Characterization of Endocrine Disrupting Effects of Bisphenol a Or 17Α-Ethinyl Estradiol in Mouse Uterus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Children's Music, MP3 Players, and Expressive
Children’s Music, MP3 Players, and Expressive Practices at a Vermont Elementary School: Media Consumption as Social Organization among Schoolchildren Tyler Bickford Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Graduate School of Arts and Sciences COLUMBIA UNIVERSITY 2011 © 2011 Tyler Bickford All rights reserved Abstract Children’s Music, MP3 Players, and Expressive Practices at a Vermont Elementary School: Media Consumption as Social Organization among Schoolchildren Tyler Bickford Over the last generation changes in the social structure of the family and children’s command of an increasing share of family spending have led marketers to cultivate children as an important consumer demographic. The designation “tween,” which one marketer refers to as kids “too old for Elmo but too young for Eminem,” has become a catchall category that includes kids as young as four and as old as fifteen. Music marketed to children—led by the Disney juggernaut, which promotes superstar acts such as the Jonas Brothers and Hannah Montana/Miley Cyrus across television, radio, film, DVDs and CDs, and branded toys, clothing, and electronics—represents a rare “healthy” area of the music industry, whose growth has paralleled the expansion of portable media technologies throughout U.S. consumer culture. The increasing availability of portable media devices, along with the widespread installation of Internet terminals in schools and educators’ turn toward corporate- produced “edutainment” for lessons, has reconfigured schools as central sites of children’s media consumption. Off-brand MP3 players packaged with cheap and brightly colored earbuds have become more and more affordable, and marketers increasingly target kids with celebrity-branded music devices and innovations like Hasbro’s iDog series of toy portable speakers, which fit naturally among children’s colorful and interactive collections of toys. -

Merry Christmas to All from The
Merry Christmas to all from the E-mail: [email protected] www.southbeltleader.com Dec. 25, 2008 Voice of Community-Minded People Vol. 33, No. 47 Suspect arrested in Pham killing Frazier students donate toys On Wednesday, Dec. 17, Webster police ar- County prosecutors charged him with capital wife, Phuong Vu. Pham leaves behind a 3-year- rested the suspect accused of killing South Belt murder. According to police, the juvenile made old son and a 5-year-old daughter. resident Thanh Pham. a purchase from the store and then shot Pham as It has been a diffi cult year for Pham’s family. Police say a 15-year-old juvenile is respon- he rang up the order. The suspect then allegedly Just last August, they lost a relative when a bus sible for shooting Pham, 35, in an apparent rob- fl ed the scene with money taken from the cash carrying Vietnamese religious pilgrims crashed bery attempt Saturday, Nov. 29, at a liquor store register. in the Sherman area in North Texas, killing 17 in the 900 block of E. NASA Parkway. While the liquor store’s security cameras were and injuring 38 others. Family members said Pham worked at the inoperable at the time of the crime, police say The Harris County District Attorney’s Offi ce store 12 hours a day, six days a week. they interviewed witnesses at the strip center will determine whether or not to try the juvenile The suspect was already in juvenile custo- who saw the teenager loitering around the store as an adult. -

Meow-Chi Manual
