ● Glutaraldehyde ● It should only be used in well-ventilated natural rubber, or PVC gloves for ● Ortho-phthalaldehyde (OPA) areas. concentrated solutions ● The chemicals are irritating, toxic to humans ● Protective clothing to minimize skin upon contact or inhalation of high contact concentrations. -

Effect of Diethylenetriamine and Triethylamine Sensitization on the Critical Diameter of Nitromethane’
CP505, Shock Compression of Condensed Matter - 1999 edited by M. D. Furnish, L. C. Chhabildas, and R. S. Hixson 0 2000 American Institute of Physics l-56396-923-8/00/$17.00 EFFECT OF DIETHYLENETRIAMINE AND TRIETHYLAMINE SENSITIZATION ON THE CRITICAL DIAMETER OF NITROMETHANE’ J.J. Lee*, J. Jiang?, K.H. Choong’, J.H.S. Lee’ *Graduate Aeronautics Laboratory, California Institute of Technology, Pasadena, CA 9112.5, USA ‘Dept. of Mechanical Engineering, McGill University, Montr&al, Que’bec, Canada, H3A 2K6 In this work, the critical diameter for detonation was measured for Nitromethane (NM) sensitized with two different amines: Diethylenetriamine (DETA) and Triethylamine (TEA). The critical diameter in glass and polyvinylchloride tubes is found to decrease rapidly as the amount of sensitizer is increased, then increase past a critical amount of sensitizer. Thus the critical diameter reaches a minimum at a critical concentration of sensitizer. It was also found that the critical diameter is lower with DETA than with TEA. INTRODUCTION propagation in various tubes and channels, and the critical conditions for propagation in porous media Previous studies have shown that small (3) . concentrations of certain substances can strongly The effect of DETA on the critical diameter of increase the explosive sensitivity nitromethane NM has been reported by Engelke (4), who (NM). Amines are found to be the most effective performed measurements with up to 2.5% DETA by chemical sensitizing agent for NM with mass in NM. Engelke observed a reduction in the ethylenediamine and diethylenetriamine (DETA) critical diameter of over 50% in the range of DETA producing the largest increase in the card gap value concentrations used. -
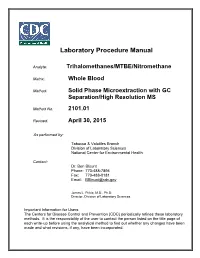
Trihalomethanes/MTBE/Nitromethane Lab Procedure Manual
Laboratory Procedure Manual Analyte: Trihalomethanes/MTBE/Nitromethane Matrix: Whole Blood Method: Solid Phase Microextraction with GC Separation/High Resolution MS Method No: 2101.01 Revised: April 30, 2015 As performed by: Tobacco & Volatiles Branch Division of Laboratory Sciences National Center for Environmental Health Contact: Dr. Ben Blount Phone: 770-488-7894 Fax: 770-488-0181 Email: [email protected] James L. Pirkle, M.D., Ph.D. Director, Division of Laboratory Sciences Important Information for Users The Centers for Disease Control and Prevention (CDC) periodically refines these laboratory methods. It is the responsibility of the user to contact the person listed on the title page of each write-up before using the analytical method to find out whether any changes have been made and what revisions, if any, have been incorporated. THMs & MTBE VOCs in Blood DLS Method Code: 2101.01 National Center for Health Staistics 2 This document details the Lab Protocol for testing the items listed in the following table Data File Name Variable Name SAS Label LBXVBF Blood Bromoform (pg/mL) LBXVBM Blood Bromodichloromethane (pg/mL) VOCMWB_F LBXVCF Blood Chloroform (pg/mL) LBXVCM Blood Dibromochloromethane (pg/mL) LBXVME Blood MTBE (pg/mL) LBXVNM Blood Nitromethane (pg/mL) THMs & MTBE VOCs in Blood DLS Method Code: 2101.01 National Center for Health Staistics 3 1. Clinical Relevance and Summary of Test Principle a. Clinical Relevance The prevalence of disinfection by-products in drinking water supplies has raised concerns about possible adverse health effects from chronic exposure to these potentially carcinogenic compounds. To support studies exploring the relation between exposure to trihalomethanes (THMs), nitromethane (NM: biomarker for halonitromethanes), methyl tert-butyl ether (MTBE) and adverse health effects, an automated analytical method was developed using capillary gas chromatography (GC) and high-resolution mass spectrometry (MS) with selected ion mass detection and isotope-dilution techniques. -

