Conversion of Morphology of ICD-O-2 to ICD-10
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Rare Skin Cancers in General Practice
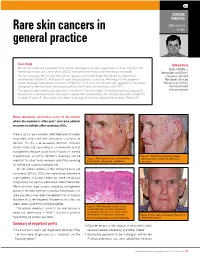
CLINICAL PRACTICE Skin cancer Rare skin cancers in series general practice Case study Anthony Dixon Mr LA has long been troubled with actinic damage to his skin, especially his face. He has had MBBS, FACRRM, is many squamous cell carcinomas (SCCs) removed and many solar keratoses managed. dermasurgeon and Director On this occasion Mr LA had two actinic lesions on his left cheek that failed to respond to of Research, Skin Alert cryotherapy (Figure 1). A biopsy of each site produced a surprise. Histology of the superior Skin Cancer Clinics and lesion revealed sebaceous carcinoma (Figure 2). This is an uncommon yet aggressive cutaneous Skincanceronly, Belmont, malignancy derived from sebaceous glands. The 5 year survival rate is 60–70%. Victoria. anthony@ The tumour was widely excised with a minimum 10 mm margin. A multidisciplinary approach skincanceronly.com resulted in a decision not to proceed to adjunctive radiotherapy. The wound was well healed by 8 weeks (Figure 3). Four years on there is no sign of local or regional recurrence (Figure 4). Many sebaceous carcinomas occur on the eyelids where the outcome is often poor;1 and some patients are prone to multiple other cutaneous SCCs. There is also a rare syndrome called Muir-torre of visceral neoplasms associated with sebaceous carcinoma on the skin.2 As this is an autosomal dominant condition, family history and counselling is an esssential part of management (enquire about family history of internal malignancies). A family member's diagnosis can be Figure 3. Satisfactory healing 8 weeks Figure 1. Two actinic lesions on the left face following wide excision of sebaceous important for other family members and offers screening have failed to respond to cryotherapy carcinoma for internal and cutaneous malignancies. -

A Rare Bone Tumor
OPEN ACCESS L E T T E R T O T H E E D I T O R Periosteal Desmoplastic Fibroma of Radius: A Rare Bone Tumor Aniqua Saleem1,* Hira Saleem2 1 Radiology Department, District Head Quarters Hospital, Rawalpindi Medical University, Rawalpindi 2 Department of Surgery, Shifa International Hospital, Islamabad. Correspondence*: Dr. Aniqua Saleem, Radiology Department, District Head Quarters Hospital, Rawalpindi Medical University, Rawalpindi E-mail: [email protected] © 2019, Saleem et al, Submitted: 05-04-2019 Accepted: 09-06-2019 Conflict of Interest: None Source of Support: Nil This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. DEAR SIR Desmoplastic fibroma is an extremely rare tumor of enhancement on post contrast images and with adjacent bone with a reported incidence of 0.11 % of all primary bone involvement as was evident by focal cortical inter- bone tumors. The most common site of involvement is ruption, mild endosteal thickening and irregularity and mandible (reported incidence 22% of all Desmoplastic also mild ulnar shaft remodeling (Fig. 3a, 3b). To further fibroma cases) followed by metaphysis of long bones. characterize the lesion, Tc99 MDP (methylene diphos- Involvement of forearm especially involving periosteum phonate) bone scan was also performed which showed is seldom reported. Prompt diagnosis and adequate active bone involvement in left distal radial shaft. management is important for limb salvage and restora- tion of limb function. [1-3] An 11-year-old boy presented with painful mild swelling of left forearm for a month, with no significant past med- ical history or any history of trauma. -

Atypical Compound Nevus Arising in Mature Cystic Ovarian Teratoma
J Cutan Pathol 2005: 32: 71–123 Copyright # Blackwell Munksgaard 2005 Blackwell Munksgaard. Printed in Denmark Journal of Cutaneous Pathology Abstracts of the Papers Presented at the 41st Annual Meeting of The American Society of Dermatopathology Westin Copley Place Boston, Massachusetts, USA October 14–17, 2004 These abstracts were presented in oral or poster format at the 41st Annual Meeting of The American Society of Dermatopathology on October 14–17, 2004. They are listed on the following pages in alphabetical order by the first author’s last name. 71 Abstracts IN SITU HYBRIDIZATION IS A VALUABLE DIAGNOSTIC A 37-year-old woman with diagnosis of Sjogren’s syndrome (SS) TOOL IN CUTANEOUS DEEP FUNGAL INFECTIONS presented with asymptomatic non-palpable purpura of the lower J.J. Abbott1, K.L. Hamacher2,A.G.Bridges2 and I. Ahmed1,2 extremities. Biopsy of a purpuric macule revealed a perivascular Departments of Laboratory Medicine and Pathology1 and and focally nodular lymphocytic infiltrate with large numbers of Dermatology2, plasma cells, seemingly around eccrine glands. There was no vascu- litis. The histologic findings in the skin were strikingly similar to those Mayo Clinic and Mayo Foundation, Rochester, MN, USA of salivary, parotid, and other ‘‘secretory’’ glands affected in SS. The cutaneous manifestations of SS highlighted in textbooks include Dimorphic fungal infections (histoplasmosis, blastomycosis, coccidiomy- xerosis, annular erythema, small-vessel vasculitis, and pigmented cosis, and cryptococcosis) can occur in immunocompromised and purpura. This case illustrates that purpura in skin of patients with healthy individuals. Cutaneous involvement is often secondary and SS may be caused by a peri-eccrine plasma-rich infiltrate. -