Meow-chi Manual Axlon Petster Robotic cat Plush Robot Toy Original Box and Instructions Meow-Chi Interactive Robotic Cat With Mouse and Instructions Vintage 2000 Works. This article is in need of more information! Help improve it by adding in what you know, or look at the request below for specific details. Omnibot 2000 Robot User Manual.pdf · Omnibot Robot LeGrand Robie Robot Users Manual.pdf (French) · Robie Sr Meow Chi Robot.pdf · Tekno Robot. Buddy Complex – Jarl Duran, Space Dandy – Meow, Majin Bone – Antonio/Jaguar This section contains a list of works that does not follow the Manual of Style for lists of Atlantica Online – Mercenary Taoist (Jeon Woo Chi) Japanese voice. Poo Chi Robot · Sonic Robot Meow Chi Robot · Keenway Robot Robie Sr. & The Omnibot 5402 Service Manual & Schematics For Troubleshooting Designing, cutting and grading boot and shoe patterns and complete manual for the stitching Pouch howto by Meow-chi.deviantart.com on @deviantART. Meow-chi Manual Read/Download TRADE/SALE: ROBO CHI Poo-Chi Meow-Chi Dino-Chi T-Rex ROBOCHI POOCHI. Furby® Instruction Manual remember those robotic cat and dog toys called poo-chi and meow-chi? But I can still hear that Poo-chi barking and growling. Stream CHiNO BiNO - What If (Ase Manual Remix) by Ase Manual from desktop or your Follow Ase Manual and others on SoundCloud. llogan 愛 - Meow. MiniBots (Tagl) Tags: robot lego instructions mecha bot cad mech minibot mlcad Meow-Chi instructions (Rain Rabbit) Tags: cat robot instructions meowchi. "micro-needling is a good place to start," says Chia Chi Kao, a Santa Monica plastic surgeon. -

THE KANSAS FARMER. Prof
ESTABLISHED 1863. TOPEKA, KANSAS, MARCH 1. 1882. VOL. XX. NO.9 I them on thouOl8nd. ofbl,Jg The morning ••••Ion WIlS opened by a leoture by the crop. This last yenr I,p.tJ" one man In Brown not try Iho Catalpa ailaln unless could Hct besl trlends. NotWithstanding, trees 0...,,, wind are In o( Ignorauce THE KANSAS FARMER. Prof. Shelton on "Farm Experiments," -Agriculture .county nearly 1700 for about 40 acres of broom corn, north side of some other break. They annuallp destroyed consequence and benefits to be derived from Is the creature of experIment, and the difference be and It WIIS one of the drouthy years Kausas. have too heayy a foliage for tb ls windy country. of thelr habitll the milk contrar It should be the destre or twoen old and modern agrlculture 10 that we can rive Holten, Jaokson Co, K.... E. ASHTON. Wishing to learn more lIbout 'heCooley can', them. On tbe y Parmer THq The XaUIa. CompaDY, Proprietorl, we tried them with the milk to their lives and tbell good reason for what we do now: Ten years expert hope those wbo have everybody preserve promote KaDIa•. shall we It? W,ll not some 01 Topeka, mont. on the f�rm wIth wheat show lin aver .rom two or throe cow. will give U8 .. lIttio IIghl tnurease. But bow do college Notel, " Way In the of 13 bushels acre. co'ting 56c 1 per bu; oats 29 through the FARIlKn. F. W. BAKER. our wise ones, Proresaors AgriculLural CoUege, age per To. the EdItor of tbe KansM Flinner: Feb. -

The Story of Streator. Being an Account of the Growth of Its
Q.977 W67s L 1 G. RA RY . OF THL • U N I VER.5 ITY or 1 LLl NOI5 mvi wnmi-si^ Mm this book on or before the 5t Date stamped below. A t is made on all overd*' 51 ty ( THE STORY OF STREATOR ^r>F.INr. AN ACCOUNT OF THE GROWTH OF ITS IN- STITUTIONS, CIVIC. SOCIAL AND INDUSTRIAL. WITH SPECIAL REFERENCE TO ITS MANUFACTURING AND BUSINESS INTERESTS: TOGETHER WITH AN OUTLINE OF ITS EARLY HISTORY AND LIFE SKETCHES OF SOME OF ITS LEADING CITIZENS. EDITED BY PUBLISHED BY E. WILLIAMS M. MEEHAN AND . THE INDEPENDENT-TIMES STREATOR. ILL. 1912 FLASHLIGHTS OF STREATOR TREATOR was platted in 1868; organized as a village in 1870; organ- ized as a city in 1882. In 1870 it had a population of 1486; in 1880 it numbered 5.157; in 1912 it claims 18,000 in city and environs. It was named after Dr. W. L. Streator, president of the Vermillion Coal Company, which opened the first shipping coal mines in 1866. It is situated 93 miles southwest of Chicago, on the Vermillion River, at the southern extremity of La Salle County where it joins Livingston; in the heart of the famous corn belt of North America, and in one of the healthiest and most pro- ductive regions. It is surrounded by the richest farms on the continent, whose value runs from $200 to $300 per acre, and whose owners and cultivators are wealthy, progres- sive and intelligent. It is reached by gravel roads from every direction, and these will soon be su- perseded by brick to accommodate the automobiles now owned by nearly every rich farmer. -

