Nursing Home Visitation-COVID-19
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gao-21-367, Covid-19 in Nursing
United States Government Accountability Office Report to Congressional Addressees May 2021 COVID-19 IN NURSING HOMES Most Homes Had Multiple Outbreaks and Weeks of Sustained Transmission from May 2020 through January 2021 GAO-21-367 May 2021 COVID-19 IN NURSING HOMES Most Homes Had Multiple Outbreaks and Weeks of Sustained Transmission from May 2020 through January 2021 Highlights of GAO-21-367, a report to congressional addressees Why GAO Did This Study What GAO Found The COVID-19 pandemic has had a GAO analysis of data from the Centers for Disease Control and Prevention disproportionate impact on the 1.4 (CDC) shows that, from May 2020 through January 2021, nursing homes million elderly or disabled residents in commonly experienced multiple COVID-19 outbreaks. According to CDC, an the nation’s more than 15,000 outbreak starts the week a nursing home reports a new resident or staff COVID- Medicare- and Medicaid-certified 19 case and ends when there are 2 weeks with no new cases. GAO found that nursing homes. The Centers for nursing homes had an average of about three outbreaks during the review Medicare & Medicaid Services (CMS) period, with most of the nursing homes (94 percent, or 12,555 of the 13,380 is responsible for ensuring that nursing nursing homes) experiencing more than one COVID-19 outbreak. homes nationwide meet federal quality standards. The CARES Act includes a provision directing GAO to monitor the federal pandemic response. GAO was also asked to review CMS oversight of nursing homes in light of the pandemic. This report describes the frequency and duration of COVID-19 outbreaks in nursing homes. -

2021 7 Day Working Days Calendar
2021 7 Day Working Days Calendar The Working Day Calendar is used to compute the estimated completion date of a contract. To use the calendar, find the start date of the contract, add the working days to the number of the calendar date (a number from 1 to 1000), and subtract 1, find that calculated number in the calendar and that will be the completion date of the contract Date Number of the Calendar Date Friday, January 1, 2021 133 Saturday, January 2, 2021 134 Sunday, January 3, 2021 135 Monday, January 4, 2021 136 Tuesday, January 5, 2021 137 Wednesday, January 6, 2021 138 Thursday, January 7, 2021 139 Friday, January 8, 2021 140 Saturday, January 9, 2021 141 Sunday, January 10, 2021 142 Monday, January 11, 2021 143 Tuesday, January 12, 2021 144 Wednesday, January 13, 2021 145 Thursday, January 14, 2021 146 Friday, January 15, 2021 147 Saturday, January 16, 2021 148 Sunday, January 17, 2021 149 Monday, January 18, 2021 150 Tuesday, January 19, 2021 151 Wednesday, January 20, 2021 152 Thursday, January 21, 2021 153 Friday, January 22, 2021 154 Saturday, January 23, 2021 155 Sunday, January 24, 2021 156 Monday, January 25, 2021 157 Tuesday, January 26, 2021 158 Wednesday, January 27, 2021 159 Thursday, January 28, 2021 160 Friday, January 29, 2021 161 Saturday, January 30, 2021 162 Sunday, January 31, 2021 163 Monday, February 1, 2021 164 Tuesday, February 2, 2021 165 Wednesday, February 3, 2021 166 Thursday, February 4, 2021 167 Date Number of the Calendar Date Friday, February 5, 2021 168 Saturday, February 6, 2021 169 Sunday, February -

