Refinement of Evolutionary Medicine Predictions Based on Clinical
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thiadiazole Derivatives As Anticancer Agents
Pharmacological Reports (2020) 72:1079–1100 https://doi.org/10.1007/s43440-020-00154-7 REVIEW Thiadiazole derivatives as anticancer agents Monika Szeliga1 Received: 15 June 2020 / Revised: 13 August 2020 / Accepted: 20 August 2020 / Published online: 3 September 2020 © The Author(s) 2020 Abstract In spite of substantial progress made toward understanding cancer pathogenesis, this disease remains one of the leading causes of mortality. Thus, there is an urgent need to develop novel, more efective anticancer therapeutics. Thiadiazole ring is a versatile scafold widely studied in medicinal chemistry. Mesoionic character of this ring allows thiadiazole-containing compounds to cross cellular membrane and interact strongly with biological targets. Consequently, these compounds exert a broad spectrum of biological activities. This review presents the current state of knowledge on thiadiazole derivatives that demonstrate in vitro and/or in vivo efcacy across the cancer models with an emphasis on targets of action. The infuence of the substituent on the compounds’ activity is depicted. Furthermore, the results from clinical trials assessing thiadiazole- containing drugs in cancer patients are summarized. Keywords Thiadiazole derivatives · Cancer · Anticancer therapy · Clinical trials Introduction antiparasitic, anti-infammatory and anticancer activities [2]. Due to the mesoionic nature, thiadiazoles are able to According to the most recent data provided by the Interna- cross the cellular membranes. Their relatively good lipo- tional Agency for Research on Cancer (IARC), 18.1 mil- solubility is most likely attributed to the presence of the sul- lion new cases and 9.6 million cancer deaths were regis- phur atom [3]. The thiadiazole-containing drugs, including tered worldwide in 2018 [1]. -
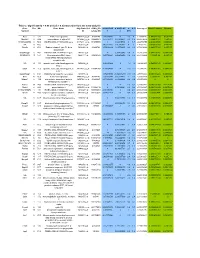
Table 2. Significant
Table 2. Significant (Q < 0.05 and |d | > 0.5) transcripts from the meta-analysis Gene Chr Mb Gene Name Affy ProbeSet cDNA_IDs d HAP/LAP d HAP/LAP d d IS Average d Ztest P values Q-value Symbol ID (study #5) 1 2 STS B2m 2 122 beta-2 microglobulin 1452428_a_at AI848245 1.75334941 4 3.2 4 3.2316485 1.07398E-09 5.69E-08 Man2b1 8 84.4 mannosidase 2, alpha B1 1416340_a_at H4049B01 3.75722111 3.87309653 2.1 1.6 2.84852656 5.32443E-07 1.58E-05 1110032A03Rik 9 50.9 RIKEN cDNA 1110032A03 gene 1417211_a_at H4035E05 4 1.66015788 4 1.7 2.82772795 2.94266E-05 0.000527 NA 9 48.5 --- 1456111_at 3.43701477 1.85785922 4 2 2.8237185 9.97969E-08 3.48E-06 Scn4b 9 45.3 Sodium channel, type IV, beta 1434008_at AI844796 3.79536664 1.63774235 3.3 2.3 2.75319499 1.48057E-08 6.21E-07 polypeptide Gadd45gip1 8 84.1 RIKEN cDNA 2310040G17 gene 1417619_at 4 3.38875643 1.4 2 2.69163229 8.84279E-06 0.0001904 BC056474 15 12.1 Mus musculus cDNA clone 1424117_at H3030A06 3.95752801 2.42838452 1.9 2.2 2.62132809 1.3344E-08 5.66E-07 MGC:67360 IMAGE:6823629, complete cds NA 4 153 guanine nucleotide binding protein, 1454696_at -3.46081884 -4 -1.3 -1.6 -2.6026947 8.58458E-05 0.0012617 beta 1 Gnb1 4 153 guanine nucleotide binding protein, 1417432_a_at H3094D02 -3.13334396 -4 -1.6 -1.7 -2.5946297 1.04542E-05 0.0002202 beta 1 Gadd45gip1 8 84.1 RAD23a homolog (S. -

Inherited Neuropathies
