Our Briefing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Leading the Way Fight Night Rescheduled
Thursday, July 9, 2020 Since Sept 27, 1879 Retail $2.20 Home delivered from $1.40 THE INDEPENDENT VOICE OF MID CANTERBURY Leading Fight Night the way rescheduled P3 P16 National MPs (from left): Andrew Falloon, Gerry Brownlee, party leader Todd Muller and Selwyn candidate Nicola Grigg at the announcement of the party’s com- mitment to a four-lane highway between Ashburton and Christchurch. PHOTO HEATHER MACKENZIE 080720-HM-0055 Four-lane commitment BY JAIME PITT-MACKAY a whirlwind visit through Can- tha-Southland MP Hamish four lanes of highway, it’s fantas- suring that it is all sorted so we [email protected] terbury on Wednesday, ahead Walker. tic,” he quipped. can construct it,” he said. National leader Todd Muller has of a public meeting at the Hotel After an extended period of Muller confirmed the road will “We have a fantastic track re- sent a clear message to voters Ashburton. questions about the scandal, be 60kms long, between Ash- cord with infrastructure projects ahead of the September elec- The announcement was made which has resulted in Walker burton and Christchurch, and with the roads of national signif- tion; vote me into Government, to both local and national me- announcing he won’t stand in would cost $1.5 billion. It would icance. and I will build you 60km of dia, but was somewhat over- this year’s election, Muller was also include second bridges be- four-lane highway between Ash- shadowed by the controversy looking to talk more about the ing built on the Ashburton, Sel- burton and Christchurch. -
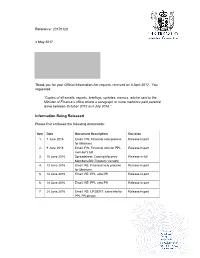
Official Information Act Response 20170123
Reference: 20170123 4 May 2017 Thank you for your Official Information Act request, received on 4 April 2017. You requested: “Copies of all emails, reports, briefings, updates, memos, advice sent to the Minister of Finance’s office where a paragraph or more mentions paid parental leave between October 2015 and July 2016.” Information Being Released Please find enclosed the following documents: Item Date Document Description Decision 1. 7 June 2016 Email: FW: Financial veto process Release in part for Ministers 2. 9 June 2016 Email: FW: Financial veto for PPL Release in part member's bill 3. 10 June 2016 Spreadsheet: Costing Moroney Release in full Members Bill (Treasury Version) 4. 13 June 2016 Email: RE: Financial veto process Release in part for Ministers 5. 14 June 2016 Email: RE: PPL veto PR Release in part 6. 14 June 2016 Email: RE: PPL veto PR Release in part 7. 28 June 2016 Email: RE: URGENT: extra info for Release in part PPL PR please I have decided to release the documents listed above, subject to information being withheld under one or more of the following sections of the Official Information Act, as applicable: • personal contact details of officials, under section 9(2)(a) – to protect the privacy of natural persons, including deceased people • direct dial phone numbers of Treasury officials, under section 9(2)k – to prevent the disclosure of official information for improper gain or improper advantage, and • names and contact details of junior officials, under section 9(2)(g)(i) – to maintain the effective conduct of public affairs through the free and frank expression of opinions. -

Tuesday, October 20, 2020 Home-Delivered $1.90, Retail $2.20 She Shed Support Sell-Out Mounts for Davis New Covid Strain As Deputy Pm Identified
TE NUPEPA O TE TAIRAWHITI TUESDAY, OCTOBER 20, 2020 HOME-DELIVERED $1.90, RETAIL $2.20 SHE SHED SUPPORT SELL-OUT MOUNTS FOR DAVIS NEW COVID STRAIN AS DEPUTY PM IDENTIFIED PAGE 2 PAGE 3 PAGE 8 LIVID LANDSCAPE: Artist John Walsh’s painting, When decisions are made from afar, is a direct response to the forestry industry’s devastating impact on the ecology of the East Coast. SEE STORY PAGE 4 Image courtesy of John Walsh and Page Galleries. Picture by Ryan McCauley Multiple injuries from unprovoked JAIL FOR attack by drunk farmer in a fury HELLBENT on attacking a fellow farmer, who socialised in the same group, was a Gisborne man drove for 40 minutes in a fit involved in a situation with a woman. of rage fuelled by vodka, prescription drugs Morrison asked directions to the man’s and cannabis, to get to him, Gisborne District house from his neighbours and told them Court was told. they would “find out later” why he wanted to David Bruce Morrison, 47, was jailed know. The neighbours phoned ahead to warn yesterday for four years and one month, and the victim Morrison, seemingly drunk, was VIOLENT, given a three-strike warning for intentionally on his way. The victim went to his gateway to causing grievous bodily harm to the victim meet him. in an unprovoked incident about 9pm on Morrison immediately launched a vicious, October 11, 2018. prolonged, assault on the man, ultimately He pleaded guilty to the charge and an rendering him unconscious. It was extreme associated one of unlawfully possessing a violence, for which the victim subsequently firearm. -