September 17, 2020 the Honorable Ruth R. Hughs Secretary of State
GovERNoR GREG ABBOTT FILED IN E OF THE September 17, 2020 SECRETARY OF STATE IjcOCLOCK The Honorable Ruth R. Hughs Secretary of State State Capitol Room 1E.8 Austin, Texas 78701 Dear Secretary Hughs: Pursuant to his powers as Governor of the State of Texas. Greg Abbott has issued the following: Executive Order No. GA-30 relating to the continued response to the COVID-19 disaster as Texas reopens. The original exectitive order is attached to this letter of transmittal. ectfully submitted, Governor GSD/gsd Attachment Posi OFFICE Box 12428 AUSTIN, TEXAS 78711 512-463-2000 (VoICE) DIAL 74-1 FOR RELAY SERVICES 3xrruftir tiIrrr BY THE GOVERNOR OF THE STATE OF TEXAS Executive Department Austin, Texas September 17, 2020 EXECUTIVE ORDER GA3O Relating to the contütued response to the COVID-19 disaster as Texas reopens. WHEREAS, I, Greg Abbott, Governor of Texas, issued a disaster proclamation on March 13, 2020, certifying under Section 418.0 14 of the Texas Government Code that the novel coronavirus (COVID- 19) poses an imminent threat of disaster for all counties in the State of Texas; and WHEREAS, in each subsequent month effective through today, I have renewed the disaster declaration for all Texas counties; and WHEREAS, I have issued executive orders and suspensions of Texas laws in response to COVID-1 9, aimed at protecting the health and safety of Texans and ensuring an effective response to this disaster; and WHEREAS, I issued Executive Order GA-Os on March 19, 2020, mandating certain social-distancing restrictions for Texans in accordance with guidelines promulgated by President Donald J. -

Nursing Home Resident's Rights
Your Rights and Protections as a Nursing Home Resident What are my rights in a nursing home? As a nursing home resident, you have certain rights and protections under Federal and state law that help ensure you get the care and services you need. You have the right to be informed, make your own decisions, and have your personal information kept private. The nursing home must tell you about these rights and explain them in writing in a language you understand. They must also explain in writing how you should act and what you’re responsible for while you’re in the nursing home. This must be done before or at the time you’re admitted, as well as during your stay. You must acknowledge in writing that you got this information. At a minimum, Federal law specifies that nursing homes must protect and promote the following rights of each resident. You have the right to: Be Treated with Respect: You have the right to be treated with dignity and respect, as well as make your own schedule and participate in the activities you choose. You have the right to decide when you go to bed, rise in the morning, and eat your meals. Participate in Activities: You have the right to participate in an activities program designed to meet your needs and the needs of the other residents. Be Free from Discrimination: Nursing homes don’t have to accept all applicants, but they must comply with Civil Rights laws that say they can’t discriminate based on race, color, national origin, disability, age, or religion. -

Choosing Long-Term Care Insurance
MFS ADVISOR EDGESM MFS HERITAGE PLANNING® > RETIREMENT Choosing Long-Term Care Insurance mfs.com When Alzheimer’s disease, an accident, a stroke or aging leaves you incapable of performing activities on your own, long-term care — in a nursing home, your own home or another residential setting — may become an essential part of your daily life. But most health insurance programs do not Protecting your assets, freeing your family from typically cover long-term care expenses. The concern and controlling where and how you state-funded Medicaid programs, for example, receive long-term care services are all good pay for some long-term care, but only if you reasons to investigate this option. have already spent most of your savings or other assets. What does long-term care insurance cover? As baby boomers see their parents grow old While long-term care policies vary greatly with and begin to understand the costs of taking respect to premiums and benefits, most policies care of them as they age, they are seeking ways cover the cost of to cover those costs for themselves. For many, ■ nursing home care purchasing long-term care insurance is the most ■ in-home assistance with daily activities effective way to do this. ■ adult daycare and other community-based A long-term care insurance policy helps you pay programs for long-term care services in whole or in part. ■ assisted-living services, including meals, With such a policy, you pay monthly premiums, health monitoring and help with daily and in the event you need long-term care, your activities provided in a setting outside the costs are covered as specified in your policy. -

