Functionality of Ceonc Sites in Two Districts and Selected Birthing Centres in Three Districts
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nepal Human Rights Year Book 2021 (ENGLISH EDITION) (This Report Covers the Period - January to December 2020)
Nepal Human Rights Year Book 2021 (ENGLISH EDITION) (This Report Covers the Period - January to December 2020) Editor-In-Chief Shree Ram Bajagain Editor Aarya Adhikari Editorial Team Govinda Prasad Tripathee Ramesh Prasad Timalsina Data Analyst Anuj KC Cover/Graphic Designer Gita Mali For Human Rights and Social Justice Informal Sector Service Centre (INSEC) Nagarjun Municipality-10, Syuchatar, Kathmandu POBox : 2726, Kathmandu, Nepal Tel: +977-1-5218770 Fax:+977-1-5218251 E-mail: [email protected] Website: www.insec.org.np; www.inseconline.org All materials published in this book may be used with due acknowledgement. First Edition 1000 Copies February 19, 2021 © Informal Sector Service Centre (INSEC) ISBN: 978-9937-9239-5-8 Printed at Dream Graphic Press Kathmandu Contents Acknowledgement Acronyms and Abbreviations Foreword CHAPTERS Chapter 1 Situation of Human Rights in 2020: Overall Assessment Accountability Towards Commitment 1 Review of the Social and Political Issues Raised in the Last 29 Years of Nepal Human Rights Year Book 25 Chapter 2 State and Human Rights Chapter 2.1 Judiciary 37 Chapter 2.2 Executive 47 Chapter 2.3 Legislature 57 Chapter 3 Study Report 3.1 Status of Implementation of the Labor Act at Tea Gardens of Province 1 69 3.2 Witchcraft, an Evil Practice: Continuation of Violence against Women 73 3.3 Natural Disasters in Sindhupalchok and Their Effects on Economic and Social Rights 78 3.4 Problems and Challenges of Sugarcane Farmers 82 3.5 Child Marriage and Violations of Child Rights in Karnali Province 88 36 Socio-economic -

Nepal Electricity Authority
NEPAL ELECTRICITY AUTHORITY ENVIRONMENTAL AND SOCIALMANAGEMENT PLAN OF SUPPLY AND INSTALLATION OF DISTRIBUTION PROJECTS (33KV TRANSMISSION LINE) UNDER THE GRID SOLAR AND ENERGY EFFICIECY PROJECT VOLUME II Prepared and Submitted by: Environment and Social Studies Department Kharipati, Bhaktapur Phone No.: 01-6611580, Fax: 01-6611590 Email: [email protected] September, 2018 SIDP Abbreviations and Acronyms ABBREVIATIONS AND ACRONYMS BS : Bikram Sambat (Nepali Era) DADO : District Agriculture Development Office DCC : District Coordination Committee DFO : District Forest Office DoED : Department of Electricity Development ESMF : Environment and Social Management Framework ESMP : Environment and Social Management Plan EPR : Environment Protection Rules, 1997 ESSD : Environment and Social Studies Department GoN : Government of Nepal GSEEP : Grid Tied and Solar Energy Efficiency Project GRC : Grievance Redress Cell GRM : Grievance Redress Mechanism HHs : Households IEE : Initial Environmental Examination MoEWRI : Ministry of Energy, Water Resource and Irrigation MoFE : Ministry of Forest and Environment NEA : Nepal Electricity Authority PAS : Project Affected Settlement PMO : Project Management Office SIDP : Supply and Installation of Distribution Project WB : World Bank Units ha : Hectare km : Kilometer kV : Kilo Volt m2 : Square meter ESMP Report i NEA-ESSD SIDP Table of Contents Table of Contents ABBREVIATIONS AND ACRONYMS ........................................................................................ I 1 INTRODUCTION ............................................................................................................ -

List of Annex
