Impact Factor
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

New Species and Records of Balkan Trichoptera III
097_132_Balkan_Trichoptera_III_Olah.qxd 1/29/2015 12:22 PM Page 97 FOLIA HISTORICO-NATURALIA MUSEI MATRAENSIS 2014 38: 97–131 New species and records of Balkan Trichoptera III. JÁNOS OLÁH & TIBOR KOVÁCS ABSTRACT: We report 113 caddisfly species from Albania, Bosnia & Herzegovina, Bulgaria, Croatia, Greece, Macedonia, Montenegro, Serbia, and Slovenia. Ten new species are described: Wormaldia busa Oláh sp. n., W. daga Oláh sp. n., W. graeca Oláh sp. n., W. homora Oláh sp. n., Tinodes karpathos Oláh sp. n., Hydropsyche sarnas Oláh sp. n., Annitella jablanicensis Oláh sp. n., Allogamus zugor Oláh sp. n., Potamophylax alsos Oláh sp. n., and Beraea gurba Oláh sp. n. Two unknown females are described: Potamophylax kesken Oláh, 2012, and P. tagas Oláh et Kovács, 2012. The Potamophylax tagas species cluster is revised by fine structure analysis of the cluster divergence, including cluster history, probable speciation, divergence between sibling pairs, as well as gonopod, paramer, aedeagus, and vaginal sclerite divergences. Introduction Data and information on the Balkan Trichoptera, especially from Albania, Macedonia Monte- negro and Serbia is still very limited in spite of the very high diversity in these countries. High elevation habitats in several mountain ranges are significant endemic hotspots. Our annual field work, although very limited, is producing every year new distributional data and new species (OLÁH 2010, 2011; OLÁH & KOVÁCS 2012a,b, 2013; OLÁH et al. 2012, 2013a,b, 2014). Both spring and autumnal collecting trips were financed by The Sakertour Eastern Europe, the Birdwatching and Hide Photography Company of the Carpathian Basin and Danube Delta. We have applied the collecting, processing, clearing, cleaning and drawing methods described by OLÁH (2011). -

Pagina 1 Di 22 10/10/2014
Pagina 1 di 22 Print Bluetongue, Bulgaria Close Information received on 01/09/2014 from Pr. Nikola T. Belev, OIE Delegate, OIE Regional Representation for Eastern Europe, Ministry of Agriculture and Food , SOFIA, Bulgaria Summary Report type Follow-up report No. 3 Date of start of the event 04/07/2014 Date of pre-confirmation of the 04/07/2014 event Report date 01/09/2014 Date submitted to OIE 01/09/2014 Reason for notification Reoccurrence of a listed disease Date of previous occurrence 27/03/2008 Manifestation of disease Clinical disease Causal agent Bluetongue virus Serotype 4 Nature of diagnosis Clinical, Laboratory (basic) This event pertains to the whole country Immediate notification (15/07/2014) Follow-up report No. 1 (07/08/2014) Follow-up report No. 2 (08/08/2014) Related reports Follow-up report No. 3 (01/09/2014) Follow-up report No. 4 (08/09/2014) Follow-up report No. 5 (24/09/2014) New outbreaks (156) Outbreak 1 Zlatograd, Zlatograd, Smoljan, SMOLJAN Date of start of the outbreak 14/07/2014 Outbreak status Continuing (or date resolved not provided) Epidemiological unit Farm Species Susceptible Cases Deaths Destroyed Slaughtered Affected animals Cattle 15 4 0 0 0 Outbreak 2 Kushla, Zlatograd, Smoljan, SMOLJAN Date of start of the outbreak 14/07/2014 Outbreak status Continuing (or date resolved not provided) Epidemiological unit Farm Species Susceptible Cases Deaths Destroyed Slaughtered Affected animals Goats 93 2 0 0 0 Outbreak 3 Tsatsarovtsi, Zlatograd, Smoljan, SMOLJAN Date of start of the outbreak 14/07/2014 Outbreak -