FIA Technical Regulations for Drag Racing
FIA DRAG RACING SECTION 1 - JUNIOR DRAGSTER & JUNIOR FUNNY CAR 2021 Specific Regulations for FIA Drag Racing These Technical Regulations provide guidelines and minimum standards for the construction and operation of vehicles used in FIA Drag Racing. It is the responsibility of the participant to be familiar with the contents of these Technical Regulations and to comply with its requirements. It is not the responsibility of the officials to discover all potential rule compliance issues. The responsibility for compliance with these Technical Regulations rests first and foremost with the competitor. Additional safety equipment or safety-enhancing equipment is always permitted and the levels of safety equipment stated in these Technical Regulations are minimum prescribed levels for a particular type of competition and do not prohibit the individual competitor from using additional safety equipment. Competitors are encouraged to investigate the availability of additional safety devices or equipment for their type of competition. In disputed cases, whether an item, device or piece of equipment is safety-enhancing or performance-enhancing will be determined by the FIA Technical Delegate or the FIA Technical Department. Furthermore, as to performance-enhancing equipment, it is the general principle that unless optional performance-enhancing equipment or performance- related modifications are specifically permitted by these Technical Regulations, they are prohibited. Throughout these Technical Regulations, a number of references are made for particular products and equipment to meet certain standards and specifications (i.e. FIA-Standard, SFI Specs, Snell, DOT, etc.). It is important to realize that these products are manufactured to meet certainspecifications, and upon completion, the manufacturer labels the product as meeting that standard or specification. -

NMR Chemical Shifts of Common Laboratory Solvents As Trace Impurities
7512 J. Org. Chem. 1997, 62, 7512-7515 NMR Chemical Shifts of Common Laboratory Solvents as Trace Impurities Hugo E. Gottlieb,* Vadim Kotlyar, and Abraham Nudelman* Department of Chemistry, Bar-Ilan University, Ramat-Gan 52900, Israel Received June 27, 1997 In the course of the routine use of NMR as an aid for organic chemistry, a day-to-day problem is the identifica- tion of signals deriving from common contaminants (water, solvents, stabilizers, oils) in less-than-analyti- cally-pure samples. This data may be available in the literature, but the time involved in searching for it may be considerable. Another issue is the concentration dependence of chemical shifts (especially 1H); results obtained two or three decades ago usually refer to much Figure 1. Chemical shift of HDO as a function of tempera- more concentrated samples, and run at lower magnetic ture. fields, than today’s practice. 1 13 We therefore decided to collect H and C chemical dependent (vide infra). Also, any potential hydrogen- shifts of what are, in our experience, the most popular bond acceptor will tend to shift the water signal down- “extra peaks” in a variety of commonly used NMR field; this is particularly true for nonpolar solvents. In solvents, in the hope that this will be of assistance to contrast, in e.g. DMSO the water is already strongly the practicing chemist. hydrogen-bonded to the solvent, and solutes have only a negligible effect on its chemical shift. This is also true Experimental Section for D2O; the chemical shift of the residual HDO is very NMR spectra were taken in a Bruker DPX-300 instrument temperature-dependent (vide infra) but, maybe counter- (300.1 and 75.5 MHz for 1H and 13C, respectively). -

Expert Consensus Guidelines for Stocking of Antidotes in Hospitals That Provide Emergency Care
TOXICOLOGY/CONCEPTS Expert Consensus Guidelines for Stocking of Antidotes in Hospitals That Provide Emergency Care Richard C. Dart, MD, PhD From the Rocky Mountain Poison & Drug Center - Denver Health, Denver, CO (Dart, Heard, Schaeffer, Stephen W. Borron, MD, MS Bogdan, Alhelail, Buchanan, Hoppe, Lavonas, Mlynarchek, Phua, Rhyee, Varney, Zosel); Department of E. Martin Caravati, MD, MPH Surgery, University of Texas Health Sciences Center, San Antonio, TX (Borron); Division of Emergency Daniel J. Cobaugh, PharmD Medicine, Utah Poison Control Center, University of Utah Health Sciences Center, Salt Lake City, UT Steven C. Curry, MD (Caravati); ASHP Research and Education Foundation, Bethesda, MD (Cobaugh); Department of Jay L. Falk, MD Medical Toxicology and Banner Poison Control Center, Banner Good Samaritan Medical Center, Lewis Goldfrank, MD Phoenix, AZ (Curry); Department of Emergency Medicine, Orlando Regional Medical Center, University of Susan E. Gorman, PharmD, MS Florida, Orlando, FL (Falk); New York City Poison Center; New York University School of Medicine, New Stephen Groft, PharmD York, NY (Goldfrank); Division of Strategic National Stockpile, Centers for Disease Control and Kennon Heard, MD Prevention, Atlanta, GA (Gorman); Office of Rare Diseases Research, Bethesda, MD (Groft); Division of Ken Miller, MD, PhD Emergency Medicine, School of Medicine (Dart, Heard, Lavonas, Schaeffer) and Department of Kent R. Olson, MD Pharmaceutical Sciences, School of Pharmacy (Bogdan), University of Colorado Denver, Aurora, CO; Gerald O’Malley, DO Orange County Fire Authority and Orange County Health Care Agency Emergency Medical Services, Donna Seger, MD Irvine, CA, and National Association of EMS Physicians, Lenexa, KS, (Miller); University of California, Steven A. Seifert, MD San Francisco, and San Francisco Division, California Poison Control System, San Francisco, CA Marco L. -