List of Annex Annex 1.1 List of Officers and Stakeholders Met (1st Stage) Annex 1.2 Field Trip Report Annex 1.3 Key Literatures and Reports Reviewed Annex 1.4 List of Officers and Stakeholders Met (2nd Stage) Annex 1.5 Questionnaire for Household Survey Annex 1.6 Traders Survey Questionnaire Annex 1.7 Report of Workshops Annex 2.1 Organization Chart of MOAC Annex 2.2 Major Functions /Roles of Different Organizational Unit of DOA Annex 2.3 Import of Selected Agricultural and Related Commodities from India and Countries other than India Annex 2.4 Export of Selected Agricultural and Related Commodities to India and Countries other than India Annex 2.5 Agriculture Markets Network in Nepal Annex 2.6 Map of Nepal Showing Agriculture Markets Network in Nepal Annex 2.7 Organization Chart of MoLD Annex 3.1 Map of Nepal Showing Survey Districts Annex 3.2 Map of Kavrepalanchok District Showing the Proposed VDCs for Survey Annex 3.3 Map of Sindhuli District Showing the Proposed VDCs for Survey Annex 3.4 Map of Mahottari District Showing the Proposed VDCs for Survey Annex 3.5 Map of Ramechhap District Showing the Proposed VDCs for Survey Annex 3.6 Map of Dolakha District Showing the Proposed VDCs for Survey Annex 3.7 Summary of Periodic District Development Plans Annex 3.8 Organizational Structure of DDC Annex 3.9 Organizational Structure of District Technical Office Annex 3.10 Key Agriculture Sector INGOs /NGOs /COs Working in the Survey Districts Annex 3.11 Annual Programs and Projects Implemented by DADO in FY 2008/09 Annex 3.12 Proportions of Cropped Area under Different Crops, 2007/08 Annex 3.13 Lists of VDCs by Potentiality Commodities Annex 5.1 Profile of Selected Markets Annex 1.1 Annex 1.1 List of Officers & Stakeholders Met (1st Stage) Date Name Organization Designation Venue Mar. -

MISP) of Reproductive Health Services for Internally Displaced Persons in Kathmandu and Sindhupalchowk Districts, Nepal
Women’s Refugee Commission Research. Rethink. Resolve. Evaluation of the Minimum Initial Services Package (MISP) of Reproductive Health Services for Internally Displaced Persons in Kathmandu and Sindhupalchowk Districts, Nepal Literature Review Focus Group Discussions Key Informant Interviews Health Facility Assessments May 2016 Research. Rethink. Resolve. The Women’s Refugee Commission improves the lives and protects the rights of women, children, and youth displaced by conflict and crisis. We research their needs, identify solutions, and advocate for programs and policies to strengthen their resilience and drive change in humanitarian practice. Acknowledgments This evaluation could not have been undertaken without the support of the Family Health Division (FHD), Department of Health Services (DoHS) Nepal the United Nations Population Fund Nepal (UNFPA), International Planned Parenthood Foun- dation (IPPF), and the Family Planning Association of Nepal (FPAN). We greatly appreciate the time taken by Dr. Shilu Aryal, FHD and Dr. Shilu Adhikari UNFPA in particular for supporting the Internal Review Board submission to the Nepal Research Council; hosting the Nepal RH sub-cluster MISP evaluation debriefing and support throughout the evaluation. We also deeply appreciate the time of Mr. Hari Kari UNFPA for scheduling and accompanying the evaluation team on key informant interviews; Dr. Nirmal Rimal, UNFPA for scheduling health facility assessments, and the overall support of UNFPA Country Director, Ms. Giulia Vallese. We also thank the IPPF for supporting administration and logistics for the evaluation including Ms. Nimisha Goswami and Mr. Rajrattan Lokhande, and at FPAN Mr. Subhash Shreshtha and Mr. Prabin Khadka. Thanks to Research Input and Development Action (RIDA) for conducting the focus group discussions; and FPAN for coordinating, scheduling, logistics, and overseeing recruitment of participants. -

