Thyroid Disorders—An Update
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thyroid Hormone Misuse and Abuse
Endocrine (2019) 66:79–86 https://doi.org/10.1007/s12020-019-02045-1 REVIEW Thyroid hormone misuse and abuse Victor J. Bernet 1,2 Received: 11 June 2019 / Accepted: 2 August 2019 © Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Thyroid hormone (TH) plays an essential role in human physiology and maintenance of appropriate levels is important for good health. Unfortunately, there are instances in which TH is misused or abused. Such misuse may be intentional such as when individuals take thyroid hormone for unapproved indications like stimulation of weight loss or improved energy. There are instances where healthcare providers prescribe thyroid hormone for controversial or out of date uses and sometimes in supraphysiologic doses. Othertimes, unintentional exposure may occur through supplements or food that unknowingly contain TH. No matter the reason, exposure to exogenous forms of TH places the public at risk for potential adverse side effects. Keywords Thyrotoxicosis ● Thyroid hormone abuse ● Thyroid hormone misuse ● Factitious thyrotoxicosis ● Supplements ● 1234567890();,: 1234567890();,: Analogs Overdose Thyroid hormone misuse and abuse secondary to exogenous TH ingestion that may be unin- tentional or purposeful such as in some cases of Munch- Almost any substance that impacts body physiology and ausen syndrome. Instances of TH misuse can be associated function is at risk for misuse or frank abuse, usually in the with the development of significant side effects. There are misgiven belief that the particular agent whether it be a other instances of chronic, low-grade over treatment with herb, supplement, medication, or hormone has healing TH, which occur for various misreasoning such as weight properties beyond that of which it actually possesses. -

A Case of Thyrotoxic Paralysis Caused by Consumption of Iodocaseine
Journal of Health and Social Sciences 2019; 4,2:277-282 CASE REPORT IN EMERGENCY MEDICINE A case of thyrotoxic paralysis caused by consumption of iodocaseine Antonio Villa1, Gabriella Nucera2 Affiliations: 1 M.D., Department of Emergency, ASST Monza, PO Desio, Monza, Italy 2 M.D., Department of Emergency Medicine, ASST Fatebenefratelli-Sacco, PO Fatebenefratelli, Milano, Italy Corresponding author: Dr Antonio Villa, ASST Monza, PO Desio. Via Fiuggi, 56 20159 Milan, Italy. E-mail: [email protected] Abstract Acute hypokalaemic paralysis is a rare but treatable cause of acute limb weakness. Thyrotoxic paralysis is an uncommon, potentially life-threatening endocrine emergency and it is a rare complication of hyperthyroidism. The most common causes of hyperthyroidism include Graves’ disease, multinodular goiters or solitary thyroid nodule, and iodine-induced thyrotoxicosis ( Jod-Basedow syndrome). Thyreotoxicosis factitia, which is caused by the excessive ingestion of exogenous thyroid hormone or iodine derivatives administration, has been rarely reported as a cause of thyrotoxic paralysis. We describe the case of a young Caucasian male with flaccid paralysis of all four limbs and severe hypokalaemia after inappropriate iodine derivatives (iodocasein) intake to show, in conclusion, how critical care physicians need to be aware of this rare but curable condition. KEY WORDS: Iodocaseine; hypokalaemia; thyrotoxic paralysis. 277 Journal of Health and Social Sciences 2019; 4,2:277-282 Riassunto La paralisi acuta ipokaliemica è una causa rara ma curabile di astenia acuta. La paralisi tireotossica è un'e- mergenza endocrina non comune e potenzialmente pericolosa per la vita ed è una rara complicanza dell'i- pertiroidismo. L'ipertiroidismo è causato prevalentemente dalla malattia di Graves, da gozzi singoli o multi- nodulari, e dalla malattia indotta da iodio ( Jod-Basedow). -
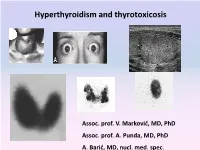
Hyperthyroidism and Thyrotoxicosis