Nursing Home Compare Quality Measure Technical Specifications
Nursing Home Compare Claims- Based Quality Measure Technical Specifications Final September 2018 Prepared for: Centers for Medicare and Medicaid Services 7500 Security Blvd. Baltimore, MD 21244 Submitted by: Abt Associates 10 Fawcett Street Cambridge, MA 02138 Revision History Original Publication: April 26, 2016 Revision: September, 2018 This update contains the specifications for the Number of Hospitalizations per 1,000 Long-Stay Resident Days measure, which is claims-based and risk-adjusted. This update also revises the MDS items included in the risk-adjustment models for the short-stay, claims-based quality measures, as well as the coefficients for the models. Contents PERCENTAGE OF SHORT-STAY RESIDENTS WHO WERE RE-HOSPITALIZED AFTER A NURSING HOME ADMISSION ................................................................................................. 1 Measure Name ........................................................................................................................... 1 Purpose of Measure.................................................................................................................... 1 Measure Description and Specifications .................................................................................... 1 Risk Adjustment ........................................................................................................................ 3 Measure Calculations ................................................................................................................. 6 NUMBER OF -

What Factors Predict Falls in Older Adults Living in Nursing Homes: a Pilot Study
Journal of Functional Morphology and Kinesiology Article What Factors Predict Falls in Older Adults Living in Nursing Homes: A Pilot Study Aditi Datta 1,*, Rahul Datta 2,* and Jeananne Elkins 1 1 College of Professional Studies, Northeastern University, Boston, MA 02115, USA; [email protected] 2 Mendel University In Brno. Zemˇedˇelská 1665/1, 613 00 Brno, Czech Republic * Correspondence: [email protected] (A.D.); [email protected] (R.D.); Tel.: +1-817-733-6708 (A.D.); +420-773990283 (R.D.) Received: 23 October 2018; Accepted: 20 December 2018; Published: 25 December 2018 Abstract: Background: In community-dwelling older adults, slow gait speed is linked to falls; however, little is known about the use of gait speed to predict falls in nursing home residents. The prevalence of risk factors for falls in nursing home residents is multifactorial. Objective: The purpose of this study was to examine the relationship between falls and multiple factors such as age, sex, gait speed, mobility device, fear of falling, cognitive function, medication, and environmental causes in a nursing home setting. Material and Methods: Participants were recruited from a nursing home. Independent variables such as age, sex, gait speed for 40 feet, use of a mobility device, fear of falls, cognitive function, medication, and environmental causes of falls were measured and recorded. The dependent variable was falls. Participants were followed-up for a period of six months for falls. Falls were documented from the computerized medical records at the facility. Results: Five of the 16 participants had falls in the follow-up period. Exact logistic regression, bivariate analysis, showed no significant relationship between falls and the independent variables of age, sex, gait speed, mobility device, fear of falls, cognitive function, and medication. -

Community Nursing Home
Community Nursing Home your own resources to pay for nursing home care, which may include Medicare benefits and/or applying for Medicaid assistance if you cannot afford to pay. Talk with a VA social worker about your eligibility and to figure out a plan for paying for Community Nursing Home care services. What is a Community Nursing Find out more by visiting the Paying Home? for Long Term Care section at Community Nursing Home is a place www.va.gov/Geriatrics. where Veterans can live full time and receive skilled nursing care any time What services can I get? of day or night. Community Nursing Home care always provides: VA contracts with community nursing homes to care for Veterans. 24-hour skilled nursing care The Community Nursing Home (such as wound care or help program is offered in many with IV medication) communities so Veterans can receive Occupational and physical care near their homes and families. therapy Access to social work services Am I eligible for a Community Some Community Nursing Homes Nursing Home? also provide: Eligibility for a Community Nursing Home is based on Short term rehab services clinical need and setting Hospice and palliative care for availability. The VA will only pay the end of life for Community Nursing Home care if Special care for dementia you meet eligibility criteria involving your service-connected status, level How do I decide if it is right for of disability, and income. me? Moving into a Community Nursing If you do not meet these Home is an important decision for requirements, you will need to use you and your family. -

