Towards the Global Elimination of Brain Damage Due to Iodine Deficiency
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SECTION 3.P65
Section III The Global Partnership People & Governments/Salt Industry UN System/AusAID/CIDA/ Kiwanis International/Global Network/ ICCIDD/IRLI/Research Centres/MI 1. Introduction 2. People in Countries where IDD is a Public Health Problem 3. Governments of Countries where IDD is a Public Health Problem 4. The Salt Industry 5. The Role of UNICEF and WHO in Eliminating Iodine Deficiency Disorders 6. Bilateral Aid (Development) Agencies 7. Kiwanis International First Worldwide Service Project 8. The Global Network for the Sustainable Elimination of Iodine Deficiency 9. The International Council for Control of Iodine Deficiency Disorders (ICCIDD) 10.The International Resource Laboratories for Iodine (IRLI) Network 11.Research Centres that have made major contributions to IDD research 12.The Micronutrient Initiative (MI) 40 Global Elimination of Brain Damage Due to Iodine Deficiency 1. Introduction Great progress has been made in the development of IDD Elimination Programs through an informal Global Partnership that has developed following the World Summit for Children in 1990. In this Section III the various partners describe their role which has led to the development of coordination and effective action towards the great goal of elimination. The partnership includes the following - 2. People in countries where IDD is a public health problem. 3. Governments of countries where IDD is a public health problem. 4. Salt Industry has an important role to play in achieving effective Salt iodization 5. The Role of the UN System particularly WHO and UNICEF, which are specifically committed to assisting countries achieve the goal of elimination of IDD. The World Bank has provided major funding support to the development of the salt industry in Indonesia and China. -

Annual Report 2008 - 2009 - 2008 Report Annual FOOD STANDARDS Australia New Zealand Annual Report 2008-2009
Annual Report 2008 - 2009 FOOD STANDARDS Australia New Zealand Annual Report 2008-2009 Australia New Zealand PO Box 7186 PO Box 10559 Canberra BC The Terrace ACT 2610 Wellington 6036 Australia New Zealand Tel: +61 2 6271 2241 Tel: +64 4 978 5630 Fax: +61 2 6271 2278 Fax: +64 4 473 9855 [email protected] [email protected] www.foodstandards.gov.au www.foodstandards.govt.nz Food Standards Australia New Zealand Food Standards FOOD STANDARDS Australia New Zealand Annual Report 2008-2009 © Food Standards Australia New Zealand 2009 ISSN 1329-3850 This work is copyright. Apart from any use as permitted under the Copyright Act 1968, no part may be reproduced by any process without prior written permission from Food Standards Australia New Zealand (FSANZ). Requests and inquiries concerning reproduction and rights should be addressed to the Information Officer, FSANZ, PO Box 7186, Canberra BC, ACT 2610. An electronic version of this work is available on the Food Standards Australia New Zealand (FSANZ) website at http:// www.foodstandards.gov.au. This electronic version may be downloaded, displayed, printed and reproduced in unaltered form only for your personal, non-commercial use or use within your organisation. Food Standards Australia New Zealand Australia New Zealand PO Box 7186 PO Box 10559 Canberra BC The Terrace ACT 2610 Wellington 6036 Australia New Zealand Tel: 61 2 6271 2241 Tel: 64 4 473 9942 Fax: 61 2 6271 2278 Fax: 64 4 473 9855 [email protected] [email protected] ANNUAL REPORT 2008-2009 Letter of Transmittal The Hon Mark Butler, MP Parliamentary Secretary for Health Parliament House Canberra ACT 2600 Annual Report of Food Standards Australia New Zealand for the year ended 30 June 2009 I am pleased to present to you the Annual Report of Food Standards Australia New Zealand. -

