Understanding Your MULTIPLE MYELOMA LAB TESTS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of Abnormal Liver Chemistries
ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries Paul Y. Kwo, MD, FACG, FAASLD1, Stanley M. Cohen, MD, FACG, FAASLD2, and Joseph K. Lim, MD, FACG, FAASLD3 1Division of Gastroenterology/Hepatology, Department of Medicine, Stanford University School of Medicine, Palo Alto, California, USA; 2Digestive Health Institute, University Hospitals Cleveland Medical Center and Division of Gastroenterology and Liver Disease, Department of Medicine, Case Western Reserve University School of Medicine, Cleveland, Ohio, USA; 3Yale Viral Hepatitis Program, Yale University School of Medicine, New Haven, Connecticut, USA. Am J Gastroenterol 2017; 112:18–35; doi:10.1038/ajg.2016.517; published online 20 December 2016 Abstract Clinicians are required to assess abnormal liver chemistries on a daily basis. The most common liver chemistries ordered are serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase and bilirubin. These tests should be termed liver chemistries or liver tests. Hepatocellular injury is defined as disproportionate elevation of AST and ALT levels compared with alkaline phosphatase levels. Cholestatic injury is defined as disproportionate elevation of alkaline phosphatase level as compared with AST and ALT levels. The majority of bilirubin circulates as unconjugated bilirubin and an elevated conjugated bilirubin implies hepatocellular disease or cholestasis. Multiple studies have demonstrated that the presence of an elevated ALT has been associated with increased liver-related mortality. A true healthy normal ALT level ranges from 29 to 33 IU/l for males, 19 to 25 IU/l for females and levels above this should be assessed. The degree of elevation of ALT and or AST in the clinical setting helps guide the evaluation. -

Total Bilirubin in Athletes, Determination of Reference Range
OriginalTotal bilirubin Paper in athletes DOI: 10.5114/biolsport.2017.63732 Biol. Sport 2017;34:45-48 Total bilirubin in athletes, determination of reference range AUTHORS: Witek K1, Ścisłowska J2, Turowski D1, Lerczak K1, Lewandowska-Pachecka S2, Corresponding author: Pokrywka A3 Konrad Witek Department of Biochemistry, Institute of Sport - National 1 Department of Biochemistry, Institute of Sport - National Research Institute, Warsaw, Poland Research Institute 2 01-982 Warsaw, Poland Faculty of Pharmacy with the Laboratory Medicine Division, Medical University of Warsaw, Poland 3 E-mail: Department of Biochemistry, 2nd Faculty of Medicine, Medical University of Warsaw, Poland [email protected] ABSTRACT: The purpose of this study was to determine a typical reference range for the population of athletes. Results of blood tests of 339 athletes (82 women and 257 men, aged 18-37 years) were retrospectively analysed. The subjects were representatives of different sports disciplines. The measurements of total bilirubin (BIT), iron (Fe), alkaline phosphatase (ALP), alanine aminotransferase (ALT) and gamma-glutamyltransferase (GGT) were made using a Pentra 400 biochemical analyser (Horiba, France). Red blood cell count (RBC), reticulocyte count and haemoglobin concentration measurements were made using an Advia 120 haematology analyser (Siemens, Germany). In groups of women and men the percentage of elevated results were similar at 18%. Most results of total bilirubin in both sexes were in the range 7-14 μmol ∙ L-1 (49% of women and 42% of men). The highest results of elevated levels of BIT were in the range 21-28 μmol ∙ L-1 (12% of women and 11% of men). There was a significant correlation between serum iron and BIT concentration in female and male athletes whose serum total bilirubin concentration does not exceed the upper limit of the reference range. -