Hyperthyroidism and thyrotoxicosis Assoc. prof. V. Marković, MD, PhD Assoc. prof. A. Punda, MD, PhD A. Barić, MD, nucl. med. spec. Hyperthyroidism- Thyrotoxicosis Hyperthyroidism- elevated serum levels of thyroid hormones caused by overproduction of thyroid hormones Thyrotoxicosis: elevated serum level of thyroid hormones/ excessive amount of circulating thyroid hormone Hyperthyreoidism includes thyreotoxycosis but Thyrotoxicosis is not exclusively caused by hyperthyroidism Classification of thyrotoxicosis Hyperthyroidism Thyrotoxicosis without hyperthyroidism Mb Basedow-Graves Thyrotoxicosis factitia Multinodular toxic goiter Subacute thyroiditis (painfull) Toxic adenoma Subacute thyroiditis (painless) Elevated TSH levels Ectopic thyroid tissue Trophoblastic tumors Iod-Basedow Diffuse toxic goiter (Mb Basedow, Graves) Diffuse toxic goiter Mb. Graves-Basedow Epidemiology and etiology Diffuse toxic goiter (Mb. Graves- Basedow) is an autoimune, multysistemic dissease, wich includes the thyoid gland, infiltrative ophthalmopathy, dermopathy and acropathy. World wide prevalence is about 0,4-2% in women, 0,1% in men, includes 60-90% of hyperthyroidism cases*. It is complex disease with predominant genetic component.& Sex hormones, stress. Disease is caused by TSH receptor stimulating antibodies/ TSH stimulating antibodies (TSAb), in 80-100% patients. *Taunbridge WMG, Vanderpump MPJ. Population screening for autoimmune thyroid disease. Endocriol Metab Clin North Am. 2000;29:239-253. &Brix TH, Kyvik KO, Christensen K, et al. Evdence for a major -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Thyroid Vascularity and Blood Flow
European Journal of Endocrinology (1999) 140 452–456 ISSN 0804-4643 Thyroid vascularity and blood flow are not dependent on serum thyroid hormone levels: studies in vivo by color flow doppler sonography Fausto Bogazzi, Luigi Bartalena, Sandra Brogioni, Alessandro Burelli, Luca Manetti, Maria Laura Tanda, Maurizio Gasperi and Enio Martino Dipartimento di Endocrinologia e Metabolismo, Ortopedia e Traumatologia, Medicina del Lavoro, University of Pisa, Pisa, Italy (Correspondence should be addressed to E Martino, Dipartimento di Endocrinologia e Metabolismo, Ortopedia e Traumatologia, Medicina del Lavoro, Universita` di Pisa, Ospedale di Cisanello, Via Paradisa, 2, 56122 Pisa, Italy) Abstract Objective: Thyroid blood flow is greatly enhanced in untreated Graves’ disease, but it is not known whether it is due to thyroid hormone excess or to thyroid hyperstimulation by TSH-receptor antibody. To address this issue in vivo patients with different thyroid disorders were submitted to color flow doppler sonography (CFDS). Subjects and methods: We investigated 24 normal subjects, and 78 patients with untreated hyperthy- roidism (49 with Graves’ hyperthyroidism, 24 with toxic adenoma, and 5 patients with TSH-secreting pituitary adenoma (TSHoma)), 19 patients with thyrotoxicosis (7 with thyrotoxicosis factitia, and 12 with subacute thyroiditis), 37 euthyroid patients with goitrous Hashimoto’s thyroiditis, and 21 untreated hypothyroid patients with Hashimoto’s thyroiditis. Results: Normal subjects had CFDS pattern 0 (absent or minimal intraparenchimal spots) and mean intraparenchimal peak systolic velocity (PSV) of 4.8 6 1.2 cm/s. Patients with spontaneous hyperthy- roidism due to Graves’ disease, TSHoma, and toxic adenoma had significantly increased PSV (P < 0.0001, P = 0.0004, P < 0.0001 respectively vs controls) and CFDS pattern. -

Oxidative Stress and Antioxidant Status in Hypo- and Hyperthyroidism
Chapter 8 Oxidative Stress and Antioxidant Status in Hypo- and Hyperthyroidism Mirela Petrulea, Adriana Muresan and Ileana Duncea Additional information is available at the end of the chapter http://dx.doi.org/10.5772/51018 1. Introduction Thyroid hormones are involved in the regulation of basal metabolic state and in oxidative metabolism [1]. They can cause many changes in the number and activity of mitochondrial respiratory chain components. This may result in the increased generation of reactive oxygen species (ROS) [2,3]. Oxidative stress is a general term used to describe a state of damage caused by ROS [4]. ROS have a high reactivity potential, therefore they are toxic and can lead to oxidative damage in cellular macromolecules such as proteins, lipids and DNA [5]. In