SOLHE020 Pearls (Bla
SOLHE020 Pearls (Blackmores) Zipper CS5.indd 1 CS5.indd Zipper (Blackmores) Pearls SOLHE020 3/06/10 5:43 PM 5:43 3/06/10 Acknowledgement This issue of clinical Masterclass has been GPs. for only is competition This 2010. 31, August entry for date closing — www.healthed.com.au at conditions and terms full read LTPS/10/04667 number lottery *NSW made possible thanks to an unrestricted educational grant from Blackmores Phone 1300 797 794 Fax 1300 797 792 Email [email protected] Mail GPO BOX 500 Burwood 1805 FOLD FOLD FOLD s s This package contains one Audio CD and one DVD Find out why Iodine supplements are now regarded as essential for these women. these for essential as regarded now are supplements Iodine why out Find or considering pregnancy take an iodine supplement of 150mcg per day. day. per 150mcg of supplement iodine an take pregnancy considering or NHMRC recommends that all Australian women who are pregnant, breastfeeding breastfeeding pregnant, are who women Australian all that recommends NHMRC Synopsis: Synopsis: Iodine deficiency is widespread and increasing. As of March 2010 the the 2010 March of As increasing. and widespread is deficiency Iodine Coffee Machine Coffee $900 Gaggia Gaggia $900 a for go into the draw draw the into go and and CPD the the Complete Complete Medical & Adviser, Australian Thyroid Foundation Thyroid Australian Adviser, & Medical Endocrinologist, Eastman, Creswell Prof Why, How Much, When? When? Much, How Why, Duration 25 min 25 Duration Iodine Supplementation in Pregnancy Pregnancy in Supplementation Iodine Burwood NSW 1805 NSW Burwood AUSTRALIA NSW lottery number LTPS/10/04667* PO BOX 500 BOX PO PAID PAID Masterclass Clinical Vol 20 Vol POSTAGE POSTAGE FOLD FOLD FOLD s s About the Speaker Your Learning Options, Claiming CPD Online PROF CRESWELL J. -

The Iodine Deficiency Disorders
THE IODINE DEFICIENCY DISORDERS Creswell J. Eastman MD, Professor of Medicine, Sydney Medical School, the University of Sydney; Principal, The Sydney Thyroid Clinic; Consultant Emeritus Westmead Hospital, Sydney. PO Box 478, St Leonards, Sydney NSW 2065 Australia. Email: [email protected] Michael B. Zimmermann MD, Professor of Human Nutrition, Swiss Federal Institute of Technology (ETH) Zurich, LFVD20, Schmelzbergstrasse 7, CH-8092 Zurich, Switzerland Email: [email protected] Revised 6 25 17 ABSTRACT This chapter provides an overview of the disorders caused by iodine deficiency. Extensively referenced, it includes data on dietary sources of iodine, goitrogens, the effects of iodine deficiency throughout the lifecycle, the pathophysiology of iodine deficiency, as well as strategies for control and monitoring of the iodine deficiency disorders, such as iodized salt and iodized oil. It emphasizes the role of iodine deficiency in the development of brain damage and neurocognitive impairment, assessment of the iodine status of a population, the potential side effects of excessive iodine intake and current worldwide epidemiological data. INTRODUCTION This chapter provides a global overview of the disorders caused by iodine deficiency. Special emphasis will be put on recent developments such as the role of iodine deficiency in the development of brain damage and neurocognitive impairment, assessment of the iodine status of a population, strategies for control and monitoring of the iodine deficiency disorders (IDD), as well as side effects of iodine. Up to date information on IDD can be obtained by visiting the website of the Iodine Global Network (IGN) http://www.ign.org. ETIOLOGY Iodine (atomic weight 126.9 g/atom) is an essential component of the hormones produced by the thyroid gland. -