Supplementary Information Changes in the Plasma Proteome At
Supplementary Information Changes in the plasma proteome at asymptomatic and symptomatic stages of autosomal dominant Alzheimer’s disease Julia Muenchhoff1, Anne Poljak1,2,3, Anbupalam Thalamuthu1, Veer B. Gupta4,5, Pratishtha Chatterjee4,5,6, Mark Raftery2, Colin L. Masters7, John C. Morris8,9,10, Randall J. Bateman8,9, Anne M. Fagan8,9, Ralph N. Martins4,5,6, Perminder S. Sachdev1,11,* Supplementary Figure S1. Ratios of proteins differentially abundant in asymptomatic carriers of PSEN1 and APP Dutch mutations. Mean ratios and standard deviations of plasma proteins from asymptomatic PSEN1 mutation carriers (PSEN1) and APP Dutch mutation carriers (APP) relative to reference masterpool as quantified by iTRAQ. Ratios that significantly differed are marked with asterisks (* p < 0.05; ** p < 0.01). C4A, complement C4-A; AZGP1, zinc-α-2-glycoprotein; HPX, hemopexin; PGLYPR2, N-acetylmuramoyl-L-alanine amidase isoform 2; α2AP, α-2-antiplasmin; APOL1, apolipoprotein L1; C1 inhibitor, plasma protease C1 inhibitor; ITIH2, inter-α-trypsin inhibitor heavy chain H2. 2 A) ADAD)CSF) ADAD)plasma) B) ADAD)CSF) ADAD)plasma) (Ringman)et)al)2015)) (current)study)) (Ringman)et)al)2015)) (current)study)) ATRN↓,%%AHSG↑% 32028% 49% %%%%%%%%HC2↑,%%ApoM↓% 24367% 31% 10083%% %%%%TBG↑,%%LUM↑% 24256% ApoC1↓↑% 16565% %%AMBP↑% 11738%%% SERPINA3↓↑% 24373% C6↓↑% ITIH2% 10574%% %%%%%%%CPN2↓%% ↓↑% %%%%%TTR↑% 11977% 10970% %SERPINF2↓↑% CFH↓% C5↑% CP↓↑% 16566% 11412%% 10127%% %%ITIH4↓↑% SerpinG1↓% 11967% %%ORM1↓↑% SerpinC1↓% 10612% %%%A1BG↑%%% %%%%FN1↓% 11461% %%%%ITIH1↑% C3↓↑% 11027% 19325% 10395%% %%%%%%HPR↓↑% HRG↓% %%% 13814%% 10338%% %%% %ApoA1 % %%%%%%%%%GSN↑% ↓↑ %%%%%%%%%%%%ApoD↓% 11385% C4BPA↓↑% 18976%% %%%%%%%%%%%%%%%%%ApoJ↓↑% 23266%%%% %%%%%%%%%%%%%%%%%%%%%%ApoA2↓↑% %%%%%%%%%%%%%%%%%%%%%%%%%%%%A2M↓↑% IGHM↑,%%GC↓↑,%%ApoB↓↑% 13769% % FGA↓↑,%%FGB↓↑,%%FGG↓↑% AFM↓↑,%%CFB↓↑,%% 19143%% ApoH↓↑,%%C4BPA↓↑% ApoA4↓↑%%% LOAD/MCI)plasma) LOAD/MCI)plasma) LOAD/MCI)plasma) LOAD/MCI)plasma) (Song)et)al)2014)) (Muenchhoff)et)al)2015)) (Song)et)al)2014)) (Muenchhoff)et)al)2015)) Supplementary Figure S2. -
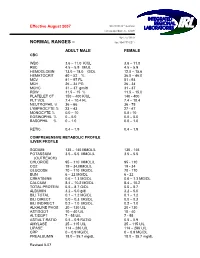
Normal Rangesа–А
Effective August 2007 5361 NW 33 rd Avenue Fort Lauderdale, FL 33309 954-777-0018 NORMAL RANGES – fax: 954-777-0211 ADULT MALE FEMALE CBC WBC 3.6 – 11.0 K/UL 3.6 – 11.0 RBC 4.5 – 5.9 M/UL 4.5 – 5.9 HEMOGLOBIN 13.0 – 18.0 G/DL 12.0 – 15.6 HEMATOCRIT 40 – 52 % 36.0 – 46.0 MCV 81 – 97 FL 81 93 MCH 26 – 34 PG 26 34 MCHC 31 – 37 gm/dl 31 37 RDW 11.5 – 15 % 11.5 – 15.0 PLATELET CT 150 – 400 K/UL 140 400 PLT VOL 7.4 – 10.4 FL 7.4 – 10.4 NEUTROPHIL % 36 – 66 36 75 LYMPHOCYTE % 23 – 43 27 47 MONOCYTE % 0.0 – 10 0.0 10 EOSINOPHIL % 0 – 5.0 0.0 – 5.0 BASOPHIL % 0 – 1.0 0.0 – 1.0 RETIC 0.4 – 1.9 0.4 – 1.9 COMPREHENSIVE METABOLIC PROFILE /LIVER PROFILE SODIUM 135 – 145 MMOL/L 135 145 POTASSIUM 3.5 – 5.5 MMOL/L 3.5 – 5.5 (OUTREACH) CHLORIDE 95 – 110 MMOL/L 95 110 CO2 19 – 34.MMOL/L 19 34 GLUCOSE 70 – 110 MG/DL 70 110 BUN 6 – 22 MG/DL 6 22 CREATININE 0.6 – 1.3 MG/DL 0.6 – 1.3 MG/DL CALCIUM 8.4 – 10.2 MG/DL 8.4 – 10.2 TOTAL PROTEIN 5.5 – 8.7 G/DL 5.5 – 8.7 ALBUMIN 3.2 – 5.0 g/dl 3.2 – 5.0 BILI TOTAL 0.1 – 1.2 MG/DL 0.1 – 1.2 BILI DIRECT 0.0 – 0.3 MG/DL 0.0 – 0.3 BILI INDIRECT 0.2 – 1.0 MG/DL 0.2 – 1.0 ALKALINE PHOS 20 – 130 U/L 20 130 AST/SGOT 10 – 40 U/L 10 40 ALT/SGPT 7 55 U/L 7 55 AST/ALT RATIO 0.5 – 0.9 RATIO 0.5 – 0.9 AMYLASE 25 – 115 U/L 25 – 115 U/L LIPASE 114 – 286 U/L 114 – 286 U/L CRP 0 – 0.9 MG/DL 0 – 0.9 MG/DL PREALBUMIN 18.0 – 35.7 mg/dL 18.0 – 35.7 mg/dL Revised 807 MAGNESIUM 1.8 – 2.4 mg/dL 1.8 – 2.4 mg/Dl LDH 100 – 200 Units /L 100 – 200 Units/L PHOSPHOROUS 2.3 – 5.0 mg/dL 2.3 – 5.0 mg/dL LACTIC ACID 0.4 -