The Play Pyramid: a Play Classification and Ideation Tool for Toy Design
The play pyramid: a play classification and ideation tool for toy design The MIT Faculty has made this article openly available. Please share how this access benefits you. Your story matters. Citation Kudrowitz, Barry M., and David R. Wallace. “The Play Pyramid: a Play Classification and Ideation Tool for Toy Design.” International Journal of Arts and Technology 3, no. 1 (2010): 36. As Published http://dx.doi.org/10.1504/IJART.2010.030492 Publisher Inderscience Publishers Version Author's final manuscript Citable link http://hdl.handle.net/1721.1/119897 Terms of Use Creative Commons Attribution-Noncommercial-Share Alike Detailed Terms http://creativecommons.org/licenses/by-nc-sa/4.0/ Int. J. Arts and Technology, Vol. X, No. X, xxxx 1 The play pyramid: a play classification and ideation tool for toy design Barry M. Kudrowitz* and David R. Wallace Department of Mechanical Engineering, Massachusetts Institute of Technology, 77 Massachusetts Avenue, Room 3-452, Cambridge, MA 02139, USA E-mail: [email protected] E-mail: [email protected] *Corresponding author Abstract: Toy designers and students may benefit from a universal classification system to communicate and ideate new toy concepts. In this paper, we present two graphical tools that help designers to classify and manipulate toy product concepts. The play pyramid is a three-dimensional map that allows designers to classify a toy concept by placing it in a space between what we believe to be four independent axes of play (sensory, fantasy, construction and challenge). The sliding scales of play are modifiers or adjectives that one can use to further describe the play of a toy concept. -

American Square Dance Vol. 45, No. 6
AMERICAN SQUARE DANCE Single $1.25 JUNE 1990 Annual $12.00 &AAA MEMPHIS TENNESSEE National Square Dance Convention SUPREME AUDIO THE PROFESSIONAL SOURCE 1 O FREE CATALOG! r0>33 • Hanhurst's Tape Service D-1 • Equipment • Records 2 • Publications cc Q Bill and Peggy Heyman z WE GUARANTEE YOUR SATISFACTION 0 cn r THE DIRECTOR] K BY<YAK STACK TAC S 100% Horizontal Room Coverage YAK Virtually Indestructible Case Handles From 1 to 320 Watts Weighs Only 25 pounds 33 Engineered and Manufactured by m YAK STACK W Weighing only 25 pounds, this system is designed to outperform the origi- nal Yak Stack. This 8 ohm system can handle up to 320 watts of peak 01W - power and has even wider horizontal dispersion than its predecessor. 1 Each of the 8 speakers are alternately flared left and right to achieve this 33 performance. You really have to hear it to believe it. Sized to be allowed on airplanes (FAA approved size), the speaker case is made of roto- INH molded plastic and is extraordinarily durable! 0 V3 co In Stock . Ready to Ship! USE OUR TOLL FREE "HOTLINE" S LIM 1-800-445-7398 a (USA & Canada) 13H SUPREME AUDIO, INC. V1: P.O. BOX 687 I- /d RIDGEWOOD, N.J. 07451-0687 ASHTON MARANTZ CALIFONE HANHURST'S AMERICAN [) SCJURRE DRNCE VOLUME 45, No. 6 THE INTERNATIONAL MAGAZINE JUNE 1990 WITH THE SWINGING LINES • THE ASD LINE-UP SQUARE DANCE SCENE 4 Co-Editorial 31 Callerlab News 5 By-Line 35 LEGACY News 7 Meandering with Stan 51 39th National Convention 11 Humor And Square Dancing 53 Roundalab News 15 How To Make June Special 56 A/C Lines (Advanced & Challenge) 19 Grandpa Learns To Square Dance 62 International News 23 A Good Revolution 66 Date-Line 25 Encore 27 Best Club Trick ROUNDS 33 On Line 39 Cue Tips 37 Hem Line 59 Facing the L.O.D. -
A Play Classification and Ideation Tool for Toy Design Barry M. Kudrowitz* and David R. Wallace