407 Inherited Neuropathies Vera Fridman, MD1 M. M. Reilly, MD, FRCP, FRCPI2 1 Department of Neurology, Neuromuscular Diagnostic Center, Address for correspondence Vera Fridman, MD, Neuromuscular Massachusetts General Hospital, Boston, Massachusetts Diagnostic Center, Massachusetts General Hospital, Boston, 2 MRC Centre for Neuromuscular Diseases, UCL Institute of Neurology Massachusetts, 165 Cambridge St. Boston, MA 02114 and The National Hospital for Neurology and Neurosurgery, Queen (e-mail: [email protected]). Square, London, United Kingdom Semin Neurol 2015;35:407–423. Abstract Hereditary neuropathies (HNs) are among the most common inherited neurologic Keywords disorders and are diverse both clinically and genetically. Recent genetic advances have ► hereditary contributed to a rapid expansion of identifiable causes of HN and have broadened the neuropathy phenotypic spectrum associated with many of the causative mutations. The underlying ► Charcot-Marie-Tooth molecular pathways of disease have also been better delineated, leading to the promise disease for potential treatments. This chapter reviews the clinical and biological aspects of the ► hereditary sensory common causes of HN and addresses the challenges of approaching the diagnostic and motor workup of these conditions in a rapidly evolving genetic landscape. neuropathy ► hereditary sensory and autonomic neuropathy Hereditary neuropathies (HN) are among the most common Select forms of HN also involve cranial nerves and respiratory inherited neurologic diseases, with a prevalence of 1 in 2,500 function. Nevertheless, in the majority of patients with HN individuals.1,2 They encompass a clinically heterogeneous set there is no shortening of life expectancy. of disorders and vary greatly in severity, spanning a spectrum Historically, hereditary neuropathies have been classified from mildly symptomatic forms to those resulting in severe based on the primary site of nerve pathology (myelin vs. -

Anticancer Effects of NSC‑631570 (Ukrain) in Head and Neck Cancer Cells: in Vitro Analysis of Growth, Invasion, Angiogenesis and Gene Expression
282 ONCOLOGY REPORTS 43: 282-295, 2020 Anticancer effects of NSC‑631570 (Ukrain) in head and neck cancer cells: In vitro analysis of growth, invasion, angiogenesis and gene expression RUTH HERRMANN1, JOSEPH SKAF2, JEANETTE ROLLER1, CHRISTINE POLEDNIK1, ULRIKE HOLZGRABE2 and MARIANNE SCHMIDT1 1Department of Otorhinolaryngology, University of Würzburg, D-97080 Würzburg; 2Institute of Pharmacy and Food Chemistry, University of Würzburg, D-97074 Würzburg, Germany Received September 17, 2018; Accepted September 30, 2019 DOI: 10.3892/or.2019.7416 Abstract. NSC-631570 (Ukrain) is an aqueous extract of laminin). Microarray analysis revealed the downregulation of Chelidonium majus, a herbaceous perennial plant, one of two genes encoding key regulators, including EGFR, AKT2, JAK1, species in the genus Chelidonium, which has been demonstrated STAT3 and ß-catenin (CTNNB1), all of which are involved in to selectively kill tumor cells without affecting non-malignant cell proliferation, migration, angiogenesis, apoptosis as well as cells. In the present study, the components of NSC-631570 the radiation- and chemo-resistance of HNSCC. The strongest were examined by combined liquid chromatography/mass upregulation occurred for cytochrome P450 1A1 (CYP1A1) spectroscopy (LC-MS) and the effects of NSC-631570 on and 1B1 (CYP1B1), involved in the metabolism of xenobiotics. HNSCC cell lines, as well as primary cells, were analyzed Upregulation of CYP1A1 was at least partially caused by chel- with respect to growth, apoptosis, invasion, angiogenesis erythrine and allocryptopine, as shown by RT-qPCR in two and gene expression. LC-MS identified chelerythrine and HNSCC cell lines. In addition, NSC-631570 showed a high allocryptopine as the major alkaloids of the extract. -

Determining HDAC8 Substrate Specificity by Noah Ariel Wolfson A