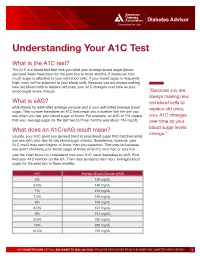
Understanding Your A1C Test
Diabetes Advisor Understanding Your A1C Test What is the A1C test? The A1C is a blood test that tells you what your average blood sugar (blood glucose) levels have been for the past two to three months. It measures how much sugar is attached to your red blood cells. If your blood sugar is frequently high, more will be attached to your blood cells. Because you are always making new red blood cells to replace old ones, your A1C changes over time as your blood sugar levels change. “Because you are always making new What is eAG? red blood cells to eAG stands for estimated average glucose and is your estimated average blood replace old ones, sugar. This number translates an A1C test result into a number like the one you see when you test your blood sugar at home. For example, an A1C of 7% means your A1C changes that your average sugar for the last two to three months was about 154 mg/dL. over time as your What does an A1C/eAG result mean? blood sugar levels change.” Usually, your A1C gives you general trend in your blood sugar that matches what you see with your day-to-day blood sugar checks. Sometimes, however, your A1C result may seem higher or lower than you expected. That may be because you aren’t checking your blood sugar at times when it’s very high or very low. Use the chart below to understand how your A1C result translates to eAG. First find your A1C number on the left. -

Serological (Antibody) Testing for Covid-19
SEROLOGICAL (ANTIBODY) TESTING FOR COVID-19 Serological tests detect antibodies in the blood People in the early stages of COVID-19 might generated as part of the immune response test antibody negative despite being highly to a specific infection, such as infection with infectious. Additionally, some tests might give a SARS-CoV-2, the virus that causes COVID-19. false positive result because of past or present Antibody tests are different from tests such as infection with other types of coronaviruses. polymerase chain reaction (PCR) and antigen False positive results are also more likely tests which detect the SARS-CoV-2 virus. when the percentage of the population with Many new serological tests for COVID-19 have the disease is low. The Idaho Division of Public been developed and have an emergency use Health discourages persons who have a positive authorization (EUA) from the U.S. Food and serology test from relaxing the precautions such Drug Administration (FDA). Only antibody tests as social distancing that are recommended for that have an FDA EUA should be used. The all Idahoans to prevent spread of coronavirus, Idaho Division of Public Health discourages and strongly discourages employers form the use of unauthorized serology-based assays relaxing the employee protections for an for diagnosis of COVID-19 or determining if employee solely based upon a positive serology someone is currently infected or had a prior test. infection. The immune response to SARS-CoV-2 (the Serological tests are not recommended for virus that causes COVID-19) infection is not COVID-19 diagnosis in most situations because well understood. -
Effect of Thyroid Hormones on Kidney Function in Patients After