Food Insecurity and Undernutrition in Nepal
SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics Acknowledgements The completion of both this and the earlier feasibility report follows extensive consultation with the National Planning Commission, Central Bureau of Statistics (CBS), World Food Programme (WFP), UNICEF, World Bank, and New ERA, together with members of the Statistics and Evidence for Policy, Planning and Results (SEPPR) working group from the International Development Partners Group (IDPG) and made up of people from Asian Development Bank (ADB), Department for International Development (DFID), United Nations Development Programme (UNDP), UNICEF and United States Agency for International Development (USAID), WFP, and the World Bank. WFP, UNICEF and the World Bank commissioned this research. The statistical analysis has been undertaken by Professor Stephen Haslett, Systemetrics Research Associates and Institute of Fundamental Sciences, Massey University, New Zealand and Associate Prof Geoffrey Jones, Dr. Maris Isidro and Alison Sefton of the Institute of Fundamental Sciences - Statistics, Massey University, New Zealand. We gratefully acknowledge the considerable assistance provided at all stages by the Central Bureau of Statistics. Special thanks to Bikash Bista, Rudra Suwal, Dilli Raj Joshi, Devendra Karanjit, Bed Dhakal, Lok Khatri and Pushpa Raj Paudel. See Appendix E for the full list of people consulted. First published: December 2014 Design and processed by: Print Communication, 4241355 ISBN: 978-9937-3000-976 Suggested citation: Haslett, S., Jones, G., Isidro, M., and Sefton, A. (2014) Small Area Estimation of Food Insecurity and Undernutrition in Nepal, Central Bureau of Statistics, National Planning Commissions Secretariat, World Food Programme, UNICEF and World Bank, Kathmandu, Nepal, December 2014. -
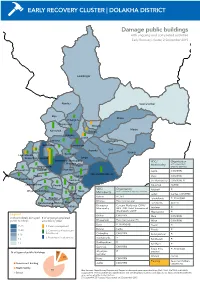
Early Recovery Cluster | Dolakha District
EARLY RECOVERY CLUSTER | DOLAKHA DISTRICT Damage public buildings with ongoing and completed activities Early Recovery cluster, 2 September 2015 Lamabagar Alambu Gaurishankar Bigu Khare Chilangkha Khopachagu Worang Marbu Kalinchok Bulung Babare Laduk Lapilang Changkhu Sundrawati Lamidanda Jhyanku Suri Syama Boch Sunkhani Lakuridanda Suspa Kshyamawati Jungu Bhimeswor Municipality VDC/ Organisation Chhetrapa Municipality with completed/ Magapauwa Kabre ongoing activities Bhusaphedi Katakuti Namdru Japhe CWV/RRN JIRI MUNICIPALITY Phasku Mirge Jhule CWV/RRN Dodhapokhari Gairimudi Jiri Municipality CWV/RRN, PI Bhirkot Sailungeshwar Pawati Kalinchok ACTED VDC/ Organisation Katakuti PI Ghyangsukathokar Jhule Hawa Municipality with completed/ongoing activities Japhe Laduk Caritas, CWV/RRN Babare ACTED Bhedpu Chyama Lakuridanda PI, RI/ANSAB Bhedpu Plan International Dandakharka Melung Malu Lamidanda ACTED Shahare Bhimeswor Concern Worldwide (CWV)/ Municipality RRN. IOM, Relief International Lapilang PI (RI)/ANSAB, UNDP Magapauwa PI Legend Bhirkot CWV/RRN Malu CWV/RRN # of completely damaged # of ongoing/completed public buildings activities by pillar Bhusaphedi Plan International (PI) Mirge CWV/RRN Boch PI, RI/ANSAB 21-28 1. Debris management Pawati PI Bulung Carita 11-20 