Thursday, June 3, 2021
TE NUPEPA O TE TAIRAWHITI THURSDAY, JUNE 3, 2021 HOME-DELIVERED $1.90, RETAIL $2.20 PAGE 3 INNOCENT COUNCIL VICTIMS 22 FROM ONE FAMILY TO PAY FOR KILLED ARTS & IN GAZA HEADSTONES ENTERTAINMENT BOMBINGS PAGES 23-26 PAGE 15 INSIDE TODAY Countdown blasts off Mayor Rehette Stoltz and Countdown Gisborne team member Diane Harkess cut the ribbon to officially open Countdown’s new store this morning. Watching proceedings is store manager Jess Stubbs. Mrs Harkess is the longest serving team member with Countdown Gisborne. The supermarket, built near the original Countdown, has 35 percent more space and offers more car parks, which began to be steadily filled following the official opening. Story on page 3 Pictures by Paul Rickard The purchase of TOPP1‘ is key in POWER TO enabling us to deliver on our strategy of 100 megawatts of renewable generation by 2025 — Eastland’ Group chief THE PEOPLE executive Matt Todd Kawerau power plant bought by Eastland Generation for $83m EASTLAND Group’s generation Zealand electricity market. significant developer, owner and operator supply business”. business has bought a Kawerau Eastland Generation already owns two of renewable energy in the New Zealand “It also increases our financial capacity geothermal power station from Ngati plants on the Kawerau geothermal field market. to both diversify our commercial interests Tuwharetoa Geothermal Assets (NTGA) — the 9MW Geothermal Developments “TOPP1 will provide operational and increase the level of support provided for $83 million. Ltd (GDL) and the 25MW Te Ahi O Maui synergies across our three geothermal to our owners.” Eastland Generation will take over geothermal power stations. -

2021 Opposition Team
LEADER DEPUTY LEADER Judith Collins Shane Reti Andrew Bayly David Bennett Chris Bishop Simon Bridges Gerry Brownlee Simeon Brown Jacqui Dean Papakura List MP Port Waikato List MP List MP Tauranga List MP Pakuranga Waitaki National Security & Intelligence Health Shadow Treasurer (Revenue) Agriculture Covid-19 response Justice • Water Foreign Affairs Police • Corrections Conservation Pacific Peoples • Technology, Children Infrastructure Horticulture Shadow Leader of the House Pike River Re-entry GCSB & NZSIS SFO • Youth Assistant Speaker Manufacturing & Artificial Statistics Biosecurity Māori-Crown Relations Associate Finance Intelligence Matt Doocey Paul Goldsmith Nicola Grigg Barbara Kuriger Melissa Lee Christopher Luxon Todd McClay Ian McKelvie Mark Mitchell Waimakariri List MP Selwyn Taranaki-King Country List MP Botany Rotorua Rangitīkei Whangaparaoa Chief Whip • Mental Health Education Women Energy & Resources Broadcasting & Media Local Government Economic Development Seniors • Forestry Public Service • SOEs Associate Social Associate Trade Rural Communities Digital Economy & Māori Development Small Business • Commerce Racing • Disability Issues Sports & Recreation Development & Employment Associate Arts, Food Safety Communications Associate Transport & Consumer Affairs • Tourism Associate Health Culture & Heritage Associate Transport Ethnic Communities Associate Pacific Peoples Joseph Mooney Todd Muller Simon O’Connor Chris Penk Maureen Pugh Penny Simmonds Scott Simpson Nick Smith Stuart Smith Southland Bay of Plenty Tāmaki Kaipara -