Application of Aerospace Methods for Monitoring of Forest Fires and Evaluation of Burned Area in Haskovo Region in the Summer of 2011
Bulgarian Academy of Sciences. Space Research and Technology Institute. Aerospace Research in Bulgaria. 25, 2013, Sofia APPLICATION OF AEROSPACE METHODS FOR MONITORING OF FOREST FIRES AND EVALUATION OF BURNED AREA IN HASKOVO REGION IN THE SUMMER OF 2011 Maria Dimitrova, Iva Ivanova, Mariana Zaharinova, Roumen Nedkov Space Research and Technology Institute – Bulgarian Academy of Sciences e-mail: [email protected] Abstract The most significant forest and field fires in Haskovo region in the summer of 2011 are looked through. Information about physico-geographic characteristics of the area, land cover, etc. are gathered and analyzed in GIS. Тhe location and the area affected by the largest fire are being determined based on sattelite data. An analysis of the affected area is done. Introduction Haskovo region is situated in the East part of South Bulgaria. It has an area of 5534 km2 that is 5% of the country area. In the region there are 261 urban places, arranged in 11 municipalities - Haskovo, Dimitrovgrad, Svilengrad, Lyubimets, Harmanli, Madzharovo, Simeonovgrad, Ivaylovgrad Topolovgrad, Mineral Baths and Stambolovo. The municipality borders are: the districts of Plovdiv, Stara Zagora, Yambol, Kardzhali. In the South-East region it borders with Greece and Turkey. The region is crossed by the railway line Sofia - Istanbul and the highway “Trakia”. The territory of Haskovo region covers the southwestern ridges of the Sakar Mountain and the northern parts of the Eastern Rhodopes. Though the region flow the rivers Maritsa, Arda and Sazliyka. There are hot springs and balneological resorts in the area of Haskovski Mineral Baths and Merichleri, in Simeonovgrad and Dolno Botevo. -

Deronectes Moestus
Journal of Biogeography (J. Biogeogr.) (2016) 43, 1533–1545 ORIGINAL Reconstructing ancient Mediterranean ARTICLE crossroads in Deronectes diving beetles David Garcıa-Vazquez1, David T. Bilton2, Rocıo Alonso1, Cesar J. Benetti3, Josefina Garrido3, Luis F. Valladares4 and Ignacio Ribera1,* 1Institute of Evolutionary Biology (CSIC- ABSTRACT Universitat Pompeu Fabra), Barcelona, Spain, Aim To reconstruct the evolutionary history of a genus of freshwater beetle 2Marine Biology and Ecology Research Centre, with a pan-Mediterranean distribution, to test classic hypotheses which pro- School of Marine Science and Engineering, Plymouth University, Drake Circus, Plymouth posed a Miocene origin for groups with high biodiversity in the Iberian and PL4 8AA, UK, 3Department of Ecology and Anatolian peninsulas. Animal Biology, Faculty of Biology, University Location Mediterranean basin. of Vigo, 36310 Vigo, Spain, 4Department of Biodiversity and Environmental Management Methods We sequenced four mitochondrial and one nuclear gene from 51 (Zoology), Leon University, 24071 Leon, specimens of 30 of the c. 60 extant species of Deronectes (Dytiscidae), all typical Spain of mid-mountain streams from North Africa and Iberia over most of Europe to the Middle East. We used maximum likelihood, Bayesian probabilities with an a priori evolutionary rate and a dispersal–extinction–cladogenesis model to reconstruct their biogeographical history. Results Deronectes has two major lineages which originated in the mid Mio- cene; one including mostly eastern and another mainly western and central Mediterranean species. From these two areas, range expansions, mainly at the end of the Miocene and beginning of the Pliocene, resulted in the many species groups and some of the extant species of the genus. -

Ethnobotany / Etnobotánica
Botanical Sciences 99(2): 321-341 2021 Received: October 6, 2020, Accepted: December 16, de 2020 DOI: 10.17129/botsci.2672Ivanova et al. / BotanicalOn Sciences line first: 99(2):February 321-341. 15, 2021 2021 Ethnobotany / Etnobotánica SINGING THE NATURE - ETHNOBOTANICAL KNOWLEDGE IN BULGARIAN FOLK SONGS CANTO CON LA NATURALEZA: CONOCIMIENTO ETNOBOTÁNICO EN CANCIONES POPULARES BÚLGARAS 1 2 1 1 TEODORA IVANOVA *, VALENTINA GANEVA-RAICHEVA , YULIA BOSSEVA , AND DESSISLAVA DIMITROVA 1 Institute of Biodiversity and Ecosystem Research, Bulgarian Academy of Sciences, Acad. G. Bonchev St., Sofia, Bulgaria. 2 Institute of Ethnology and Folklore Studies with Ethnographic Museum, Bulgarian Academy of Sciences, Acad. G. Bonchev St., Sofia, Bulgaria. *Author for correspondence: [email protected] Abstract Background: Bulgarian poetic folklore reflects an agrarian culture deeply connected with land and nature. However, traditional ecological knowledge (TEK) transmitted through Bulgarian folklore is scarcely assessed. Questions: What are the dimensions of the TEK related to plant diversity (native and introduced) that appear in Bulgarian folk songs and what is their potential as transmitters of ТЕК? Data description: The lyrics of 10,113 Bulgarian folk songs were excerpted from major academic collections and a set of unpublished songs. Study site and dates: Current study covers songs that have been documented since mid-19th century onwards in the present and former Bulgar- ian territories and in areas that have been inhabited by ethnic Bulgarians abroad. Methods: Common plant names and descriptions of plants and landscapes were used to detect botanical affiliations of the denoted plants. We focused on frequencies of plant representations and their functions associated with cultural, agricultural and food-processing practices. -