fact, the cell contains a variety of substances capable of scavenging the free radicals, protecting them from harmful effects. Among the enzymatic antioxidants, are glutathione reductase (GR), glutathione peroxydase (GPx), catalase (CAT), superoxide dismutase (SOD), while the non-enzymatic antioxidants are glutathione (GSH), vitamin E, vitamin C, β- carotene, and flavonoids [6]. When ROS generation exceeds the antioxidant capacity of cells, oxidative stress develops [7]. Life means a continuous struggle for energy, which is required to fight against entropy. The most effective way to obtain energy is oxidation. Oxidative processes predominantly occur in mitochondria [8]. On the other hand, mitochondria are the favorite targets of thyroid hormones. During thyroid hormone synthesis, there is a constant production of oxygenated water, which is absolutely indispensable for iodine intrafollicular oxidation in the presence of thyroid peroxidase. In recent years, the possible correlation between impaired thyroid gland function and reactive oxygen species has been increasingly taken into consideration [9]. -

ABSTRACT Title of Dissertation: Insight Into the Structure And
ABSTRACT Title of dissertation: Insight into the Structure and Mechanism of Iodotyrosine Deiodinase, the First Mammalian Member of the NADH Oxidase / Flavin Reductase Superfamily James Ambrose Watson, Jr. Doctor of Philosophy, 2006 Dissertation directed by: Professor Steven E. Rokita Department of Chemistry and Biochemistry Iodotyrosine deiodinase (IYD) has remained poorly characterized for nearly 50 years in spite of its function as an iodine salvage pathway and its role in regulation of mammalian basal metabolism. IYD catalyzes the reductive deiodination of both mono- and diiodotyrosine, the iodinated side-products of thyroid hormone production. The Rokita lab previously purified IYD from porcine thyroids and identified a putative dehalogenase gene. The work in this dissertation confirms the identity of the gene that encodes IYD -1 -1 through expression in HEK293 cells (KM = 4.4 ± 1.7 µM and Vmax = 12 ± 1 nmol hr µg ) and, furthermore, identifies IYD as the first mammalian member of the NADH oxidase/flavin reductase superfamily, a protein fold previously found only in bacteria. In addition, a three- dimensional model of the NADH oxidase/flavin reductase domain of IYD was constructed based on the x-ray crystal structure coordinates (Protein Data Bank code 1ICR) of the minor nitroreductase from Escherichia coli. The model also predicts structural features of IYD, including interactions between the flavin bound to IYD and one of three conserved cysteines. To investigate the role of the NADH oxidase/flavin reductase domain plays in electron transfer, two truncation mutants were generated: IYD-NR (residues 81-285) and IYD-∆TM (residues 34-285) encoding transmembrane-domain deleted IYD. -

Iodotyrosine Deiodinase from Selected Phyla Engineered for Bacterial Expression
ABSTRACT Title of Document: IODOTYROSINE DEIODINASE FROM SELECTED PHYLA ENGINEERED FOR BACTERIAL EXPRESSION Jennifer Marilyn Buss Doctor of Philosophy, 2012 Directed By: Professor Steven E. Rokita Department of Chemistry and Biochemistry Iodide is a well known halogen necessary for development. The majority of iodide processing in biological systems occurs in the thyroid gland. Iodide salvage is essential to thyroid hormone metabolism and metabolic regulation. The DEHAL1 gene product iodotyrosine deiodinase (IYD) is responsible for deiodination of the mono- and diiodotyrosine byproducts of thyroid hormone synthesis (triiodothyronine and thyroxine, T3 and T4, respectively). IYD is a membrane-bound flavoprotein comprised of three domains with the catalytic domain belonging to the NADPH oxidase/flavin reductase structural superfamily. This enzyme required engineering for expression of soluble protein in E. coli and was characterized using CD spectra, kinetic rate constants, binding constants of substrates, and crystal structure. Analysis of the crystal structure of IYD indicates a dimer with an active site comprising of both monomers and orienting the C-I bond of