Detoxification of Lignocellulose-Derived Microbial Inhibitory Compounds by Clostridium Beijerinckii NCIMB 8052 During Acetone-Butanol-Ethanol Fermentation
Detoxification of Lignocellulose-derived Microbial Inhibitory Compounds by Clostridium beijerinckii NCIMB 8052 during Acetone-Butanol-Ethanol Fermentation DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Yan Zhang Graduate Program in Animal Sciences The Ohio State University 2013 Dissertation Committee: Thaddeus C. Ezeji, Advisor Steven C. Loerch Sandra G. Velleman Zhongtang Yu Venkat Gopalan Copyrighted by Yan Zhang 2013 Abstract Pretreatment and hydrolysis of lignocellulosic biomass to fermentable sugars generate a complex mixture of microbial inhibitors such as furan aldehydes (e.g., furfural), which at sublethal concentration in the fermentation medium can be tolerated or detoxified by acetone butanol ethanol (ABE)-producing Clostridium beijerinckii NCIMB 8052. The response of C. beijerinckii to furfural at the molecular level, however, has not been directly studied. Therefore, this study was to elucidate mechanism employed by C. beijerinckii to detoxify lignocellulose-derived microbial inhibitors and use this information to develop inhibitor-tolerant C. beijerinckii. Towards the long-term goal of developing inhibitor-tolerant Clostridium strains, the first objective was to evaluate ABE fermentation by C. beijerinckii using different proportions of Miscanthus giganteus hydrolysates as carbon source. Compared to the growth of C. beijerinckii in control medium, C. beijerinckii experienced different degrees of inhibition. The degree of inhibition was dose-dependent, and C. beijerinckii did not grow in P2 medium with greater than 25% (v/v) Miscanthus giganteus hydrolysates. To improve tolerance of C. beijerinckii to inhibitors, supplementation of P2 medium with undiluted (100%) Miscanthus giganteus hydrolysates with 4 g/L CaCO3 resulted in successful growth of and ABE production by C. -

Reactions of Alcohols & Ethers 1
REACTIONS OF ALCOHOLS & ETHERS 1. Combustion (Extreme Oxidation) alcohol + oxygen carbon dioxide + water 2 CH3CH2OH + 6 O2 4 CO2 + 6 H2O 2. Elimination (Dehydration) ° alcohol H 2 S O 4/ 1 0 0 C alkene + water H2SO4/100 ° C CH3CH2CH2OH CH3CH=CH2 + H2O 3. Condensation ° excess alcohol H 2 S O 4 / 1 4 0 C ether + water H2SO4/140 ° C 2 CH3CH2OH CH3CH2OCH2CH3 + H2O 4. Substitution Lucas Reagent alcohol + hydrogen halide Z n C l2 alkyl halide + water ZnCl2 CH3CH2OH + HCl CH3CH2Cl + H2O • This reaction with the Lucas Reagent (ZnCl2) is a qualitative test for the different types of alcohols because the rate of the reaction differs greatly for a primary, secondary and tertiary alcohol. • The difference in rates is due to the solubility of the resulting alkyl halides • Tertiary Alcohol→ turns cloudy immediately (the alkyl halide is not soluble in water and precipitates out) • Secondary Alcohol → turns cloudy after 5 minutes • Primary Alcohol → takes much longer than 5 minutes to turn cloudy 5. Oxidation • Uses an oxidizing agent such as potassium permanganate (KMnO4) or potassium dichromate (K2Cr2O7). • This reaction can also be used as a qualitative test for the different types of alcohols because there is a distinct colour change. dichromate → chromium 3+ (orange) → (green) permanganate → manganese (IV) oxide (purple) → (brown) Tertiary Alcohol not oxidized under normal conditions CH3 KMnO4 H3C C OH NO REACTION K2Cr2O7 CH3 tertbutyl alcohol Secondary Alcohol ketone + hydrogen ions H O KMnO4 H3C C CH3 + K2Cr2O7 C + 2 H H3C CH3 OH propanone 2-propanol Primary Alcohol aldehyde + water carboxylic acid + hydrogen ions O KMnO4 O H H KMnO H H 4 + CH3CH2CH2OH C C C H C C C H + 2 H K2Cr2O7 + H2O K Cr O H H H 2 2 7 HO H H 1-propanol propanal propanoic acid 6. -