Determining HDAC8 substrate specificity by Noah Ariel Wolfson A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Biological Chemistry) in the University of Michigan 2014 Doctoral Committee: Professor Carol A. Fierke, Chair Professor Robert S. Fuller Professor Anna K. Mapp Associate Professor Patrick J. O’Brien Associate Professor Raymond C. Trievel Dedication My thesis is dedicated to all my family, mentors, and friends who made getting to this point possible. ii Table of Contents Dedication ....................................................................................................................................... ii List of Figures .............................................................................................................................. viii List of Tables .................................................................................................................................. x List of Appendices ......................................................................................................................... xi Abstract ......................................................................................................................................... xii Chapter 1 HDAC8 substrates: Histones and beyond ...................................................................... 1 Overview ..................................................................................................................................... 1 HDAC introduction -
Chuanxiong Rhizoma Compound on HIF-VEGF Pathway and Cerebral Ischemia-Reperfusion Injury’S Biological Network Based on Systematic Pharmacology
ORIGINAL RESEARCH published: 25 June 2021 doi: 10.3389/fphar.2021.601846 Exploring the Regulatory Mechanism of Hedysarum Multijugum Maxim.-Chuanxiong Rhizoma Compound on HIF-VEGF Pathway and Cerebral Ischemia-Reperfusion Injury’s Biological Network Based on Systematic Pharmacology Kailin Yang 1†, Liuting Zeng 1†, Anqi Ge 2†, Yi Chen 1†, Shanshan Wang 1†, Xiaofei Zhu 1,3† and Jinwen Ge 1,4* Edited by: 1 Takashi Sato, Key Laboratory of Hunan Province for Integrated Traditional Chinese and Western Medicine on Prevention and Treatment of 2 Tokyo University of Pharmacy and Life Cardio-Cerebral Diseases, Hunan University of Chinese Medicine, Changsha, China, Galactophore Department, The First 3 Sciences, Japan Hospital of Hunan University of Chinese Medicine, Changsha, China, School of Graduate, Central South University, Changsha, China, 4Shaoyang University, Shaoyang, China Reviewed by: Hui Zhao, Capital Medical University, China Background: Clinical research found that Hedysarum Multijugum Maxim.-Chuanxiong Maria Luisa Del Moral, fi University of Jaén, Spain Rhizoma Compound (HCC) has de nite curative effect on cerebral ischemic diseases, *Correspondence: such as ischemic stroke and cerebral ischemia-reperfusion injury (CIR). However, its Jinwen Ge mechanism for treating cerebral ischemia is still not fully explained. [email protected] †These authors share first authorship Methods: The traditional Chinese medicine related database were utilized to obtain the components of HCC. The Pharmmapper were used to predict HCC’s potential targets. Specialty section: The CIR genes were obtained from Genecards and OMIM and the protein-protein This article was submitted to interaction (PPI) data of HCC’s targets and IS genes were obtained from String Ethnopharmacology, a section of the journal database. -

SUMF1 Enhances Sulfatase Activities in Vivo in Five Sulfatase Deficiencies
SUMF1 enhances sulfatase activities in vivo in five sulfatase deficiencies Alessandro Fraldi, Alessandra Biffi, Alessia Lombardi, Ilaria Visigalli, Stefano Pepe, Carmine Settembre, Edoardo Nusco, Alberto Auricchio, Luigi Naldini, Andrea Ballabio, et al. To cite this version: Alessandro Fraldi, Alessandra Biffi, Alessia Lombardi, Ilaria Visigalli, Stefano Pepe, et al.. SUMF1 enhances sulfatase activities in vivo in five sulfatase deficiencies. Biochemical Journal, Portland Press, 2007, 403 (2), pp.305-312. 10.1042/BJ20061783. hal-00478708 HAL Id: hal-00478708 https://hal.archives-ouvertes.fr/hal-00478708 Submitted on 30 Apr 2010 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Biochemical Journal Immediate Publication. Published on 8 Jan 2007 as manuscript BJ20061783 SUMF1 enhances sulfatase activities in vivo in five sulfatase deficiencies Alessandro Fraldi*1, Alessandra Biffi*2,3¥, Alessia Lombardi1, Ilaria Visigalli2, Stefano Pepe1, Carmine Settembre1, Edoardo Nusco1, Alberto Auricchio1, Luigi Naldini2,3, Andrea Ballabio1,4 and Maria Pia Cosma1¥ * These authors contribute equally to this work 1TIGEM, via P Castellino, 111, 80131 Naples, Italy 2San Raffaele Telethon Institute for Gene Therapy (HSR-TIGET), H. San Raffaele Scientific Institute, Milan 20132, Italy 3Vita Salute San Raffaele University Medical School, H. -