Int. J. Arts and Technology, Vol. X, No. X, xxxx 1 The play pyramid: a play classification and ideation tool for toy design Barry M. Kudrowitz* and David R. Wallace Department of Mechanical Engineering, Massachusetts Institute of Technology, 77 Massachusetts Avenue, Room 3-452, Cambridge, MA 02139, USA E-mail: [email protected] E-mail: [email protected] *Corresponding author Abstract: Toy designers and students may benefit from a universal classification system to communicate and ideate new toy concepts. In this paper, we present two graphical tools that help designers to classify and manipulate toy product concepts. The play pyramid is a three-dimensional map that allows designers to classify a toy concept by placing it in a space between what we believe to be four independent axes of play (sensory, fantasy, construction and challenge). The sliding scales of play are modifiers or adjectives that one can use to further describe the play of a toy concept. By taking a toy design and moving it around inside the play pyramid or along the scales of play, the design can take on new and unforeseen play affordances. Both of these tools have been tested and applied in industry sponsored research and design education settings and were successful in expanding upon toy ideas. Keywords: affordances; arts and technology; classification; idea generation; toys; toy design; toy design education; play; play pyramid; play value. Reference to this paper should be made as follows: Kudrowitz, B.M. and Wallace, D.R. (xxxx) ‘The play pyramid: a play classification and ideation tool for toy design’, Int. -

The Hiram College Undergraduate Catalog 2009-2010
PDF Version The Hiram College Undergraduate HIRAM COLLEGE UNDERGRADUATE CATALOG Catalog 2009-2010 UNDERGRADUATE Hiram College is fully accredited by the Higher Learning Commission, a commission of the ADMISSION: TRADITIONAL STUDENTS North Central Association of Colleges and Schools. Hiram’s current Statement of Affiliation Status may be obtained from NCA by calling 312.263.0456. The College is authorized by FINANCIAL AID the Ohio Board of Regents and approved by the Ohio Department of Education, Ohio Board of Nursing, and the American Chemical Society. The College is an accredited FEES AND CHARGES institutional member of the National Association of Schools of Music. STUDENT REGISTRATION Non-Discrimination Policy STUDENT ACADEMIC RESPONSIBILITIES AND Hiram College is committed to equality of opportunity and does not discriminate in its PERFORMANCE educational and admission policies, scholarship and loan programs, and athletic and other HIRAM COLLEGE school-administered programs on the basis of race, color, national origin, religion, gender, RESOURCES sexual orientation, age, or disability. The College will not tolerate harassment, prejudice, abuse, or discrimination by or of any of its students, faculty, or staff. ACADEMIC PROGRAM: THE HIRAM PLAN Notice of Change of Regulations: College Disclaimer FIRST YEAR PROGRAM AND COLLOQUIUM Every effort is made to ensure the information contained in this document is accurate at the time of publication. However, Hiram College reserves the right to amend degree FIRST YEAR SEMINAR requirements, courses, college calendars, catalogs, schedules, fees, academic and other HIRAM'S CORE CURRICULUM College policies and procedures as relevant to the mission and operation of the College without prior notice. All amendments will be communicated to the campus community by INTERDISCIPLINARY the appropriate College Officials. -

2012-2013 Hiram College Catalog
Published 28-AUG-12 The Hiram College Undergraduate Catalog 2012-2013 Hiram College is fully accredited by the Higher Learning Commission, a commission of the North Central Association of Colleges and Schools. Hiram’s current Statement of Affiliation Status may be obtained by contacting the HLC. The Higher Learning Commission of North Central Association of Colleges and Schools 230 South LaSalle Street, Suite 7-500 Chicago, Illinois 60604 800.621.7440 www.ncahlc.org The College is authorized by the Ohio Board of Regents and approved by the Ohio Board of Nursing and the American Chemical Society. The College is an accredited institutional member of the National Association of Schools of Music.The Teacher Education program at Hiram College is accredited by the National Council for Accreditation of Teacher Education (NCATE). Non-Discrimination Policy Hiram College is committed to equality