Recommended Methods for the Purification of Solvents and Tests for Impurities Nitromethane
Pure & App!. Chem., Vol. 58, No. 11, pp. 1541—1545, 1986. Printed in Great Britain. © 1986 IUPAC INTERNATIONALUNION OF PURE AND APPLIED CHEMISTRY ANALYTICAL CHEMISTRY DIVISION COMMISSION ON ELECTROANALYTICAL CHEMISTRY* RECOMMENDED METHODS FOR THE PURIFICATION OF SOLVENTS AND TESTS FOR IMPURITIES NITROMETHANE Prepared for publication by J. F. COETZEE and T.-H. CHANG Department of Chemistry, University of Pittsburgh, PA 15260, USA *Membership of the Commission during 1983—85 when the report was prepared was as follows: Chairman: J. Jordan (USA); Secretary: K. Izutsu (Japan); Titular Members: A. K. Covington (UK); J. Juillard (France); R. C. Kapoor (India); E. Pungor (Hungary); Associate Members: W. Davison (UK); R. A. Durst (USA); M. Gross (France); K. M. Kadish (USA); R. Kalvoda (Czechoslovakia); H. Kao (China); Y. Marcus (Israel); T. Mussini (Italy); H. W. NUrnberg (FRG); M. Senda (Japan); N. Tanaka (Japan); K. Tóth (Hungary); National Representatives: D. D. Perrin (Australia); B. Gilbert (Belgium); W. C. Purdy (Canada); A. A. Vlek (Czecho- slovakia); H. Monien (FRG); M. L'Her (France); Gy. Farsang (Hungary); H. C. Gaur (India); W. F. Smyth (Ireland); E. Grushka (Israel); S. R. Cavallari (Italy); W. Frankvoort (Netherlands); Z. Galus (Poland); G. Johansson (Sweden); J. Buffle (Switzerland); H. Thompson (UK); J. G. Osteryoung (USA); I. Piljac (Yugoslavia). Republication of this report is permitted without the need for formal IUPAC permission on condition that an acknowledgement, with full reference together with JUPAC copyright symbol (© 1986 JUPAC), is printed. Publication of a translation into another language is subject to the additional condition of prior approval from the relevant JUPAC NationalAdhering Organization. Recommended methods for the purification of solvents and tests for impurities: nitromethane Themost significant solvent properties of nitromethane are discussed. -

Download Author Version (PDF)
Dalton Transactions Evaluation of Chemo- and Shape-Selective Association of a Bowl-Type Dodecavanadate Cage with an Electron-Rich Group Journal: Dalton Transactions Manuscript ID DT-ART-01-2019-000462.R1 Article Type: Paper Date Submitted by the 22-Mar-2019 Author: Complete List of Authors: Kikukawa, Yuji; Kanazawa University; JST PRESTO Kitajima, Hiromasa; Kanazawa University Hayashi, Yoshihito; Kanazawa University, Chemistry Page 1 of 6 PleaseDalton do not Transactions adjust margins Journal Name ARTICLE Evaluation of Chemo- and Shape-Selective Association of a Bowl- Type Dodecavanadate Cage with an Electron-Rich Group ab b b Received 00th January 20xx, Yuji Kikukawa, * Hiromasa Kitajima, and Yoshihito Hayashi Accepted 00th January 20xx The host-guest interaction between a half spherical-type dodecavanadate (V12) and a neutral molecule guest was evaluated DOI: 10.1039/x0xx00000x by monitoring the flip of a VO5 unit caused by the presence or absence of a guest in the cavity of V12. In N,N- www.rsc.org/ dimethylformamide (DMF), V12 adopted the guest-free-form (V12-free). By addition of several guest molecules, such as acetonitrile, nitromethane, dichloromethane, the structure conversion to the guest-inserted form (V12(guest)) were observed with the affinity constants of 137±10, 0.14±0.1, and 0.15±0.1 M−1, respectively. In the case of 1,2-dichloroethane, 1,2-dibromoethane, and 1,2-diiodoethane, the constants were 35±5, 114±5, and 2.1±0.5 M−1, respectively, suggesting that the bromo group is best fit to the cavity of the bowl. A cyclic carbonate and 5- and 6-membered lactons, cycrobutanone, and hexanal were inserted to the V12 host, while non-cyclic carbonate, non-cyclic and 7-membered cyclic ester, ketone with a 6-membered ring, and benzaldehyde showed no effect on the guest insertion. -