Final Assessment Report Proposal P230
12 February 2008 [1-08] FINAL ASSESSMENT REPORT PROPOSAL P230 CONSIDERATION OF MANDATORY FORTIFICATION WITH IODINE FOR NEW ZEALAND For Information on matters relating to this Report or the assessment process generally, please refer to http://www.foodstandards.gov.au/standardsdevelopment/ Executive Summary This Final Assessment Report considers mandatory fortification with iodine as a means of addressing the re-emergence of iodine deficiency in New Zealand. Iodine deficiency such, as that reported in New Zealand, has can have a negative impact on mental and nervous system development in children, and increases the risk of some forms of hyperthyroidism, especially in the elderly. In May 2004, the Australia and New Zealand Food Regulation Ministerial Council (Ministerial Council) requested that Food Standards Australia New Zealand (FSANZ) give priority consideration to mandatory fortification with iodine. In response, FSANZ prepared this Proposal (Proposal P230). In October 2005, the Ministerial Council noted the advice of the Australian Health Ministers’ Advisory Council and Australian Health Ministers’ Conference that mandatory fortification with iodine is an effective public health strategy subject to clinical safety and cost- effectiveness. FSANZ was asked to progress consideration of mandatory fortification with iodine as a matter of priority and on this basis has expedited this process. In September 2007, FSANZ was advised that Australian Health Ministers were re-evaluating the evidence on the prevalence and severity of iodine deficiency in Australia, and that FSANZ should defer its consideration of mandatory iodine fortification for Australia until further advice is received. In addition Health Ministers noted that the situation in New Zealand presents a significant health problem, and that mandatory fortification with iodine is considered the most effective strategy to address it. -

The Parliament of the Commonwealth of Australia Australian Government
The Parliament of the Commonwealth of Australia Australian Government Publishing Service Canberra © Commonwealth of Australia 1993 ISBN 0644 32757 2 This work is copyright. Apart from any use as permitted under the Copyright Act 1968, no part may be reproduced by any process without prior written permission from the Australian Government Publishing Service. Requests and inquiries concerning reproduction and rights should be addressed to the Manager, Commonwealth Information Services, Australian Government Publishing Service, GPO Box 84, Canberra ACT 2601. Printed in Australia by A. J. LAW, Commonwealth Government Printer, Canberra VI vii ABBREVIATIONS viii x 1 INTRODUCTION 1 CONDUCT OF THE INQUIRY . 1 PRELIMINARY OBSERVATIONS 2 AID BUDGET 6 The nature of aid 6 History of the official aid program 7 Recent influences on the health component of the aid budget 8 Health aid to Papua New Guinea 10 International influences on the health aid budget 10 Other influences on the health aid budget 11 WHAT IS HEALTH AID? 12 Primary Health Care 12 Too narrow a definition of health aid? 13 THE SIZE OF THE HEALTH AID BUDGET 16 The total aid budget 16 The health component of the aid budget 17 in THE ROLE OF THE DEPARTMENT OF HEALTH, HOUSING, LOCAL GOVERNMENT & COMMUNITY SERVICES Memoranda of Understanding The Public Health Education and Research Program Special "international" PHERP funding THE ROLE OF THE DEPARTMENT OF FOREIGN AFFAIRS AND TRADE 30 Direct Aid Program 30 DFAT liaison with AIDAB 30 DFAT liaison with DHHLGCS 31 THE ROLE OF NON GOVERNMENT ORGANISATIONS 33 The advantages and disadvantages of using NGOs to deliver aid 34 COUNTRY STRATEGIES AND PROGRAMS 37 HEALTH SECTOR COORDINATION WITHIN AIDAB 38 The Health and Population Section 38 The Coordinating Group on Health . -

Problems of Interfering Substances Identified
[Reprinted from CLINICAL CHEMISTRY, 36, 865 (1990).] ' Copyright 1990 by the American Association of Clinical Chemistry and reprinted by permission of the copyright owner. Evaluation of Automated Urinary lodine Methods: Problems of Interfering Substances Identified Warwick May,' Diana Wu,' Creswell Eastman,' Pierre Bourdoux,^ and Glen Maberly' We evaluated automated methods for measurement of uri biochemical déterminations have advanced rapidly. nary iodine (Ul) over a range expected in iodinereplete and Our aim w£is to evaluate the performance of the auto iodinedeficient populations. Results obtained with Tectini mated Ul System available since 1973, which is based on con AutoAnalyzer II Systems, based on either dialysis or acid dialysis of urine (method A). Results from samples assayed digestion, were compared witfi those obtained by a manual at Westmead Hospital, Australia, were correlated with alkaline ashing techinique. Results of automated dialysis results fi^m the Saint Pierre University Hospital, Bel were consistently higher than those obtained by the other gium, which were obtained with an even earlier automated methods. The apparently higher concentrations of Ul we Ul détermination, based on acid digestion (method B). measured were due to interfering substances crossing the Results from thèse automated methods were also compared with results obtained by a more technically demanding dialysis membrane and participating in the catalytic reaction. manual technique (method G, performed at Westmead Thiocyanate (SCN) was one endogenous substance contrib Hospital), based on the oSicial method of the Association of uting to the increased measurement of Ul. For urinary SCN OflRcial Analytical Chemists (AOAC) (6), in which alkaline concentrations of 5 to 15 mg/L, the amount of overestimation ashing is used to destroy organic matter in the sample in the Ul measurement attributable to SCN ranged from 21.8 before the final colorimetric measurement of iodine. -