Calendar September 14, 2020 9:30 AM Commissioners Session
Calendar September 14, 2020 9:30 AM Commissioners Session September 17, 2020 9:30 AM Commissioners Session 10:00 AM Reconvening Of Public Hearing For Consideration Of Pither #377 Drainage Maintenance Petition (Public Participation In This Hearing Will Be Taking Place Only By Virtual Means) 1:30 PM Work Session September 21, 2020 9:30 AM Commissioners Session September 24, 2020 Canceled -NO Session September 28, 2020 9:30 AM Commissioners Session 1:30 PM View, With The Use Of Video Technology, For The Petition Requesting The Vacation Of A 0.165 Acre Tract Of Bainbridge Mills Drive In Liberty Township (Public Participation In This Viewing, Will Be Taking Place Only By Virtual Means) October 1, 2020 9:30 AM Commissioners Session 10:00 AM Reconvening Of Hearing For Consideration Of The Zerbe- O’Keefe #265 Drainage Improvement Petition October 5, 2020 9:30 AM Commissioners Session 10:00 AM Hearing For The Petition Requesting The Vacation Of A 0.165 Acre Tract Of Bainbridge Mills Drive In Liberty Township (Public Participation In This Viewing, Will Be Taking Place Only By Virtual Means) October 8, 2020 9:30 AM Commissioners Session October 12, 2020 9:30 AM Commissioners Session October 15, 2020 9:30 AM Commissioners Session October 19, 2020 9:30 AM Commissioners Session October 22, 2020 9:30 AM Commissioners Session October 22, 2020 10:00 AM Reconvene Public Hearing For Consideration Of A Petition From The Lake-Of-The-Woods Water Company Requesting Dedication Of A 3.136-Acre Segment Of Duncan’s Glen Drive As A Public Right-Of-Way October 26, -