www.nature.com/scientificreports OPEN Efect of Thyroid Hormones on Kidney Function in Patients after Kidney Transplantation Benjamin Schairer1, Viktoria Jungreithmayr2, Mario Schuster2, Thomas Reiter 1, Harald Herkner3, Alois Gessl4, Gürkan Sengölge1* & Wolfgang Winnicki 1 Elevated levels of thyroid-stimulating-hormone (TSH) are associated with reduced glomerular fltration rate (GFR) and increased risk of developing chronic kidney disease even in euthyroid patients. Thyroid hormone replacement therapy has been shown to delay progression to end-stage renal disease in sub-clinically hypothyroid patients with renal insufciency. However, such associations after kidney transplantation were never investigated. In this study the association of thyroid hormones and estimated GFR (eGFR) in euthyroid patients after kidney transplantation was analyzed. In total 398 kidney transplant recipients were assessed retrospectively and association between thyroid and kidney function parameters at and between defned time points, 12 and 24 months after transplantation, was studied. A signifcant inverse association was shown for TSH changes and eGFR over time between months 12 and 24 post transplantation. For each increase of TSH by 1 µIU/mL, eGFR decreased by 1.34 mL/min [95% CI, −2.51 to −0.16; p = 0.03], corresponding to 2.2% eGFR decline, within 12 months. At selected time points 12 and 24 months post transplantation, however, TSH was not associated with eGFR. In conclusion, an increase in TSH between 12 and 24 months after kidney transplantation leads to a signifcant decrease in eGFR, which strengthens the concept of a kidney- thyroid-axis. Interactions between thyroid hormones and kidney function have been suggested in previous studies. -
Jaundice Protocol
fighting childhood liver disease Jaundice Protocol Early identification and referral of liver disease in infants fighting childhood liver disease 36 Great Charles Street Birmingham B3 3JY Telephone: 0121 212 3839 yellowalert.org childliverdisease.org [email protected] Registered charity number 1067331 (England & Wales); SC044387 (Scotland) The following organisations endorse the Yellow Alert Campaign and are listed in alphabetical order. 23957 CLDF Jaundice Protocol.indd 1 03/08/2015 18:25:24 23957 3 August 2015 6:25 PM Proof 1 1 INTRODUCTION This protocol forms part of Children’s Liver Disease Foundation’s (CLDF) Yellow Alert Campaign and is written to provide general guidelines on the early identification of liver disease in infants and their referral, where appropriate. Materials available in CLDF’s Yellow Alert Campaign CLDF provides the following materials as part of this campaign: • Yellow Alert Jaundice Protocol for community healthcare professionals • Yellow Alert stool colour book mark for quick and easy reference • Parents’ leaflet entitled “Jaundice in the new born baby”. CLDF can provide multiple copies to accompany an antenatal programme or for display in clinics • Yellow Alert poster highlighting the Yellow Alert message and also showing the stool chart 2 GENERAL AWARENESS AND TRAINING The National Institute of Health and Clinical Excellence (NICE) has published a clinical guideline on neonatal jaundice which provides guidance on the recognition, assessment and treatment of neonatal jaundice in babies from birth to 28 days. Neonatal Jaundice Clinical Guideline guidance.nice.org.uk cg98 For more information go to nice.org.uk/cg98 • Jaundice Community healthcare professionals should be aware that there are many causes for jaundice in infants and know how to tell them apart: • Physiological jaundice • Breast milk jaundice • Jaundice caused by liver disease • Jaundice from other causes, e.g. -