Sunpab Health
Sunpab Health Professional Catalogue QUALITY. TRUSTED. INNOVATIVE. Sunpab Health Contents Page 1. About Sunpab 3 2. Our Products 2.1 Pain Eze 6 2.2 Mum-2-B 32 2.3 Sugar Balance 51 2.4 EyeMax 65 2.5 Hair Skin Nails 80 2.6 CardiOz 85 2.7 Student’s Memory Power 100 2.9 Baby Smart 105 Disclaimer: The information in this document is presented by Sunpab Health Products for the purpose of dissemi- nating health information free of charge to Health Professionals and is not intended for public use. While we have exercised due care in ensuring the accuracy of the material contained in this document, the information is made available on the basis that Sunpab is not providing professional advice on a particular matter. This information is not a substitute for independent professional advice. Nothing contained in this is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used as a substitute for health professional's advice. Sunpab Health Products does not accept any liability for any injury, loss or damage incurred by use of or reliance on the information provided in this booklet. 2 Sunpab Health About Sunpab • Australian made and Australian owned • Backed by a team of Pharmacists, Naturopaths, Nutritionists and Medical Scientists • Manufacturers of quality, evidence based, natural health products • Internationally renowned company • The manufacturer of scientifically validated products • Approved by the regulatory authority of Australia (TGA) • Ingredients have been scientifically validated as well as used traditionally for centuries in different parts of the world Our activities: Sunpab Health Pty Ltd employs staff from a diverse range of backgrounds, majority are health professionals. -
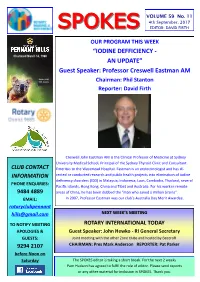
Spokesspokes Editor: David Firth
VOLUME 59 No. 11 4th September, 2017 SPOKESSPOKES EDITOR: DAVID FIRTH OUR PROGRAM THIS WEEK “IODINE DEFFICIENCY - Chartered March 14, 1960 AN UPDATE” Guest Speaker: Professor Creswell Eastman AM District 9685 NSW, Australia Chairman: Phil Stanton Reporter: David Firth Creswell John Eastman AM is the Clinical Professor of Medicine at Sydney University Medical School, Principal of the Sydney Thyroid Clinic and Consultant CLUB CONTACT Emeritus to the Westmead Hospital. Eastman is an endocrinologist and has di- INFORMATION rected or conducted research and public health projects into elimination of iodine deficiency disorders (IDD) in Malaysia, Indonesia, Laos, Cambodia, Thailand, several PHONE ENQUIRIES: Pacific Islands, Hong Kong, China and Tibet and Australia. For his work in remote 9484 4889 areas of China, he has been dubbed the "man who saved a million brains". EMAIL: In 2007, Professor Eastman was our club’s Australia Day Merit Awardee. rotaryclubpennant [email protected] NEXT WEEK’S MEETING TO NOTIFY MEETING ROTARY INTERNATIONAL TODAY APOLOGIES & Guest Speaker: John Hewko - RI General Secretary GUESTS: Joint meeting with the other Zone clubs and hosted by Beecroft 9294 2107 CHAIRMAN: Pres Mark Anderson REPORTER: Pat Parker before Noon on Saturday The SPOKES editor is taking a short break. For the next 2 weeks Pam Hudson has agreed to fulfil the role of editor. Please send reports or any other material for inclusion in SPOKES. Thank you. Rotary Meeting – Monday 28th August, 2017 Once upon a time, on a Monday that seems so far ago, a bunch of old fogies got together on a Monday night. They called it Rotary, and they had a guest speaker.