Transcriptional Analysis of Sodium Valproate in a Serotonergic Cell Line Reveals Gene Regulation Through Both HDAC Inhibition-Dependent and Independent Mechanisms
bioRxiv preprint doi: https://doi.org/10.1101/837732; this version posted November 12, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Transcriptional analysis of sodium valproate in a serotonergic cell line reveals gene regulation through both HDAC inhibition-dependent and independent mechanisms Priyanka Sinha1,2, Simone Cree1,2, Allison L. Miller1,2, John F. Pearson1,2,3, Martin A. Kennedy1,2. 1Gene Structure and Function Laboratory, Department of Pathology and Biomedical Science, University of Otago, Christchurch, New Zealand. 2Carney Centre for Pharmacogenomics, University of Otago, Christchurch, New Zealand. 3Biostatistics and Computational Biology Unit, University of Otago, Christchurch, New Zealand. Correspondence to: Prof. M. A. Kennedy Department of Pathology and Biomedical Science University of Otago, Christchurch Christchurch, New Zealand Email: [email protected] Keywords: RNA-Seq, NanoString, lithium, valproate, HDAC inhibitor, mood stabilizer 1 bioRxiv preprint doi: https://doi.org/10.1101/837732; this version posted November 12, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Abstract Sodium valproate (VPA) is a histone deacetylase (HDAC) inhibitor, widely prescribed in the treatment of bipolar disorder, and yet the precise modes of therapeutic action for this drug are not fully understood. -

Bioinformatics Classification of Mutations in Patients with Mucopolysaccharidosis IIIA
Metabolic Brain Disease (2019) 34:1577–1594 https://doi.org/10.1007/s11011-019-00465-6 ORIGINAL ARTICLE Bioinformatics classification of mutations in patients with Mucopolysaccharidosis IIIA Himani Tanwar1 & D. Thirumal Kumar1 & C. George Priya Doss1 & Hatem Zayed2 Received: 30 April 2019 /Accepted: 8 July 2019 /Published online: 5 August 2019 # The Author(s) 2019 Abstract Mucopolysaccharidosis (MPS) IIIA, also known as Sanfilippo syndrome type A, is a severe, progressive disease that affects the central nervous system (CNS). MPS IIIA is inherited in an autosomal recessive manner and is caused by a deficiency in the lysosomal enzyme sulfamidase, which is required for the degradation of heparan sulfate. The sulfamidase is produced by the N- sulphoglucosamine sulphohydrolase (SGSH) gene. In MPS IIIA patients, the excess of lysosomal storage of heparan sulfate often leads to mental retardation, hyperactive behavior, and connective tissue impairments, which occur due to various known missense mutations in the SGSH, leading to protein dysfunction. In this study, we focused on three mutations (R74C, S66W, and R245H) based on in silico pathogenic, conservation, and stability prediction tool studies. The three mutations were further subjected to molecular dynamic simulation (MDS) analysis using GROMACS simulation software to observe the structural changes they induced, and all the mutants exhibited maximum deviation patterns compared with the native protein. Conformational changes were observed in the mutants based on various geometrical parameters, such as conformational stability, fluctuation, and compactness, followed by hydrogen bonding, physicochemical properties, principal component analysis (PCA), and salt bridge analyses, which further validated the underlying cause of the protein instability. Additionally, secondary structure and surrounding amino acid analyses further confirmed the above results indicating the loss of protein function in the mutants compared with the native protein. -