Journal Club--Brucellosis Paper.Pdf
Surveillance and outbreak reports I NVEST I GAT I ON OF THE SPREAD OF BRUCELLOS I S AMONG HUMAN AND AN I MAL POPULAT I ONS I N SOUTHEASTERN B ULGAR I A , 2 0 0 7 V Tzaneva ()1, S Ivanova2, M Georgieva2, E Tasheva2 1. University Hospital, Stara Zagora, Bulgaria 2. Regional Inspectorate for Public Health Protection and Control, Haskovo, Bulgaria Three human cases of brucellosis were reported in summer 2007 countries, representing a notification rate of 0.20 per 100,000. in the region of Haskovo in southeastern Bulgaria. Subsequently, Twelve countries reported zero cases. The highest notification rates the regional veterinary and public health authorities carried out per 100,000 were reported by Greece (1.1), Italy (0.78), Portugal investigations to determine the spread of infection in domestic (0.72) and Spain (0.3) [5]. animals and in the human population. As a result, over 90,000 animals were tested, and 410 were found infected with brucellosis. In Bulgaria, since 1903, only sporadic cases had been reported The screening of 561 people believed to have been at risk of in humans. However, during the last few years, the numbers infection yielded 47 positive results. The majority of these persons increased; 37 cases were reported in 2005 and 11 in 2006 had direct contact with domestic animals or had consumed [6,7]. In 2007, in the course of the investigations described in unpasteurised dairy products. The investigations revealed evidence this paper, 50 cases were identified in the province of Haskovo in of disease among animals in the region and a considerable risk to southeastern Bulgaria (Figure 1), which brought the total number humans, thus emphasising the need for effective prevention and of cases registered in the country to 57. -
Fast Delivery
Delivery and Returns Delivery rates: We strive to offer an unbeatable service and deliver our products safely and cost-effectively. Our main focus is serving our The delivery is performed by a third-party delivery service provider. customers’ needs with a combination of great design, quality products, value for money, respect for the environment and All orders under 20 kg are shipped by courier with door-to-door delivery service. outstanding service. Please read our Delivery terms and details before you complete your order. If you have any questions, we advise that you contact us at 080019889 and speak with one of our customer service associates. All orders over 20 kg are shipped by transport company with delivery to building address service. All orders are processed within 72 hours from the day following the day on which the order is confirmed and given to the courier or transport company for delivery. After the ordered goods are given to courier or transport company for delivery, we will send you a tracking number, which will allow you to check on their website for recent status. The delivery price is not included in the price of the goods. The transport and delivery cots depend on the weight and volume of the ordered items, the delivery area and any additional services (delivery to apartment entrance, etc.). The following delivery pricelist is applied. All prices are in Bulgarian Lev (BGN) with included VAT. 1. Delivery of samples and small 3. Additional service - Delivery to packages door-to-door up to 20 kg. apartment entrance. If you need assistance by us for delivering the goods to your apartment, Kilograms Zone 1 - Zone 11 this is additionaly paid handling service, which you can request by 0 - 1 kg. -