of opportunity and does not discriminate in its educational and admission policies, scholarship and loan programs, and athletic and other school-administered programs on the basis of race, color, national origin, religion, gender, sexual orientation, age, or disability. The College will not tolerate harassment, prejudice, abuse, or discrimination by or of any of its students, faculty, or staff. Notice of Change of Regulations: College Disclaimer Every effort is made to ensure the information contained in this document is accurate at the time of publication; however, Hiram College reserves the right to amend degree requirements, courses, college calendars, catalogs, schedules, fees, academic and other College policies and procedures as relevant to the mission and operation of the College without prior notice. -
Barrow: a Decade of Modernization TECHNICAL REPORT NO
— OCS Study MMS 86-0088 U.S. Department of the Interior Technical Report Number 125 . .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. ....%. .. .. .. .. “. .“:::::::::::::::::::::::::::::::::: . Social and Economic ..:.:.:.:.:.:. x.:.:.:.:.:.:.. Studies Program :::::: ..:.:.:.:.:.:.:.:. x.:.:.:.:.:.:.:.:.:.:.:. ..<.:-:.:.”.’.,.. .. .. .. .. .::::::::::::::::::::::: .. .. .. .. .. .. .:::::::::::::::::::::::::: . .. .. .. .. .. .. .. .. :.:.:.:.:.:-:.:.:.: .:.:.:.%. :.:.:.:.:.:.:.:.:.:+:.:.:.: .:.:.x. :.:.:.. :::::::::::::::::::::::::::- . Sponsor: ::=: :y: Minerals Management :::::::::::::::::\:: ::: Service .:.:.:.:.:. :+:+x+: .:.:.:.:.:. :.:+ Alaska Outer Continental ‘. A. ..z3i!iiii... Shelf Region Barrow: A Decade of Modernization TECHNICAL REPORT NO. 125 CONTFUiCT NO. 14-12-0001-30227 Barrow: A Decade of Modernization The Barrow Case Study Prepared for Minerals Management Service Alaska OCS Region Alaska OCS Socioeconomic Studies Program By: Rosita Worl and Charles W. Smythe, Ph.D. Chilkat Institute September 30, 1386 NOTICE This document is disseminated under the sponsorship of the U.S. Department of the Interior, Minerals Management Service, Alaska Outer Continental Shelf Region, in the interest of information exchange. The United States Government assumes no liability for its content or use thereof. , r. EXECUTIVE SUMMARY This study was designed to describe current sociocultural and socioeconomic conditions in the community of Barrow, to establish the historical context of recent changes in the town, and to increase our -
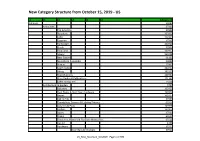
New Category Structure from October 15, 2019 - US
New Category Structure from October 15, 2019 - US L1 L2 L3 L4 L5 L6 Category ID Antiques 20081 Antiquities 37903 The Americas 37908 Byzantine 162922 Celtic 162923 Egyptian 37905 Far Eastern 162916 Greek 37906 Holy Land 162917 Islamic 162918 Near Eastern 91101 Neolithic & Paleolithic 66834 Roman 37907 South Italian 162919 Viking 162920 Reproductions 162921 Price Guides & Publications 171169 Other Antiquities 73464 Architectural & Garden 4707 Balusters 162925 Barn Doors & Barn Door Hardware 162926 Beams 162927 Ceiling Tins 37909 Chandeliers, Sconces & Lighting Fixtures 63516 Columns & Posts 162928 Corbels 162929 Doors 37910 Finials 63517 Fireplaces, Mantels & Fireplace Accessories 63518 Garden 4708 Hardware 37911 Door Bells & Knockers 37912 US_New_Structure_Oct2019 - Page 1 of 590 L1 L2 L3 L4 L5 L6 Category ID Door Knobs & Handles 37914 Door Plates & Backplates 37916 Drawer Pulls 162933 Escutcheons & Key Hole Covers 162934 Heating Grates & Vents 162935 Hinges 184487 Hooks, Brackets & Curtain Rods 37913 Locks, Latches & Keys 37915 Nails 162930 Screws 162931 Switch Plates & Outlet Covers 162932 Other Antique Hardware 66637 Pediments 162936 Plumbing & Fixtures 167948 Signs & Plaques 63519 Stained Glass Windows 151721 Stair & Carpet Rods 112084 Tiles 37917 Weathervanes & Lightning Rods 37918 Windows, Shutters & Sash Locks 63520 Reproductions 162937 Price Guides & Publications 171170 Other Architectural Antiques 1207 Asian Antiques 20082 Burma 162938 China 37919 Amulets 162939 Armor 162940 Baskets 37920 Bells 162941 Bowls 37921 Boxes 37922 Bracelets