iodotyrosine substrate stacking above the N5 of the flavin mononucleotide (FMN) required for activity. The crystal structure also identifies an active site lid that distinguishes IYD from other proteins in the NADPH oxidase/flavin reductase superfamily. Three amino acids (E153, Y157, and K178) on the active site lid form hydrogen bonding and electrostatic contacts with the zwitterionic portion of the substrate. Mutation to any of these three amino acids significantly decreases substrate-binding affinity and enzymatic activity. Homologous sequences of IYD were identified in other organisms and four sequences as representatives from their phyla were expressed in E. -

Towards a Halophenol Dehalogenase from Iodotyrosine Deiodinase Via Computational Design
Towards a Halophenol Dehalogenase from Iodotyrosine Deiodinase via Computational Design Zuodong Sun and Steven E. Rokita* Department of Chemistry, Johns Hopkins University, 3400 N. Charles St., Baltimore, MD, 21218 ABSTRACT: Reductive dehalogenation offers an attractive approach for removing halogenated pollutants from the environment and iodotyrosine deiodinase (IYD) may contribute to this process after it can be engineered to accept a broad range of substrates. The selectivity of IYD is controlled in part by an active site loop of approximately 26 amino acids. In the absence of substrate, the loop is disordered and only folds into a compact helix-turn-helix upon halotyrosine association. The design algorithm of Rosetta was applied to redesign this loop for response to 2-iodophenol rather than iodotyrosine. One strategy using a restricted number of substitutions for increasing the inherent stability of the helical regions failed to generate variants with the desired properties. A series of point mutations identified strong epistatic interactions that impeded adaptation of IYD. This limitation was overcome by a second strategy that placed no restrictions on side chain substitution by Rosetta. Nine representative designs containing between 14-18 substitutions over 26 contiguous sites were evaluated experimentally. The top performing catalyst (UD08) supported a 4.5-fold increase in turnover of 2-iodophenol and suppressed turnover of iodotyrosine by 2000-fold relative to the native enzyme. The active site loop of UD08 appeared less disordered than the native sequence in the absence of substrate as evident from their relative sensitivity to proteolysis. Protection from proteolysis increased 9-fold for UD08 in the presence of 2-iodophenol and nearly rivaled the equivalent response of wild type IYD to iodotyrosine. -

Endocrine Module (PYPP 5260), Thyroid Section, Spring 2002
Endocrine Module (PYPP 5260), Thyroid Section, Spring 2002 THYROID HORMONE TUTORIAL: THYROID PATHOLOGY Jack DeRuiter I. INTRODUCTION Thyroid disorder is a general term representing several different diseases involving thyroid hormones and the thyroid gland. Thyroid disorders are commonly separated into two major categories, hyperthyroidism and hypothyroidism, depending on whether serum thyroid hormone levels (T4 and T3) are increased or decreased, respectively. Thyroid disease generally may be sub-classified based on etiologic factors, physiologic abnormalities, etc., as described in each section below. More than 13 million Americans are affected by thyroid disease, and more than half of these remain undiagnosed. The American Association of Clinical Endocrinologists (AACE) has initiated a campaign to increase public awareness of thyroid disorders and educate Americans about key periods, from birth to advanced age, when people are at increased risk for developing a thyroid disorder (see below). The diagnosis of thyroid disease can be particularly challenging. Patients often present with vague, general clinical manifestations; in particular, the elderly may not associate the signs and symptoms with a disease process and thus may not bring them to the attention of their primary care provider. The prevalence and incidence of thyroid disorders is influenced primarily by sex and age. Thyroid disorders are more common in women than men, and in older adults compared with younger age groups. The prevalence of unsuspected overt hyperthyroidism and hypothyroidism are both estimated to be 0.6% or less in women, based on several epidemiologic studies. Age is also a factor; for overt hyperthyroidism, the prevalence rate is 1.4% for women aged 60 or older and 0.45% for women aged 40 to 60. -