Contact Salutation/Title Job Title Electorate Party Parliament Email
Contact Salutation/Title Job Title Electorate Party Parliament Email Allan, Kiritapu Hon Member for East Coast East Coast Labour Party [email protected] Andersen, Virginia Member for Hutt South Hutt South Labour Party [email protected] Ardern, Jacinda Rt. Hon. Member for Mt Albert Mt Albert Labour Party [email protected] Baillie, Christopher List Member ACT New Zealand [email protected] Bayly, Andrew Member for Port Waikato Port Waikato National Party [email protected] Belich, Camilla List Member Labour Party [email protected] Bennett, David Hon List Member National Party [email protected] Bennett, Glen Member for New Plymouth New Plymouth Labour Party [email protected] Bishop, Christopher List Member National Party [email protected] Boyack-Mayer, Rachel Member for Nelson Nelson Labour Party [email protected] Bridges, Simon Hon Member for Tauranga Tauranga National Party [email protected] Brooking, Rachel List Member Labour Party [email protected] Brown, Simeon Member for Pakuranga Pakuranga National Party [email protected] Brownlee, Gerard Hon List Member National Party [email protected] Cameron, Mark List Member ACT New Zealand [email protected] Chen, Naisi List Member Labour Party [email protected] Chhour, Karen List Member ACT New Zealand [email protected] Clark, David Hon. Dr. Member for Dunedin Dunedin Labour Party [email protected] Coffey, Tamati List Member Labour Party [email protected] Collins, Judith Hon Member for Papakura Papakura National Party [email protected] Court, Simon List Member ACT New Zealand [email protected] Craig, Elizabeth Dr. -

Contact Salutation/Title Job Title Electorate Party Parliament Email
Contact Salutation/Title Job Title Electorate Party Parliament Email Allan, Kiritapu Hon Member for East Coast East Coast Labour Party [email protected] Andersen, Virginia Member for Hutt South Hutt South Labour Party [email protected] Ardern, Jacinda Rt. Hon. Member for Mt Albert Mt Albert Labour Party [email protected] Baillie, Christopher List Member ACT New Zealand [email protected] Bayly, Andrew Member for Port Waikato Port Waikato National Party [email protected] Belich, Camilla List Member Labour Party [email protected] Bennett, David Hon List Member National Party [email protected] Bennett, Glen Member for New Plymouth New Plymouth Labour Party [email protected] Bishop, Christopher List Member National Party [email protected] Boyack-Mayer, Rachel Member for Nelson Nelson Labour Party [email protected] Bridges, Simon Hon Member for Tauranga Tauranga National Party [email protected] Brooking, Rachel List Member Labour Party [email protected] Brown, Simeon Member for Pakuranga Pakuranga National Party [email protected] Brownlee, Gerard Hon List Member National Party [email protected] Cameron, Mark List Member ACT New Zealand [email protected] Chen, Naisi List Member Labour Party [email protected] Chhour, Karen List Member ACT New Zealand [email protected] Clark, David Hon. Dr. Member for Dunedin Dunedin Labour Party [email protected] Coffey, Tamati List Member Labour Party [email protected] Collins, Judith Hon Member for Papakura Papakura National Party [email protected] Court, Simon List Member ACT New Zealand [email protected] Craig, Elizabeth Dr. -