COMMISSION IMPLEMENTING DECISION (EU) 2017/247 of 9 February 2017 on Protective Measures in Relation to Outbreaks of Highly Path
L 36/62 EN Official Journal of the European Union 11.2.2017 COMMISSION IMPLEMENTING DECISION (EU) 2017/247 of 9 February 2017 on protective measures in relation to outbreaks of highly pathogenic avian influenza in certain Member States (notified under document C(2017) 1044) (Text with EEA relevance) THE EUROPEAN COMMISSION, Having regard to the Treaty on the Functioning of the European Union, Having regard to Council Directive 89/662/EEC of 11 December 1989 concerning veterinary checks in intra- Community trade with a view to the completion of the internal market (1), and in particular Article 9(4) thereof, Having regard to Council Directive 90/425/EEC of 26 June 1990 concerning veterinary and zootechnical checks applicable in intra-Community trade in certain live animals and products with a view to the completion of the internal market (2), and in particular Article 10(4) thereof, Whereas: (1) Avian influenza is an infectious viral disease in birds. Infections with avian influenza viruses in domestic poultry and other captive birds cause two main forms of that disease that are distinguished by their virulence. The low pathogenic form generally only causes mild symptoms, while the highly pathogenic form results in very high mortality rates in most species of birds. That disease may have a severe impact on the profitability of poultry farming. (2) In the event of an outbreak of avian influenza in a Member State, there is a risk that the disease agent may spread to other holdings where poultry or other captive birds are kept. As a result, it may spread from one Member State to other Member States or to third countries through trade in live poultry or other captive birds or their products. -

Images of Horsemen in Battle on Works of Thracian Art
Mariya Avramova Images of Horsemen in Battle on Works of Thracian Art Mariya Avramova Thracians is a common name given by the Greeks to the tribes inhabiting most of the territory of modern southeastern Europe. One of the most common and important figures is the horseman who is identified with the Thracian ruler or members of the aristocracy. The present paper reviews five depictions of battle scenes from two Thracian tombs – the Alexandrovo tomb and the Kazanlak tomb, situated in modern day Bulgaria. The images, though different, have some common elements such as the depiction of horsemen and that the soldiers do not wear armor, even though they are equipped with various weapons. The wall paintings are never found within the burial chamber itself but in the rooms leading to it. This, as well as the small number of such images, may suggest that even though battle was an important rite of passage in Thracian culture, it was not the most important element. 66 Chronika Images of Horsemen in Battle on Works of Thracian Art Introduction and present a variety of themes such as scenes of investiture, hunting and, what is most This article seeks to introduce and interpret the important for the current article, battle. repertoire of currently known representations of horsemen in battle in Thracian art as Only those scenes which are undoubtedly found within modern Bulgaria. Thracians is depictions of battle where both sides of the a common name given by the Greeks to the conflict are depicted will be taken into account tribes inhabiting most of the territory of in this paper. -

Additions to the Lichenized and Lichenicolous Fungi in Bulgaria
MYCOBIOTA 10: 39–62 (2020) RESEARCH ARTICLE ISSN 1314-7129 (print) http://dx.doi.org/10.12664/mycobiota.2020.10.04doi: 10.12664/mycobiota.2020.10.04 ISSN 1314-7781 (online) www.mycobiota.com Additions to the lichenized and lichenicolous fungi in Bulgaria Helmut Mayrhofer ¹*, Adriana Atanassova ¹, Siyka O. Nikolova ² & Cvetomir M. Denchev ² ¹ Institute of Biology, Division of Plant Sciences, NAWI Graz, University of Graz, Holteigasse 6, A-8010 Graz, Austria ² Institute of Biodiversity and Ecosystem Research, Bulgarian Academy of Sciences, 2 Gagarin St., 1113 Sofi a, Bulgaria Received 28 July 2020 / Accepted 6 August 2020 / Published 7 August 2020 Mayrhofer, H., Atanassova, A., Nikolova, S.O. & Denchev, C.M. 2020. Additions to the lichenized and lichenicolous fungi in Bulgaria. – Mycobiota 10: 39–62. doi: 10.12664/mycobiota.2020.10.04 Abstract. Th irty-six taxa of lichenized fungi, Acarospora irregularis, Arthonia mediella, Caloplaca asserigena, C. atrofl ava, C. subpallida, Catillaria detractula, Diplotomma hedinii, Endohyalina insularis, Lecanora rouxii, L. rupicola subsp. subplanata, Lecidea berengeriana, L. sarcogynoides, Lepra leucosora, Lepraria borealis, L. diff usa, L. elobata, L. nylanderiana, L. vouauxii, Ochrolechia arborea, Pertusaria fl avicans, Protoparmeliopsis muralis var. dubyi, Pycnora praestabilis, Rinodina freyi, R. luridata var. immersa, R. occulta, R. roscida, R. sicula, R. teichophila, R. trevisanii, Rinodinella dubyanoides, Scoliciosporum umbrinum var. corticicolum, Solorina bispora var. macrospora, Strigula affi nis, Tephromela atra var. torulosa, Umbilicaria freyi, and U. maculata, are reported for the fi rst time from Bulgaria. Th e fi nding of Rinodina sicula represents the fi rst record for the Balkan Peninsula. Key words: biodiversity, Bulgaria, lichenicolous fungi, lichenized fungi, Rinodina, taxo nomy Introduction Th e present paper is a contribution to the lichen biota of Bulgaria and the Balkan Peninsula. -