2. Community infrastructure Phasku PI & livelihood 6-10 Chilangkha CWV/RRN Sailungeshwar PI 3. Restoration local services 3-5 Dandakharka PI Sundrawati PI Dodhapokhari PI 4% 1-2 Sunkhani PI Gairimudi CWV/RRN 12% Suspa Kshy- PI, RI/ANSAB Ghyangsu- PI amawati % of type of public buildngs 7% kathokar 14% Worang Caritas Hawa CWV/RRN Government building Planning Save the Children, Japhe CWV/RRN Government building Health facility UNDP/UNV Health facility School 79% Map Sources: Nepal Survey Department, Report on damaged government buildings, DoE, MoH, MoFALD and MoUD, 84% School August 2015. -

Time for a True Population Census: the Case of the Miscounted Thangmi Mark Turin
Time for a true population census: The case of the miscounted Thangmi Mark Turin To cite this version: Mark Turin. Time for a true population census: The case of the miscounted Thangmi. Nagarik (Citizen), 2000, 4 (2), pp.14-19. 10.17613/45tm-2914. halshs-03083395 HAL Id: halshs-03083395 https://halshs.archives-ouvertes.fr/halshs-03083395 Submitted on 27 Jan 2021 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. ‘imfl’i” (CITIZEN) Voi.I4No.4 Aug.OO-Qct.OO 0 g,q/* (CITIZEN) VoLII,Na4 Aug.OO-OcI.OO C in fact nearly double the official the months of Kartik and one another. The number of Time for a True Population Census: figure. Phagun 2054, by Mr. Meghraj Thangmi houses in each village. Simi Rishmi Thami. editor and and the breakdown of men. The Case of the Miscounted Thangmi Disparity in Figures publisher of Dolakhareng women and children, is - Mark Turin According to the 1991 (pages 38-44). (See Fig.l) common knowledge to all who (Mark Turin is a linguistic the Thangmi (Nep. Thami) workers involved in the census, the total Thangmi live n the area. -

Thangmi Time for a True Population Census: the Case of the Miscounted
‘imfl’i” (CITIZEN) Voi.I4No.4 Aug.OO-Qct.OO 0 g,q/* (CITIZEN) VoLII,Na4 Aug.OO-OcI.OO C in fact nearly double the official the months of Kartik and one another. The number of Time for a True Population Census: figure. Phagun 2054, by Mr. Meghraj Thangmi houses in each village. Simi Rishmi Thami. editor and and the breakdown of men. The Case of the Miscounted Thangmi Disparity in Figures publisher of Dolakhareng women and children, is - Mark Turin According to the 1991 (pages 38-44). (See Fig.l) common knowledge to all who (Mark Turin is a linguistic the Thangmi (Nep. Thami) workers involved in the census, the total Thangmi live n the area. According to the anthropologist and has been population of Nepal and of demanding process of statistical population is 19.103 (1999, As can be seen from the above figures then, there are working on the Thangmi Northeast India I would support recording. Having said this, the page 52) and there are 14.440 above figures. there is a great almost three times more language since 1996. He was these criticisms. disparity between the total people who spoke Thangmi as disparity between the official Thangmi people living the trained in Social Thangmi population a mother tongue (1999, page statistics and those provided by eastern districts of Nepal than Anthropology at the figure provided by the 22). Ofequal interest, however. thej ournal Dolakhareng. Some the official census suggests. University of government and the is the official breakdown of the of this difference may ofcourse Cambridge, UK, and more realistic figures Thangmi population by district. -

WASH Cluster Nepal 4W - May 12Th 2015