EGL Test Description
2460 Mountain Industrial Boulevard | Tucker, Georgia 30084 Phone: 470-378-2200 or 855-831-7447 | Fax: 470-378-2250 eglgenetics.com Mucopolysaccharidosis Type III: SGSH, GNS, HGSNAT, and NAGLU Gene Deletion/Duplication Panel Test Code: HV Turnaround time: 2 weeks CPT Codes: 81228 x1 Condition Description Mucopolysaccharidosis type III (MPS III, Sanfilippo syndrome), is a member of a group of inherited metabolic disorders collectively termed mucopolysaccharidoses (MPS's). The MPS's are caused by a deficiency of lysosomal enzymes required for the degradation of mucopolysaccharides or glycosaminoglycans (GAGs) within the lysosome [1]. When functioning normally, the lysosomal enzymes break down these GAGs, however when the enzyme is deficient, the GAGs build up in the lysosomes causing damage to the body's tissues. The MPS's share a chronic progressive course with multisystem involvement and characteristic physical features such as coarse facies, hypertelorism, and coarse hair. The MPS patients are also characterized by developmental regression, hepatosplenomegaly and characteristic laboratory and radiographic abnormalities. Clinical features of MPS III are similar to other MPS's and include hyperactivity, aggressiveness, and developmental delays in childhood. Mental abilities decline as the disease progresses. Involvement of other organ systems tends to be mild and dysmorphic features are more subtle than those observed in other type of mucopolysaccharidosis [1]. MPS III is caused by a deficiency of any of four lysosomal membrane enzymes, which leads to impaired degradation of heparan sulfate. The forms of MPS III are clinically indistinguishable each other and are caused by mutations in distinct genes. All four forms of MPS III result in buildup of the same GAG, heparin sulfate. -

Combined the SMAC Mimetic and BCL2 Inhibitor Sensitizes
Lee et al. Breast Cancer Research (2020) 22:130 https://doi.org/10.1186/s13058-020-01367-7 RESEARCH ARTICLE Open Access Combined the SMAC mimetic and BCL2 inhibitor sensitizes neoadjuvant chemotherapy by targeting necrosome complexes in tyrosine aminoacyl-tRNA synthase-positive breast cancer Kyung-Min Lee1†, Hyebin Lee2†, Dohyun Han3†, Woo Kyung Moon4, Kwangsoo Kim5, Hyeon Jeong Oh6, Jinwoo Choi7, Eun Hye Hwang8, Seong Eun Kang8, Seock-Ah Im9, Kyung-Hun Lee9 and Han Suk Ryu1,8* Abstract Background: Chemotherapy is the standard treatment for breast cancer; however, the response to chemotherapy is disappointingly low. Here, we investigated the alternative therapeutic efficacy of novel combination treatment with necroptosis-inducing small molecules to overcome chemotherapeutic resistance in tyrosine aminoacyl-tRNA synthetase (YARS)-positive breast cancer. Methods: Pre-chemotherapeutic needle biopsy of 143 invasive ductal carcinomas undergoing the same chemotherapeutic regimen was subjected to proteomic analysis. Four different machine learning algorithms were employed to determine signature protein combinations. Immunoreactive markers were selected using three common candidate proteins from the machine-learning algorithms and verified by immunohistochemistry using 123 cases of independent needle biopsy FFPE samples. The regulation of chemotherapeutic response and necroptotic cell death was assessed using lentiviral YARS overexpression and depletion 3D spheroid formation assay, viability assays, LDH release assay, flow cytometry analysis, and transmission electron microscopy. The ROS- induced metabolic dysregulation and phosphorylation of necrosome complex by YARS were assessed using oxygen consumption rate analysis, flow cytometry analysis, and 3D cell viability assay. The therapeutic roles of SMAC mimetics (LCL161) and a pan-BCL2 inhibitor (ABT-263) were determined by 3D cell viability assay and flow cytometry analysis. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase