Chapter14.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Emerging Evidence for a Central Epinephrine-Innervated A1- Adrenergic System That Regulates Behavioral Activation and Is Impaired in Depression
Neuropsychopharmacology (2003) 28, 1387–1399 & 2003 Nature Publishing Group All rights reserved 0893-133X/03 $25.00 www.neuropsychopharmacology.org Perspective Emerging Evidence for a Central Epinephrine-Innervated a1- Adrenergic System that Regulates Behavioral Activation and is Impaired in Depression ,1 1 1 1 1 Eric A Stone* , Yan Lin , Helen Rosengarten , H Kenneth Kramer and David Quartermain 1Departments of Psychiatry and Neurology, New York University School of Medicine, New York, NY, USA Currently, most basic and clinical research on depression is focused on either central serotonergic, noradrenergic, or dopaminergic neurotransmission as affected by various etiological and predisposing factors. Recent evidence suggests that there is another system that consists of a subset of brain a1B-adrenoceptors innervated primarily by brain epinephrine (EPI) that potentially modulates the above three monoamine systems in parallel and plays a critical role in depression. The present review covers the evidence for this system and includes findings that brain a -adrenoceptors are instrumental in behavioral activation, are located near the major monoamine cell groups 1 or target areas, receive EPI as their neurotransmitter, are impaired or inhibited in depressed patients or after stress in animal models, and a are restored by a number of antidepressants. This ‘EPI- 1 system’ may therefore represent a new target system for this disorder. Neuropsychopharmacology (2003) 28, 1387–1399, advance online publication, 18 June 2003; doi:10.1038/sj.npp.1300222 Keywords: a1-adrenoceptors; epinephrine; motor activity; depression; inactivity INTRODUCTION monoaminergic systems. This new system appears to be impaired during stress and depression and thus may Depressive illness is currently believed to result from represent a new target for this disorder. -

General Anaesthesia in Oral Surgery and Outpatient Surgery History
Department of Oral- and Maxillofacial Surgery, Semmelweis University Budapest Head of Department: Dr. Németh Zsolt General anaesthesia in oral surgery and outpatient surgery History 1844 Horace Wells nitrous oxide extraction of one of his own wisdom teeth by a colleague 1846 William Morton (pupil of Wells) ether extraction 1946 introduction of lidocaine General anaesthesia should be strictly limited to those patients and clinical situations in which local anaesthesia (with or without sedation) is not an option. Bourne JG. General anaesthesia in the dental surgery. B Dental J 1962; 113: 54-7. Coleman F. The history of nitrous oxide anaesthesia. Dental Record 1942; 62: 143-9 Naveen Malhotra General Anaesthesia for Dentistry ndian Journal of Anaesthesia 2008;52:Suppl (5):725-737 Types of general anaesthesia Outpatient anaesthesia • Dental chair anaesthesia Relative analgesia for simple extraction • Day care anaesthesia Conscious sedation (Sedoanalgesia) for minor oral surgery In patient anaesthesia Intubation with or without neuromuscular blocking for complicated extractions, oral- and maxillofacial surgical procedures Indications of general anaesthesia • Acute infection (pain) • Children • Mentally challenged patients • Dental phobia • Allergy to local anaesthetics • Extensive dentistry & facio-maxillary surgery Equipments • anaesthesia machine, vaporizers • oxygen, nitrous oxide • breathing circuits (adult and pediatric) • nasal and facial masks • oral and nasal air-ways • different laryngoscopes with all sizes of blades • nasal and -

Methohexital(BAN, Rinn)
1788 General Anaesthetics metabolic pathways include hydroxylation of the 3. Lökken P, et al. Conscious sedation by rectal administration of Methohexital Sodium (BANM, rINNM) midazolam or midazolam plus ketamine as alternatives to gener- cyclohexone ring and conjugation with glucuronic ac- al anesthesia for dental treatment of uncooperative children. Compound 25398; Enallynymalnatrium; Méthohexital Sodique; id. The beta phase half-life is about 2.5 hours. Keta- Scand J Dent Res 1994; 102: 274–80. Methohexitone Sodium; Metohexital sódico; Natrii Methohexi- 4. Louon A, et al. Sedation with nasal ketamine and midazolam for talum. mine is excreted mainly in the urine as metabolites. It cryotherapy in retinopathy of prematurity. Br J Ophthalmol crosses the placenta. 1993; 77: 529–30. Натрий Метогекситал 5. Zsigmond EK, et al. A new route, jet-injection for anesthetic in- C14H17N2NaO3 = 284.3. ◊ References. duction in children–ketamine dose-range finding studies. Int J CAS — 309-36-4; 22151-68-4; 60634-69-7. 1. Clements JA, Nimmo WS. Pharmacokinetics and analgesic ef- Clin Pharmacol Ther 1996; 34: 84–8. ATC — N01AF01; N05CA15. fect of ketamine in man. Br J Anaesth 1981; 53: 27–30. 6. Kronenberg RH. Ketamine as an analgesic: parenteral, oral, rec- tal, subcutaneous, transdermal and intranasal administration. J ATC Vet — QN01AF01; QN05CA15. 2. Grant IS, et al. Pharmacokinetics and analgesic effects of IM and Pain Palliat Care Pharmacother 2002; 16: 27–35. oral ketamine. Br J Anaesth 1981; 53: 805–9. Pharmacopoeias. US includes Methohexital Sodium for In- jection. 3. Grant IS, et al. Ketamine disposition in children and adults. Br J Nonketotic hyperglycinaemia. -

Local Anaesthesia for Major General Surgical Postgrad Med J: First Published As 10.1136/Pgmj.72.844.105 on 1 February 1996
Postgrad Med J' 1996; 72: 105-108 C) The Fellowship of Postgraduate Medicine, 1996 Local anaesthesia for major general surgical Postgrad Med J: first published as 10.1136/pgmj.72.844.105 on 1 February 1996. Downloaded from procedures A review of 1 16 cases over 12 years A Dennison, N Oakley, D Appleton, J Paraskevopoulos, D Kerrigan, J Cole, WEG Thomas Summary ation was collated from medical notes, anaes- Between 1980 and 1992, 116 patients had thetic records and operation notes. Cases in either a simple mastectomy (32) or intra- which local anaesthesia was augmented by abdominal procedures (84) under local regional or intravenous techniques were exc- anaesthesia (0.5-1% lignocaine with luded from the study. Patients were not 1:200 000 adrenaline). A wide variety of included ifthey had neck/head or limb surgery, general surgical procedures were feasible abdominal hernia repair, simple drainage of using only supplementary intravenous intra-abdominal abscess or any minor proce- sedation (54%). Complications were un- dures including peritoneo-venous shunts, common and related to surgical proce- laparoscopic or endoscopic procedures. dure (three incorrect diagnoses, three The 116 patients presented in the study are procedures impossible) rather than the those who had intra-abdominal surgery (84; 53 anaesthetic technique. There were no women, 31 men) or simple mastectomy (32). anaesthetic toxicity or postoperative pro- The median age was 74 years (range 27-92) blems. Local anaesthesia is extremely and all the patients were grade III or worse on safe and facilitates larger surgical proce- the American Society of Anaesthesiologists dures than is generally appreciated. -

Nerve Blocks for Surgery on the Shoulder, Arm Or Hand
Nerve blocks for surgery on the shoulder, arm or hand Information for patients and families First Edition 2015 www.rcoa.ac.uk/patientinfo Nerve blocks for surgery on the shoulder, arm or hand This leaflet is for anyone who is thinking about having a nerve block for an operation on the shoulder, arm or hand. It will be of particular interest to people who would prefer not to have a general anaesthetic. The leaflet has been written with the help of patients who have had a nerve block for their operation. Throughout this leaflet we have used the above symbol to highlight key facts. Brachial plexus block? The brachial plexus is the group of nerves that lies between your neck and your armpit. It contains all the nerves that supply movement and feeling to your arm – from your shoulder to your fingertips. A brachial plexus block is an injection of local anaesthetic around the brachial plexus. It ‘blocks’ information travelling along these nerves. It is a type of nerve block. Your arm becomes numb and immobile. You can then have your operation without feeling anything. The block can also provide excellent pain relief for between three and 24 hours, depending on what kind of local anaesthetic is used. A brachial plexus block rarely affects the rest of the body so it is particularly advantageous for patients who have medical conditions which put them at a higher risk for a general anaesthetic. A brachial plexus block may be combined with a general anaesthetic or with sedation. This means you have the advantage of the pain relief provided by a brachial plexus block, but you are also unconscious or sedated during the operation. -

Cocaine Intoxication and Hypertension
THE EMCREG-INTERNATIONAL CONSENSUS PANEL RECOMMENDATIONS Cocaine Intoxication and Hypertension Judd E. Hollander, MD From the Department of Emergency Medicine, University of Pennsylvania, Philadelphia, PA. 0196-0644/$-see front matter Copyright © 2008 by the American College of Emergency Physicians. doi:10.1016/j.annemergmed.2007.11.008 [Ann Emerg Med. 2008;51:S18-S20.] with cocaine intoxication is analogous to that of the patient with hypertension: the treatment should be geared toward the Cocaine toxicity has been reported in virtually all organ patient’s presenting complaint. systems. Many of the adverse effects of cocaine are similar to When the medical history is clear and symptoms are mild, adverse events that can result from either acute hypertensive laboratory evaluation is usually unnecessary. In contrast, if the crisis or chronic effects of hypertension. Recognizing when the patient has severe toxicity, evaluation should be geared toward specific disease requires treatment separate from cocaine toxicity the presenting complaint. Laboratory evaluation may include a is paramount to the treatment of patients with cocaine CBC count; determination of electrolyte, glucose, blood urea intoxication. nitrogen, creatine kinase, and creatinine levels; arterial blood The initial physiologic effect of cocaine on the cardiovascular gas analysis; urinalysis; and cardiac marker determinations. system is a transient bradycardia as a result of stimulation of the Increased creatine kinase level occurs with rhabdomyolysis. vagal nuclei. Tachycardia typically ensues, predominantly from Cardiac markers are increased in myocardial infarction. Cardiac increased central sympathetic stimulation. Cocaine has a troponin I is preferred to identify acute myocardial13 infarction. cardiostimulatory effect through sensitization to epinephrine A chest radiograph should be obtained in patients with and norepinephrine. -
Atopic Children and Use of Prescribed Medication: a Comprehensive Study in General Practice
RESEARCH ARTICLE Atopic children and use of prescribed medication: A comprehensive study in general practice David H. J. Pols1*, Mark M. J. Nielen2, Arthur M. Bohnen1, Joke C. Korevaar2, Patrick J. E. Bindels1 1 Department of General Practice, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands, 2 NIVEL, Netherlands Institute for Health Services Research, Utrecht, The Netherlands a1111111111 * [email protected] a1111111111 a1111111111 a1111111111 Abstract a1111111111 Purpose A comprehensive and representative nationwide general practice database was explored to study associations between atopic disorders and prescribed medication in children. OPEN ACCESS Citation: Pols DHJ, Nielen MMJ, Bohnen AM, Korevaar JC, Bindels PJE (2017) Atopic children Method and use of prescribed medication: A All children aged 0±18 years listed in the NIVEL Primary Care Database in 2014 were comprehensive study in general practice. PLoS ONE 12(8): e0182664. https://doi.org/10.1371/ selected. Atopic children with atopic eczema, asthma and allergic rhinitis (AR) were journal.pone.0182664 matched with controls (not diagnosed with any of these disorders) within the same general Editor: Anthony Peter Sampson, University of practice on age and gender. Logistic regression analyses were performed to study the differ- Southampton School of Medicine, UNITED ences in prescribed medication between both groups by calculating odds ratios (OR); 93 dif- KINGDOM ferent medication groups were studied. Received: March 24, 2017 Accepted: July 13, 2017 Results Published: August 24, 2017 A total of 45,964 children with at least one atopic disorder were identified and matched with Copyright: © 2017 Pols et al. This is an open controls. Disorder-specific prescriptions seem to reflect evidence-based medicine guide- access article distributed under the terms of the lines for atopic eczema, asthma and AR. -

An Introduction to Anaesthesia
What You Need to KNoW about An introduction to anaesthesia Introduction divided into three stages: induction, main- n Central neuraxial block, e.g. spinal or Anaesthetic experience in the undergradu- tenance and emergence. epidural (Figure 1 and Table 1). ate timetable is often very limited so it can In regional anaesthesia, nerve transmis- remain somewhat of a mysterious practice sion is blocked, and the patient may stay Components of a general well into specialist training. This introduc- awake or be sedated or anaesthetized dur- anaesthetic tion to the components of an anaesthetic ing a procedure. Techniques used include: A general anaesthetic always involves an will help readers to get more from clinical n Local anaesthetic field block hypnotic agent, usually an analgesic and attachments in surgery and anaesthetics or n Peripheral nerve block may also include muscle relaxation. The serve as an introduction to the topic for n Nerve plexus block combination is referred to as the ‘triad of novice or non-anaesthetists. anaesthesia’. Figure 1. Schematic vertical longitudinal section The relative importance of each com- Types and sites of anaesthesia of vertebral column and structures encountered ponent depends on surgical and patient The term anaesthesia comes from the when performing central neuraxial blocks. * factors: the intervention planned, site, Greek meaning loss of sensation. negative pressure space filled with fat and surgical access requirement and the Anaesthetic practice has evolved from a venous plexi. † extends to S2, containing degree of pain or stimulation anticipated. need for pain relief and altered conscious- arachnoid mater, CSF, pia mater, spinal cord The technique is tailored to the individu- ness to allow surgery. -
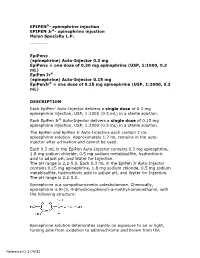
Epipen Injection Label
EPIPEN®- epinephrine injection EPIPEN Jr®- epinephrine injection Mylan Specialty L.P. ---------- EpiPen® (epinephrine) Auto-Injector 0.3 mg EpiPen® = one dose of 0.30 mg epinephrine (USP, 1:1000, 0.3 mL) EpiPen Jr® (epinephrine) Auto-Injector 0.15 mg EpiPenJr® = one dose of 0.15 mg epinephrine (USP, 1:2000, 0.3 mL) DESCRIPTION Each EpiPen® Auto-Injector delivers a single dose of 0.3 mg epinephrine injection, USP, 1:1000 (0.3 mL) in a sterile solution. Each EpiPen Jr® Auto-Injector delivers a single dose of 0.15 mg epinephrine injection, USP, 1:2000 (0.3 mL) in a sterile solution. The EpiPen and EpiPen Jr Auto-Injectors each contain 2 mL epinephrine solution. Approximately 1.7 mL remains in the auto- injector after activation and cannot be used. Each 0.3 mL in the EpiPen Auto-Injector contains 0.3 mg epinephrine, 1.8 mg sodium chloride, 0.5 mg sodium metabisulfite, hydrochloric acid to adjust pH, and Water for Injection. The pH range is 2.2-5.0. Each 0.3 mL in the EpiPen Jr Auto-Injector contains 0.15 mg epinephrine, 1.8 mg sodium chloride, 0.5 mg sodium metabisulfite, hydrochloric acid to adjust pH, and Water for Injection. The pH range is 2.2-5.0. Epinephrine is a sympathomimetic catecholamine. Chemically, epinephrine is B-(3, 4-dihydroxyphenyl)-a-methyl-aminoethanol, with the following structure: Epinephrine solution deteriorates rapidly on exposure to air or light, turning pink from oxidation to adrenochrome and brown from the Reference ID: 3176782 formation of melanin. -

2020 AAHA Anesthesia and Monitoring Guidelines for Dogs and Cats*
VETERINARY PRACTICE GUIDELINES 2020 AAHA Anesthesia and Monitoring Guidelines for Dogs and Cats* Tamara Grubb, DVM, PhD, DACVAAy, Jennifer Sager, BS, CVT, VTS (Anesthesia/Analgesia, ECC)y, James S. Gaynor, DVM, MS, DACVAA, DAIPM, CVA, CVPP, Elizabeth Montgomery, DVM, MPH, Judith A. Parker, DVM, DABVP, Heidi Shafford, DVM, PhD, DACVAA, Caitlin Tearney, DVM, DACVAA ABSTRACT Risk for complications and even death is inherent to anesthesia. However, the use of guidelines, checklists, and training can decrease the risk of anesthesia-related adverse events. These tools should be used not only during the time the patient is unconscious but also before and after this phase. The framework for safe anesthesia delivered as a continuum of care from home to hospital and back to home is