WASH Cluster Nepal 4W - May 12th 2015 Please find following the analysis of the 4W data – May 12th Introduction (Round 2) This is the second round of the 4W analysis. As this is the second round and still early in the emergency response, many agencies are still planning their interventions and caseloads, hence much of the data is understandably incomplete. In the coming week/s we will receive far more comprehensive partner data and will be able to show realistic gaps. In addition, we are receiving better affected population data and there are many ongoing assessments, the results of which will help us to understand both the response data and the affected population data and enable us to deliver a far more profound analysis of the WASH response. Please assist us as we have a lot of information gaps in the data provided so far and hence the maps are not yet providing a true picture of the response. We would like to quickly move to VDC mapping including planned/reached beneficiaries. Since the first round of reporting, agencies have provided substantially more VDC‐level data – as of today, of 740 WASH activities identified, 546 of these (74%) are matched to an identified VDC ‐ this is a big improvement from last week (which had VDC data for 192 of 445 activities, or 43%) The Highlights ・ 47 Organisations – number of organisations that reported in Round 1 and/or Round 2 of the WASH 4W ・ 206 VDCs – where WASH interventions taking place/planned (in 15 districts) 4W – WASH May 12th 2015 Water0B Spread of water activities ‐ targeted Temporary -

Gaurishankar Conservation Area - a Prime Habitat for Red Panda (Ailurus Fulgens) in Central Nepal
The Initiation Gaurishankar Conservation Area - A Prime Habitat for Red Panda (Ailurus fulgens) in Central Nepal Arjun Thapa1 Sunil Thapa1 and Shambu Poudel2 Corresponding email: [email protected] Abstract: Globally threatened Red Panda is found in isolated high mountain’s bamboo- forest patches in Nepal, India, Bhutan, China and Burma. This study was focused in Gaurishankar Conservation Area, one of the newly declared protected areas of Nepal, with aim to glean baseline information regarding existence of Red Panda, its habitat status and conservation issues. Methods like altitudinal line intercept, key informant survey and consultation (with local people, herders, conservation stakeholder) were used to address the objectives. Marbu, Kalinchok, Gaurishankar (Dolkha District), Chuchure, Gumdel (Ramechhap District) and Fulpingkatti (Sindupalchok District) area were surveyed in first phase of study and presence of Red Panda distribution was recorded from Marbu, Kalinchok, Chuchure and Fulpingkatti forests areas through sign evidence (fecal pellets). A total of 24 transects were established randomly in the whole area and only 16 transects were worked effectively because of topographical barrier. Distribution of Red Panda was found as clumped pattern ( ). Among these sites, frequent sign encounter was recorded in Marbu (5.45/km) area followed by Fulpingkatti (5.06/km), Kalinchok (3.73/km) and Chuchre (1.67/km). Like in other areas, conservation issues like habitat destruction, livestock pressure, fire wood collection and illegal poaching were rampant in Gaurishankar also. This study recommended for detail survey on population status and conservation activities should be elaborated in current identified habitat as well as further survey should be focused on other possible habitats within conservation area. -
TSLC PMT Result
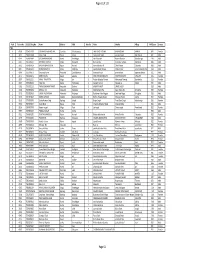