Chemical Disinfectants | Disinfection & Sterilization Guidelines | Guidelines Library | Infection Control | CDC 3/19/20, 14:52
Chemical Disinfectants | Disinfection & Sterilization Guidelines | Guidelines Library | Infection Control | CDC 3/19/20, 14:52 Infection Control Chemical Disinfectants Guideline for Disinfection and Sterilization in Healthcare Facilities (2008) Alcohol Overview. In the healthcare setting, “alcohol” refers to two water-soluble chemical compounds—ethyl alcohol and isopropyl alcohol —that have generally underrated germicidal characteristics 482. FDA has not cleared any liquid chemical sterilant or high- level disinfectant with alcohol as the main active ingredient. These alcohols are rapidly bactericidal rather than bacteriostatic against vegetative forms of bacteria; they also are tuberculocidal, fungicidal, and virucidal but do not destroy bacterial spores. Their cidal activity drops sharply when diluted below 50% concentration, and the optimum bactericidal concentration is 60%–90% solutions in water (volume/volume) 483, 484. Mode of Action. The most feasible explanation for the antimicrobial action of alcohol is denaturation of proteins. This mechanism is supported by the observation that absolute ethyl alcohol, a dehydrating agent, is less bactericidal than mixtures of alcohol and water because proteins are denatured more quickly in the presence of water 484, 485. Protein denaturation also is consistent with observations that alcohol destroys the dehydrogenases of Escherichia coli 486, and that ethyl alcohol increases the lag phase of Enterobacter aerogenes 487 and that the lag phase e!ect could be reversed by adding certain amino acids. The bacteriostatic action was believed caused by inhibition of the production of metabolites essential for rapid cell division. Microbicidal Activity. Methyl alcohol (methanol) has the weakest bactericidal action of the alcohols and thus seldom is used in healthcare 488. The bactericidal activity of various concentrations of ethyl alcohol (ethanol) was examined against a variety of microorganisms in exposure periods ranging from 10 seconds to 1 hour 483. -

Alcohols I 1400
ALCOHOLS I 1400 Table 1 MW: Table 1 CAS: Table 2 RTECS: Table 2 METHOD: 1400, Issue 2 EVALUATION: PARTIAL Issue 1: 15 February 1984 Issue 2: 15 August 1994 OSHA : Table 2 PROPERTIES: Table 1 NIOSH: Table 2 ACGIH: Table 2 COMPOUNDS AND SYNONYMS: (1) ethanol: ethyl alcohol. (2) isopropyl alcohol: 2-propanol. (3) tert-butyl alcohol: 2-methyl-2-propanol. SAMPLING MEASUREMENT SAMPLER: SOLID SORBENT TUBE TECHNIQUE: GAS CHROMATOGRAPHY, FID (coconut shell charcoal, 100 mg/50 mg) ANALYTE: compounds above FLOW RATE: 0.01 to 0.2 L/min (£0.05 L/min for ethyl alcohol) DESORPTION: 1 mL 1% 2-butanol in CS 2 (1) (2) (3) INJECTION VOL-MIN: 0.1 L 0.3 L 1.0 L VOLUME: 5 µL -MAX: 1 L 3 L 10 L TEMPERATURE-INJECTION: 200 °C SHIPMENT: cooled -DETECTOR: 250-300 °C -COLUMN: 65-70 °C SAMPLE STABILITY: unknown, store in freezer CARRIER GAS: N2 or He, 30 mL/min BLANKS: 2 to 10 field blanks per set COLUMN: glass, 2 m x 4-mm ID, 0.2% Carbowax 1500 on 60/80 Carbopack C or equivalent ACCURACY CALIBRATION: solutions of analyte in eluent (internal standard optional) RANGE STUDIED: see EVALUATION OF METHOD RANGE AND BIAS: not significant [1] PRECISION: see EVALUATION OF METHOD OVERALL PRECISION (S ˆ ): see EVALUATION OF METHOD rT ESTIMATED LOD: 0.01 mg per sample [2] ACCURACY: ± 14% APPLICABILITY: The working ranges are 16 to 1000 ppm ethanol (30 to 1900 mg/m 3) for a 1-L air sample; 4 to 400 ppm isopropyl alcohol (10 to 1000 mg/m 3) for a 3-L air sample; and 1 to 100 ppm t-butyl alcohol (3 to 300 mg/m 3) for a 10-L air sample.