presented in these guidelines. The critical importance of client commu- nication and staff training have been highlighted. The role of perioperative analgesia, anxiolytics, and proper handling of fractious/fearful/aggressive patients as components of anesthetic safety are stressed. Anesthesia equipment selection and care is detailed. The objective of these guidelines is to make the anesthesia period as safe as possible for dogs and cats while providing a practical framework for delivering anesthesia care. To meet this goal, tables, algorithms, figures, and “tip” boxes with critical information are included in the manuscript and an in-depth online resource center is available at aaha.org/anesthesia. (J Am Anim Hosp Assoc 2020; 56:---–---. DOI 10.5326/JAAHA-MS-7055) AFFILIATIONS Other recommendations are based on practical clinical experience and From Washington State University College of Veterinary Medicine, Pullman, a consensus of expert opinion. -
Patients on Beta-Blockers
Systemic Allergic & Immunoglobulin Disorders Bryan L. Martin, DO, MMAS, FACAAI, FAAAAI, FACP, FACOI Emeritus Professor of Medicine and Pediatrics President, American College of Allergy, Asthma & Immunology Disclosures . None 2 Objectives . Pass the boards! . Recognize anaphylaxis and understand the new guidelines for the treatment of anaphylaxis . Compare and contrast anaphylactic and anaphylactoid reactions 3 The Patient . 45 year old woman goes to lunch with her friends . While eating she develops GI upset, dizziness, shortness of breath and hives . Her friends drive her to your nearby clinic Initial Evaluation . Your nurse gets the history of sudden onset of GI upset, dizziness, shortness of breath and hives while eating a shrimp salad. The patient now has audible wheezing, tachycardia, and a blood pressure of 110/60 . Your initial response . Take a detailed history of everything the patient had to eat for lunch . Ask if she has a history of any medical issues such as asthma, diabetes or heart disease . Give nebulized beta agonist . Give 50 mg of oral diphenhydramine . Give 0.3 ml of IM epinephrine Anaphylaxis presentation . Your nurse gets the history of sudden onset of GI upset, dizziness, shortness of breath and hives while eating lunch. The patient now has audible wheezing, tachycardia, and a blood pressure of 110/60 . Your initial response . Take a detailed history of everything the patient had to eat for lunch . Ask if she has a history of any medical issues such as asthma, diabetes or heart disease . Give nebulized beta agonist . Give 50 mg of oral diphenhydramine . Give 0.3 ml of IM epinephrine Initial Response to anaphylaxis . -

Diphenhydramine (Systemic) Epinephrine (Systemic)
DIPHENHYDRAMINE (SYSTEMIC) ^ Diphenhist [OTC] see DiphenhydrAMINE (Systemic) on page 34 Insomnia, occasional: Oral: Children 2 to 12 years, weighing 10 to 50 kg (off-label use): DiphenhydrAMINE (Systemic) Limited data available: 1 mg/kg administered 30 minutes before bedtime; maximum single dose: 50 mg (Russo, 1976) Brand Names: US Aler-Dryl [OTC]; Allergy Relief Childrens Children ≥12 years and Adolescents: Refer to adult dosing. [OTC]; Allergy Relief [OTC]; Altaryl [OTC]; Anti-Hist Allergy [OTC]; Motion sickness: Banophen [OTC]; Benadryl Allergy Childrens [OTC]; Benadryl Prophylaxis: Oral: Allergy [OTC]; Benadryl Dye-Free Allergy [OTC]; Benadryl [OTC]; Manufacturer's labeling: Infants, Children, and Adolescents: Complete Allergy Medication [OTC]; Complete Allergy Relief [OTC]; Note: Administer 30 minutes before motion Dicopanol FusePaq; Dicopanol RapidPaq; Diphen [OTC]; Diphenh- Weight-directed dosing: 5 mg/kg/day divided into 3 to 4 doses; ist [OTC]; Genahist [OTC]; Geri-Dryl [OTC]; GoodSense Allergy maximum: 300 mg daily Relief [OTC]; Naramin [OTC]; Nighttime Sleep Aid [OTC]; Nytol Fixed dosing: 12.5 to 25 mg 3 to 4 times daily Maximum Strength [OTC]; Nytol [OTC]; Ormir [OTC]; PediaCare Alternate dosing: Children 2 to 12 years: Limited data available: Childrens Allergy [OTC]; Pharbedryl; Pharbedryl [OTC]; Q-Dryl 0.5 to 1 mg/kg/dose every 6 hours; maximum single dose: [OTC]; QlearQuil Nighttime Allergy [OTC]; Quenalin [OTC] [DSC]; 25 mg. First dose should be administered 1 hour before travel Scot-Tussin Allergy Relief [OTC]; Siladryl