Page 62 of 132 Rank Token No SLC/SEE Reg No Name District Palika WardNo Father Mother Village PMTScore Gender TSLC 1 42060 7574O15075 SOBHA BOHARA BOHARA Darchula Rithachaupata 3 HARI SINGH BOHARA BIMA BOHARA AMKUR 890.1 Female 2 39231 7569013048 Sanju Singh Bajura Gotree 9 Gyanendra Singh Jansara Singh Manikanda 902.7 Male 3 40574 7559004049 LOGAJAN BHANDARI Humla ShreeNagar 1 Hari Bhandari Amani Bhandari Bhandari gau 907 Male 4 40374 6560016016 DHANRAJ TAMATA Mugu Dhainakot 8 Bali Tamata Puni kala Tamata Dalitbada 908.2 Male 5 36515 7569004014 BHUVAN BAHADUR BK Bajura Martadi 3 Karna bahadur bk Dhauli lawar Chaurata 908.5 Male 6 43877 6960005019 NANDA SINGH B K Mugu Kotdanda 9 Jaya bahadur tiruwa Muga tiruwa Luee kotdanda mugu 910.4 Male 7 40945 7535076072 Saroj raut kurmi Rautahat GarudaBairiya 7 biswanath raut pramila devi pipariya dostiya 911.3 Male 8 42712 7569023079 NISHA BUDHa Bajura Sappata 6 GAN BAHADUR BUDHA AABHARI BUDHA CHUDARI 911.4 Female 9 35970 7260012119 RAMU TAMATATA Mugu Seri 5 Padam Bahadur Tamata Manamata Tamata Bamkanda 912.6 Female 10 36673 7375025003 Akbar Od Baitadi Pancheswor 3 Ganesh ram od Kalawati od Kalauti 915.4 Male 11 40529 7335011133 PRAMOD KUMAR PANDIT Rautahat Dharhari 5 MISHRI PANDIT URMILA DEVI 915.8 Male 12 42683 7525055002 BIMALA RAI Nuwakot Madanpur 4 Man Bahadur Rai Gauri Maya Rai Ghodghad 915.9 Female 13 42758 7525055016 SABIN AALE MAGAR Nuwakot Madanpur 4 Raj Kumar Aale Magqar Devi Aale Magar Ghodghad 915.9 Male 14 42459 7217094014 SOBHA DHAKAL Dolakha GhangSukathokar 2 Bishnu Prasad Dhakal -
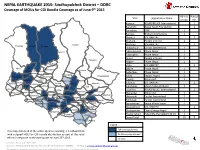
NEPAL EARTHQUAKE 2015: Sindhupalchok District – DDRC Coverage of Mous for CGI Bundle Coverage As of June 9Th 2015
NEPAL EARTHQUAKE 2015: Sindhupalchok District – DDRC Coverage of MOUs for CGI Bundle Coverage as of June 9th 2015 All HHs Partial VDC Organization Name of VDC HH Atarpur ASSAB/RELIEF International 1 Baramchi Nepal Youth Foundation 1 Barhabise IOM 1 Baruwa Global Communities 1 Bhimtar UN-HABITAT 1 Bhotang People in Need 1 Gumba Bhotsipa UN-HABITAT 1 Helambu Baruwa Bhotang Duwachaur Caritas Switzerland 1 Golche Fulpingdanda Phase Nepal 1 Fulpingkot Phase Nepal 1 Gunsa People in Need 1 Tatopani Hagam Phase Nepal 1 Thapalkot Irkhu UN-HABITAT 1 Ichok Kiul Ghunsakot Jalbire Phase Nepal 1 Ghuyang (Thanpalchap) Listokot Banskharka Kadambas Phase Nepal 1 Pangtang Palchok Mahangkal Bhotenamlang Phulpingkatti Kalika Impact Nepal 1 Kiwool Action Aid 1 Dubachaur Lagarche Baramchae Dhuyang Talamarang Kubinde UN-HABITAT 1 Thakani Jyamire Selang Hagam Marming Melamchi Sinpal Kavre Gati Kunchowk Micah Network Nepal 1 Sindhukot Syaule Jalbire Haibung ShikharpurNawalpur Batase Lisankhu ASSAB/RELIEF International 1 Bansbari Maneswar Barhabise Karthali Bhotechaur Phulpingkot Mahankal Action Aid 1 Bandegaun KunchokPipaldanda Ramche Ghorthali ChautaraKubhinde Mangkha Melamchi Caritas Switzerland 1 PhataksilaSipapokharae Gunsakun Sanusirubari Phulchodanda Tekanpur Chokati Palchowk Caritas Switzerland 1 Irkhu Pangretar BhimtarBhotsipa Piskar Sanosirubari Peace Winds Japan 1 Kadambas Thumpakhar Thulo Sirubari Pedku Yamuna Danda Tauthali Sipapokhare UN-HABITAT 1 SunkhaniThulo Pakhar Thulopakhar Clean Energy Nepal 1 Sangachok Kalika Jethal Thokarpa Attarpur Thulosirubari Help-hilfe the Selbsthilfe CV 1 Grand Total 19 8 Lisangkhu Thulo Dhading Legend Full coverage planned This map details all of the active agencies working in Sindhupalchok with a signed MOU for CGI bundle distribution as part of the relief Partial coverage planned th efforts in response to the earthquake on April 25 2015.