IPR PĀNUI the Latest from New Zealand Parliament’S Inter-Parliamentary Relations Team
APRIL 2021 IPR PĀNUI The latest from New Zealand Parliament’s Inter-Parliamentary Relations team FROM THE TEAM Welcome! Haere Mai! IN THIS EDITION... Inter-Parliamentary Organisations The New Zealand Parliament was formally opened in in the 53rd Parliament ........................ 2 November 2020, and in the last few months legislators have been busy in the Chamber and committees. Parliamentary Friendship Groups in the 53rd Parliament ............................ 4 Inter-Parliamentary activities have got off to an amazing start - we launched a new Inter- Tai a Kiwa update ................................ 5 Parliamentary Strategy, held an exhibition celebrating our Tai a Kiwa Pacific connections, and Wāhine o te Paremata Women of released a short filmWāhine o te Pāremata Women Parliament film release ...................... 6 of Parliament. Cook Islands Prime Minister meets In this edition of the pānui we introduce you to NZ MPs ................................................. 6 the new Chairpersons of our Inter-Parliamentary Our IPR portfolios ............................... 7 Organisations and Parliamentary Friendship Groups! Thank you for your support. Ngā mihi nui! The Inter-Parliamentary Relations team CONTACT Get in touch with IPR at [email protected] Follow New Zealand Parliament on social media: /NZParliament @NZParliament @NZParliament CWP New Zealand Co-Chairs, Nicola Grigg MP and Ingrid Leary MP at the International Women’s Day Celebration Breakfast. 1 INTER-PARLIAMENTARY ORGANISATIONS IN THE 53RD PARLIAMENT The New Zealand Parliament participates in the activities of three key inter-parliamentary organisations: the Inter-Parliamentary Union, the Commonwealth Parliamentary Association, and the Asia Pacific Parliamentary Forum. These are global or regional forums that bring together parliamentarians to discuss global issues, propose solutions to international devel- opments, debate world events, and promote democratic ideals and practices. -

National Party Spokesperson Allocations April 2021
National Party Spokesperson Allocations April 2021 Spokesperson for Hon Judith Collins National Security & Intelligence Leader Pacific Peoples Technology, Manufacturing & Artificial Intelligence Dr Shane Reti Health Deputy Leader Children Andrew Bayly Shadow Treasurer (Revenue) Infrastructure Statistics Hon Michael Woodhouse Finance Transport Deputy Shadow Leader of the House Hon Louise Upston Social Development & Employment Social Investment Whānau Ora Land Information Hon Todd McClay Economic Development Small Business Commerce & Consumer Affairs Tourism Associate Pacific Peoples 1 Hon Simon Bridges Justice Water Pike River Re-entry Māori-Crown Relations Chris Bishop Covid-19 Response Shadow Leader of the House Melissa Lee Broadcasting & Media Digital Economy & Communications Ethnic Communities Hon Scott Simpson Environment Workplace Relations RMA (Environment) Hon David Bennett Agriculture Horticulture Biosecurity Hon Paul Goldsmith Education Hon Mark Mitchell Public Service SOEs Sports & Recreation Barbara Kuriger Energy & Resources Rural Communities Food Safety Associate Transport 2 Hon Gerry Brownlee Foreign Affairs GCSB & NZSIS Associate Finance Nicola Willis RMA (Housing) Housing & Urban Development (including Social) Associate Economic Development Stuart Smith Climate Change Viticulture EQC Hon Jacqui Dean Conservation Assistant Speaker Todd Muller Trade & Export Growth Internal Affairs Simeon Brown Police Corrections SFO Youth Matt Doocey Chief Whip Mental Health Associate Social Development & Employment Associate Health Maureen -

Register of Pecuniary and Other Specified Interests 2021
J. 7 Register of Pecuniary and Other Specified Interests of Members of Parliament: Summary of annual returns as at 31 January 2021 Fifty-third Parliament Presented to the House of Representatives pursuant to clause 19 of Appendix B of the Standing Orders of the House of Representatives J. 7 REGISTER OF PECUNIARY AND OTHER SPECIFIED INTERESTS OF MEMBERS OF PARLIAMENT: SUMMARY OF ANNUAL RETURNS 2 REGISTER OF PECUNIARY AND OTHER SPECIFIED INTERESTS OF MEMBERS OF PARLIAMENT: SUMMARY OF J. 7 ANNUAL RETURNS MISTER SPEAKER I have the honour to provide to you, pursuant to clause 18(3) of Appendix B of the Standing Orders of the House of Representatives, a copy of the summary booklet containing a fair and accurate description of the information contained in all returns received during the period for transmitting annual returns for the Register of Pecuniary and Other Specified Interests of Members of Parliament as at 31 January 2021. Sir Maarten Wevers KNZM Registrar of Pecuniary and Other Specified Interests of Members of Parliament 3 J. 7 REGISTER OF PECUNIARY AND OTHER SPECIFIED INTERESTS OF MEMBERS OF PARLIAMENT: SUMMARY OF ANNUAL RETURNS Introduction Since 2005, members of Parliament have been required to make an annual return of their pecuniary and other specified personal interests, as set out in clauses 5 to 8 of Appendix B of the Standing Orders of the House of Representatives. The interests that are required to be registered are listed below. Items 1 to 10 provide a “snapshot” or stocktake of pecuniary and specified interests of members as at 31 January 2021. -