Thyroid Emergencies
REVIEW ARTICLE Thyroid emergencies Dorina Ylli1, Joanna Klubo ‑Gwiezdzinska2, Leonard Wartofsky3,4 1 Endocrinology Division, University of Medicine, Tirana, Albania 2 National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Bethesda, Maryland, United States 3 Endocrinology Division, Department of Medicine, Georgetown University School of Medicine, Washington DC, United States 4 MedStar Health Research Institute, MedStar Washington Hospital Center, Washington DC, United states KEY WORDS ABSTRACT coma, critical care, Myxedema coma and thyroid storm are among the most common endocrine emergencies presenting to hypothermia, general hospitals. Myxedema coma represents the most extreme, life ‑threatening expression of severe hypothyroidism, hypothyroidism, with patients showing deteriorating mental status, hypothermia, and multiple organ thyrotoxicosis system abnormalities. It typically appears in patients with preexisting hypothyroidism via a common pathway of respiratory decompensation with carbon dioxide narcosis leading to coma. Without early and appropriate therapy, the outcome is often fatal. The diagnosis is based on history and physical find‑ ings at presentation and not on any objective thyroid laboratory test. Clinically based scoring systems have been proposed to aid in the diagnosis. While it is a relatively rare syndrome, the typical patient is an elderly woman (thyroid hypofunction being much more common in women) who may or may not have a history of previously diagnosed or treated thyroid dysfunction. Thyrotoxic storm or thyroid crisis is also a rare condition, established on the basis of a clinical diagnosis. The diagnosis is based on the pres‑ ence of severe hyperthyroidism accompanied by elements of systemic decompensation. Considering that mortality is high without aggressive treatment, therapy must be initiated as early as possible in a critical care setting. -

Effects of Inorganic Iodide on the Intermediary Carbohydrate Metabolism of Surviving Sheep Thyroid Slices
EFFECTS OF INORGANIC IODIDE ON THE INTERMEDIARY CARBOHYDRATE METABOLISM OF SURVIVING SHEEP THYROID SLICES William L. Green, Sidney H. Ingbar J Clin Invest. 1963;42(11):1802-1815. https://doi.org/10.1172/JCI104865. Research Article Find the latest version: https://jci.me/104865/pdf Journal of Clinical Investigation Vol. 42, No. 11, 1963 EFFECTS OF INORGANIC IODIDE ON THE INTERMEDIARY CARBOHYDRATE METABOLISM OF SURVIVING SHEEP THYROID SLICES * By WILLIAM L. GREEN t AND SIDNEY H. INGBAR t (From the Thorndike Memorial Laboratory and Second and Fourth [Harvard] Medical Services, Boston City Hospital, and the Department of Medicine, Harvard Medical School, Boston, Mass.; and the Department of Medicine, Seton Hall College of Medicine, Jersey City, N. J.) (Submitted for publication April 2, 1963; accepted July 31, 1963) The rate of hormone formation by the thyroid changes in the rate of hormone formation in- in vivo is greatly influenced by acute alterations duced by varying the availability of iodide to thy- in the concentration of inorganic iodide in the roid slices in vitro are associated with, or can be extracellular fluid. In the rat (1-3) and in man ascribed to, alterations of intermediary metabolism (4, 5), increasing concentrations of iodide in the within the thyroid. A preliminary report of these plasma are associated with increased thyroidal studies has appeared (17). uptake of iodine until a critical concentration of iodide is reached. Beyond this range, the forma- METHODS tion of hormone declines. A similar relationship Preparation of slices. Thyroid glands were obtained between extracellular iodide concentration and from freshly killed sheep and were brought from the organic iodinations occurs in vitro in slices of abattoir to the laboratory packed in ice.