2018 - 2019 Days of Rotation Calendar
2018 - 2019 DAYS OF ROTATION CALENDAR Day # Date Rotation Day Type Notes Day # Date Rotation Day Type Notes Saturday, October 13, 2018 Sunday, October 14, 2018 Monday, September 3, 2018 Holiday/Vaca Labor Day 27 Monday, October 15, 2018 Day 3 In Session 1 Tuesday, September 4, 2018 Day 1 In Session 28 Tuesday, October 16, 2018 Day 4 In Session 2 Wednesday, September 5, 2018 Day 2 In Session 29 Wednesday, October 17, 2018 Day 5 In Session 3 Thursday, September 6, 2018 Day 3 In Session 30 Thursday, October 18, 2018 Day 6 In Session 4 Friday, September 7, 2018 Day 4 In Session 31 Friday, October 19, 2018 Day 1 In Session Saturday, September 8, 2018 Saturday, October 20, 2018 Sunday, September 9, 2018 Sunday, October 21, 2018 Monday, September 10, 2018 Day Holiday/Vaca Rosh Hashanah 32 Monday, October 22, 2018 Day 2 In Session 5 Tuesday, September 11, 2018 Day 5 In Session 33 Tuesday, October 23, 2018 Day 3 In Session 6 Wednesday, September 12, 2018 Day 6 In Session 34 Wednesday, October 24, 2018 Day 4 In Session 7 Thursday, September 13, 2018 Day 1 In Session 35 Thursday, October 25, 2018 Day 5 In Session 8 Friday, September 14, 2018 Day 2 In Session 36 Friday, October 26, 2018 Day 6 In Session Saturday, September 15, 2018 Saturday, October 27, 2018 Sunday, September 16, 2018 Sunday, October 28, 2018 9 Monday, September 17, 2018 Day 3 In Session 37 Monday, October 29, 2018 Day 1 In Session 10 Tuesday, September 18, 2018 Day 4 In Session 38 Tuesday, October 30, 2018 Day 2 In Session Wednesday, September 19, 2018 Day Holiday/Vaca Yom Kippur 39 Wednesday, October 31, 2018 Day 3 In Session 11 Thursday, September 20, 2018 Day 5 In Session 40 Thursday, November 1, 2018 Day 4 In Session 12 Friday, September 21, 2018 Day 6 In Session 41 Friday, November 2, 2018 Day 5 In Session Saturday, September 22, 2018 Saturday, November 3, 2018 Sunday, September 23, 2018 Sunday, November 4, 2018 13 Monday, September 24, 2018 Day 1 In Session 42 Monday, November 5, 2018 Day 6 In Session 14 Tuesday, September 25, 2018 Day 2 In Session Tuesday, November 6, 2018 Prof Dev. -
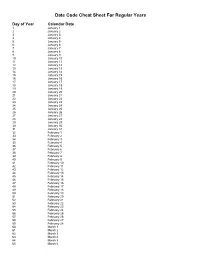
Julian Date Cheat Sheet for Regular Years
Date Code Cheat Sheet For Regular Years Day of Year Calendar Date 1 January 1 2 January 2 3 January 3 4 January 4 5 January 5 6 January 6 7 January 7 8 January 8 9 January 9 10 January 10 11 January 11 12 January 12 13 January 13 14 January 14 15 January 15 16 January 16 17 January 17 18 January 18 19 January 19 20 January 20 21 January 21 22 January 22 23 January 23 24 January 24 25 January 25 26 January 26 27 January 27 28 January 28 29 January 29 30 January 30 31 January 31 32 February 1 33 February 2 34 February 3 35 February 4 36 February 5 37 February 6 38 February 7 39 February 8 40 February 9 41 February 10 42 February 11 43 February 12 44 February 13 45 February 14 46 February 15 47 February 16 48 February 17 49 February 18 50 February 19 51 February 20 52 February 21 53 February 22 54 February 23 55 February 24 56 February 25 57 February 26 58 February 27 59 February 28 60 March 1 61 March 2 62 March 3 63 March 4 64 March 5 65 March 6 66 March 7 67 March 8 68 March 9 69 March 10 70 March 11 71 March 12 72 March 13 73 March 14 74 March 15 75 March 16 76 March 17 77 March 18 78 March 19 79 March 20 80 March 21 81 March 22 82 March 23 83 March 24 84 March 25 85 March 26 86 March 27 87 March 28 88 March 29 89 March 30 90 March 31 91 April 1 92 April 2 93 April 3 94 April 4 95 April 5 96 April 6 97 April 7 98 April 8 99 April 9 100 April 10 101 April 11 102 April 12 103 April 13 104 April 14 105 April 15 106 April 16 107 April 17 108 April 18 109 April 19 110 April 20 111 April 21 112 April 22 113 April 23 114 April 24 115 April -
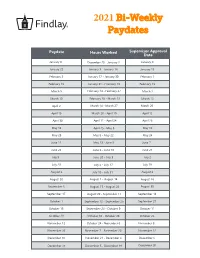
2021 Bi-Weekly Paydates
2021 Bi-Weekly Paydates Paydate Hours Worked Supervisor Approval Date January 8 December 20 - January 2 January 4 January 22 January 3 - January 16 January 15 February 5 January 17 - January 30 February 1 February 19 January 31 - February 13 February 15 March 5 February 14 - February 27 March 1 March 19 February 28 - March 13 March 15 April 2 March 14 - March 27 March 29 April 16 March 28 - April 10 April 12 April 30 April 11 - April 24 April 26 May 14 April 25 - May 8 May 10 May 28 May 9 - May 22 May 24 June 11 May 23 - June 5 June 7 June 25 June 6 - June 19 June 21 July 9 June 20 - July 3 July 2 July 23 July 4 - July 17 July 19 August 6 July 18 - July 31 August 2 August 20 August 1 - August 14 August 16 September 3 August 15 - August 28 August 30 September 17 August 29 - September 11 September 13 October 1 September 12 - September 25 September 27 October 15 September 26 - October 9 October 11 October 29 October 10 - October 23 October 25 November 12 October 24 - November 6 November 8 November 26 November 7 - November 20 November 22 December 10 November 21 - December 4 December 6 December 24 December 5 - December 18 December 20 2021 Bi-Weekly Paydate/Holiday Paydates January February March April Sun Mon Tues Wed Thurs Fri Sat Sun Mon Tues Wed Thurs Fri Sat Sun Mon Tues Wed Thurs Fri Sat Sun Mon Tues Wed Thurs Fri Sat 1 2 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 3 5 6 7 8 9 7 8 9 10 11 12 13 7 8 9 10 11 12 13 4 5 6 7 8 9 10 10 11 12 13 14 15 16 14 15 16 17 18 19 20 14 15 16 17 18 19 20 11 12 13 14 15 16 17 17 18 19 20 21 22 23 21 22 23 24 25 26