Understanding Your Blood Test Lab Results
Understanding Your Blood Test Lab Results A comprehensive "Health Panel" has been designed specifically to screen for general abnormalities in the blood. This panel includes: General Chemistry Screen or (SMAC), Complete Blood Count or (CBC), and Lipid examination. A 12 hour fast from all food and drink (water is allowed) is required to facilitate accurate results for some of the tests in this panel. Below, is a breakdown of all the components and a brief explanation of each test. Abnormal results do not necessarily indicate the presence of disease. However, it is very important that these results are interpreted by your doctor so that he/she can accurately interpret the findings in conjunction with your medical history and order any follow-up testing if needed. The Bernards Township Health Department and the testing laboratory cannot interpret these results for you. You must speak to your doctor! 262 South Finley Avenue Basking Ridge, NJ 07920 www.bernardshealth.org Phone: 908-204-2520 Fax: 908-204-3075 1 Chemistry Screen Components Albumin: A major protein of the blood, albumin plays an important role in maintaining the osmotic pressure spleen or water in the blood vessels. It is made in the liver and is an indicator of liver disease and nutritional status. A/G Ratio: A calculated ratio of the levels of Albumin and Globulin, 2 serum proteins. Low A/G ratios can be associated with certain liver diseases, kidney disease, myeloma and other disorders. ALT: Also know as SGPT, ALT is an enzyme produced by the liver and is useful in detecting liver disorders. -

Clotting Phenomena at the Blood-Polymer Interface and Development of Blood Compatible Polymeric Surfaces
Clotting Phenomena at the Blood-Polymer Interface and Development of Blood Compatible Polymeric Surfaces Adriaan Bantjes In the past two decades many attempts have been made to relate surface and interfacial parameters with the blood compatibility of polymeric surfaces. It is however doubtful if by a single parameter the behaviour of blood on a surface can be predicted. Two major aspects of blood compatibility -- the prevention of platelet adhesion and the deactivation of the intrinsic coagulation system are determined by the measure and nature of competi- tive blood protein adsorption on the foreign surface. The adhesion of blood platelets is promoted by adsorbed fibrinogen and gamma globulin, while adsorbed albumin inhibits platelct adhesion. Heparinised surfaces do not adsorb fibrin and consequently no adhesion of platelets takes place. Othcr surfaces with low platelct adhesion are the hydrogels, certain block copolyetherurethanes, polyelectrolyte complexes and biolised proteins. Heparinised surfaces of the cationically bonded type inhibit the intrinsic coagulation as well, however this may be due to unstable coatings and heparin leakage. In the authors laboratory a synthetic heparinoid was prepared with the structure - [CH, - C(CH3) NHS03Na ~ C(H) COONa ~ CH2 --] with h, = (7.5 5 1 .O) x lo5 and an in vivo anticoagulant activity of 50% of heparin. Its coatings on PVC, using tridodecyltiietliyl-ammoniuni chloridc as a coupling agent, are stable in plasma and salt solutions and provide surfaces which show negligible platelet adhesion and a strong inhibition 01 the intrinsic coagulation on contact with blood. Similar results were found with polydimethylsiloxane surfaces coated with this heparinoid. 1. INTRODUCTION new blood compatible materials may be developed it is necessary to explain sotne of the mechanisms of blood co- The clinical use of blood contacting devices and prosthcses is agulation on intcraction with a foreign surface. -