Changes to National Party Spokesperson Allocations: 11 November 2020
Changes to National Party Spokesperson Allocations: 11 November 2020 Rank Name Portfolios Gained Lost National Party Spokesperson Allocations 1 Hon Judith Collins • Leader of the Opposition • Pacific Peoples Steady • National Security & Intelligence • Technology, Manufacturing & Artificial Intelligence • Pacific Peoples • Technology, Manufacturing & Artificial Intelligence 2 Dr Shane Reti • Deputy Leader of the Opposition • Deputy Leader of the Opposition Up 3 spots from 5 • Health • Children • Children 3 Andrew Bayly • Shadow Treasurer (Revenue) • Shadow Treasurer (Revenue) • Revenue Up 14 spots from 17 • Infrastructure • Infrastructure • Commerce • Statistics • Statistics • State-Owned Enterprises • Associate Finance • Small Business and Manufacturing 4 Hon Michael Woodhouse • Finance • Finance • Regional Economic Development Up 8 spots from 12 • Transport • Transport • Pike River re-entry • Deputy Shadow Leader of the House 5 Hon Louise Upston • Social Development & Employment • Employment Up 4 spots from 9 • Social Investment • Whānau Ora • Whānau Ora • Land Information • Land Information 6 Hon Todd McClay • Economic Development • Small Business Steady • Small Business • Commerce & Consumer Affairs • Commerce & Consumer Affairs • Associate Pacific Peoples • Tourism • Associate Pacific Peoples 1 Rank Name Portfolios Gained Lost 7 Hon Simon Bridges • Justice • Water • Foreign Affairs Down 3 spots from 4 • Water • Pike River Re-entry • Pike River Re-entry • Māori-Crown Relations • Māori-Crown Relations 8 Chris Bishop • Covid-19 Response -

Wednesday, December 16, 2020
TE NUPEPA O TE TAIRAWHITI WEDNESDAY, DECEMBER 16, 2020 HOME-DELIVERED $1.90, RETAIL $2.20 PAGE 7 GOOD DOWN IN KAIKOURA DEEDS FOR TWO DEAD, THREE HURT PAGE 6 CHRISTMAS PAGE 3 SLIP, SLOP, SLAP AND SCAN MODERATE INJURY: The pilot of a Robinson R44 helicopter that crashed at Mahia this morning was flown to Gisborne Hospital for treatment (pictured). The chopper went down in remote, hilly terrain while carrying out agricultural work. Picture by Paul Rickard by Murray Robertson hilly terrain but we were able to Hastings Rescue Helicopter for land nearby,” a rescue chopper their efforts. A HELICOPTER pilot was spokesman said. “The Civil Aviation Authority taken to Gisborne Hospital this “The pilot had been able to get (CAA) has been made aware of morning after his machine went out of the machine on his own. the crash.” down in a remote area on the “He had sustained non-life In a statement late this north-eastern corner of Mahia threatening injuries to his back morning the CAA said it CHOPPER Peninsula. and head,” the spokesman said. appeared the helicopter may Police were advised of the “He was lucky not to have have hit a wire. crash and immediately called in been more seriously hurt, for “We are following up with ambulance and fire crews from sure.” police and the aviation operator. Mahia and Wairoa, and a rescue The injured pilot was treated at “It is too early to make any helicopter. the scene, carried on a stretcher comment on other details of the The Robinson R44 chopper to the rescue chopper and then accident as information is still PILOT went down in the Nukutaurua flown to Gisborne Hospital.