Regional Disparities in Bulgaria Today: Economic, Social, and Demographic Challenges
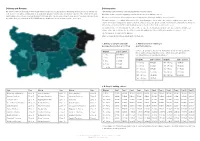
REGIONAL DISPARITIES IN BULGARIA TODAY: ECONOMIC, SOCIAL, AND DEMOGRAPHIC CHALLENGES Sylvia S. Zarkova, PhD Student1 D. A. Tsenov Academy of Economics – Svishtov, Department of Finance and Credit Abstract: To accelerate Bulgaria's economic development taking into account the specific characteristics of their regions is a serious challenge for the local governments in the country. The ongoing political and economic changes require a reassessment of the country's economic development. The aim of this study was to analyse the disparities among Bulgaria’s regions (de- fined in accordance with the Nomenclature of Territorial Units for Statistics (NUTS)) by assessing the degree of economic, social and demographic chal- lenges they face and performing a multivariate comparative analysis with sets of statistically significant indicators. The analysis clearly outlines the bounda- ries of the regional disparities and the need to improve the country’s regional and cohesion policies. Key words: regional policy, differences, NUTS, taxonomic develop- ment measure. JEL: J11, O18, R11. * * * 1 Е-mail: [email protected] The author is a member of the target group of doctoral students who participated in activities and training within the implementation of project BG05M2OP001-2.009-0026-C01 ‘Capacity development of students, PhD students, post-doctoral students and young scientists from the Dimitar A. Tsenov Academy of Economics - Svishtov for innovative scientific and practical Research in the field of economics, administration and management’ funded by the Operational Program ‘Science and Education for Smart Growth’ co-financed by the Structural and Investment Funds of the European Union. The paper won first place in the ‘Doctoral Students’ category of the national competition ‘Young Economist 2018’. -

N O CULTURAL SITE LOCATION SHORT DESCRIPTION 1 Museum
Седалище: 6300 Хасков о, у л. „Цар Осв ободител“ 4 Адрес за кореспонденция: Бизнес Инку батор, 6310 Клокотница, Община Хасков о тел: ++359 38 66 50 21; факс: ++359 38 66 48 69 e-mail: [email protected] o www.maritza.inf o N CULTURAL SITE LOCATION SHORT DESCRIPTION o The Historical Museum in Dimitrovgrad is a cultural and scientific institute established in 1951. It is the first museum in Bulgaria for contemporary history. According to its profile it is a comprehensive history museum and has the following departments: - Modern and Most Recent History Department - Ethnography Department - Arts Department - Petko Churchuliev Arts Gallery; - Affiliate - Penyo Penev House Museum - Department of Archaeology. Today it showcases artefacts from the Neolithic Age to modern times, displayed in four exhibition halls. 1 Museum of History town of Dimitrovgrad The hall entitled "Youth-brigade movement in Bulgaria" is one of a kind in Bulgaria, focusing on a complicated and controversial period of the country's recent past – the time frame 1945-1990. Brigade members' uniforms, flags, awards, photos depicting the daily life of youth brigade members, and other items reveal the history of this movement and immerse visitors in the spirit of the times. The Dimitrovgrad Hall reveals the construction of one of Bulgaria's youngest cities, which became a symbol of Socialism in the 1950s. The Archaeology Hall showcases artefacts testifying to the life in the settlements in Dimitrovgrad Municipality, some of which have had a continuous development since the Neolithic period (6th century BC) to the present day. Part of the museum's fund is known as the "Neolithic man" discovered in 2009 during archaeological rescue excavations of the medieval settlement in the Kar Dere locality near the village of Krum close to Dimitrovgrad.