Wellness Labs Explanation of Results
WELLNESS LABS EXPLANATION OF RESULTS BASIC METABOLIC PANEL BUN – Blood Urea Nitrogen (BUN) is a waste product of protein breakdown and is produced when excess protein in your body is broken down and used for energy. BUN levels greater than 50 mg/dL generally means that the kidneys are not functioning normally. Abnormally low BUN levels can be seen with malnutrition and liver failure. Creatinine – a waste product of normal muscle activity. High creatinine levels are most commonly seen in kidney failure and can also been seen with hyperthyroidism, conditions of overgrowth of the body, rhabdomyolysis, and early muscular dystrophy. Low creatinine levels can indicate low muscle mass associated with malnutrition and late-stage muscular dystrophy. Glucose – a simple sugar that serves as the main source of energy in the body. High glucose levels (hyperglycemia) is usually associated with prediabetes and can also occur with severe stress on the body such as surgery or events like stroke or trauma. High levels can also be seen with overactive thyroid, pancreatitis, or pancreatic cancer. Low glucose levels can occur with underactive thyroid and rare insulin- secreting tumors. Electrolytes – Sodium, Calcium, Potassium, Chloride, and Carbon Dioxide are all included in this category. Sodium – high levels of sodium can be seen with dehydration, excessive thirst, and urination due to abnormally low levels of antidiuretic hormone (diabetes insipidus) as well as with excessive levels of cortisol in the body (Cushing syndrome). Low levels of sodium can be seen with congestive heart failure, cirrhosis of the liver, kidney failure, and the syndrome of inappropriate antidiuretic hormone (SIADH). -

The Effect of Gamma Globulin in Pustular Acne*
PRELIMINARY AND SHORT REPORT THE EFFECT OF GAMMA GLOBULIN IN PUSTULAR ACNE* LOREN W.SHAFFER,M.D., BENJAMIN SdHWIMMER, M.D. AND RENATO J.STANICCO,M.D. One of us (LWS) bad occasion to treat a young Clinical Response: Patient 1: New lesions ceased white man with gamma globulin for prophylaxisappearing immediately after the first injection. after exposure to infectious hepatitis. He wasBy the third week most of the cystic and pustular given two injections, 10 cc. each, of human Polio-lesions had dried up, and no new ones had ap- myelitis Immune Globulin, one week apart. Itpeared. Comedones were not decreased in number. was observed that shortly after the second injec-The patient maintained his improvement through tion, his severe pustular and indurated acnethe fifth week when the cystic and pustular lesions improved considerably. This observation led tobegan to recur. the present study, of which this is a preliminary Patient 2: New lesions continued to develop report. throughout the period of treatment and the one This study of the therapeutic effect of gammamonth follow up. globulin in pustular acne is coupled with a study Patient 3: There was no observable effect of of the serum protein and C-reactive protein levelstreatment. before and after treatment. Patient 4: The first improvement was seen in Method: Four patients in their late teens, other-the second week and by the third, all cystic and wise healthy, but with severe pustular and cysticpustular lesions were dry. The improvement acne that had been resistant to conventionallasted for two weeks after which the lesions methods of treatment were selected for the study.began to return.