Malignant Hidradenoma: a Report of Two Cases and Review of the Literature
ANTICANCER RESEARCH 26: 2217-2220 (2006) Malignant Hidradenoma: A Report of Two Cases and Review of the Literature I.E. LIAPAKIS1, D.P. KORKOLIS2, A. KOUTSOUMBI3, A. FIDA3, G. KOKKALIS1 and P.P. VASSILOPOULOS2 1Department of Plastic and Reconstructive Surgery, 2First Department of Surgical Oncology and 3Department of Surgical Pathology, Hellenic Anticancer Institute, "Saint Savvas" Hospital, Athens, Greece Abstract. Introduction: Malignant tumors of the sweat glands difficult (1). Clear cell hidradenoma is an extremely rare are very rare. Clear cell hidradenoma is a lesion with tumor with less than 50 cases reported (2, 3). histopathological features resembling those of eccrine poroma The cases of two patients, suffering from aggressive and eccrine spiradenoma. The biological behavior of the tumor dermal lesions invading the abdominal wall and the axillary is aggressive, with local recurrences reported in more than 50% region, are described here. Surgical resection and of the surgically-treated cases. Materials and Methods: Two histopathological examination ascertained the presence of patients are presented, the first with tumor in the right axillary malignant clear cell hidradenoma. In addition to these region, the second with a recurrent tumor of the abdominal cases, a review of the literature is also presented. wall. The first patient underwent wide excision with clear margins and axillary lymph node dissection and the second Case Reports patient underwent wide excision of the primary lesion and bilateral inguinal node dissection due to palpable nodes. Patient 1. Patient 1 was a 68-year-old Caucasian male who had Results: The patients had uneventful postoperative courses. No undergone excision of a rapidly growing, ulcerous lesion of the additional treatment was administered. -

Angiomyolipoma of the Cervix – Report of a Rare Entity
Internet Journal of Medical Update. 2017 July;12(2):13-15. doi: 10.4314/ijmu.v12i2.4 Internet Journal of Medical Update Journal home page: http://www.akspublication.com/ijmu Case Report Angiomyolipoma of the cervix – report of a rare entity N. Hariharanadha Sarmaᴪ1, Rama Srivastava2, Smriti Agnihotri3 1Consultant Pathologist, Department of Pathology, RDT Hospital, Bathalapalli, Andhra Pradesh, India 2Professor, Department of Pathology, SSR Medical College, Belle Rive, Mauritius 3Professor, Department of Pathology, American University of Antigua College of Medicine, Antigua & Barbuda, WI (Received 22 September 2017 and accepted 04 October 2017) ABSTRACT: Angiomyolipoma (AML) is a mesenchymal neoplasm seen usually in the kidney. Few cases of extra renal AML have been documented in various organs including the female genital tract, where the uterus is the most common site. To the best of our knowledge, only 4 cases of AML in the cervix have been reported in the literature. Association of AML with tuberous sclerosis is well known. Presently AML is included in the spectrum of disease entities called PEComa. We report a case of AML without tuberous sclerosis arising from the uterine cervix, which has to be differentiated from lipoleiomyoma. KEY WORDS: Angiomyolipoma; Uterine cervix; PEComas; Uterine tumor INTRODUCTIONV localization8, and mostly in females over 409. The occurrence of AML in the cervix without Angiomyolipoma (AML) occurs most frequently in concurrent incidence in the kidney is extremely the kidney, where it is closely related to tuberous rare, and only four cases have been reported in the sclerosis complex (TSC)1,2, occasionally in other scientific literature10. We are reporting a case of organs, most commonly the liver, but occurrence at uterine cervix AML without tuberous sclerosis other sites is extremely rare3. -

Soft Tissue Cytopathology: a Practical Approach Liron Pantanowitz, MD
4/1/2020 Soft Tissue Cytopathology: A Practical Approach Liron Pantanowitz, MD Department of Pathology University of Pittsburgh Medical Center [email protected] What does the clinician want to know? • Is the lesion of mesenchymal origin or not? • Is it begin or malignant? • If it is malignant: – Is it a small round cell tumor & if so what type? – Is this soft tissue neoplasm of low or high‐grade? Practical diagnostic categories used in soft tissue cytopathology 1 4/1/2020 Practical approach to interpret FNA of soft tissue lesions involves: 1. Predominant cell type present 2. Background pattern recognition Cell Type Stroma • Lipomatous • Myxoid • Spindle cells • Other • Giant cells • Round cells • Epithelioid • Pleomorphic Lipomatous Spindle cell Small round cell Fibrolipoma Leiomyosarcoma Ewing sarcoma Myxoid Epithelioid Pleomorphic Myxoid sarcoma Clear cell sarcoma Pleomorphic sarcoma 2 4/1/2020 CASE #1 • 45yr Man • Thigh mass (fatty) • CNB with TP (DQ stain) DQ Mag 20x ALT –Floret cells 3 4/1/2020 Adipocytic Lesions • Lipoma ‐ most common soft tissue neoplasm • Liposarcoma ‐ most common adult soft tissue sarcoma • Benign features: – Large, univacuolated adipocytes of uniform size – Small, bland nuclei without atypia • Malignant features: – Lipoblasts, pleomorphic giant cells or round cells – Vascular myxoid stroma • Pitfalls: Lipophages & pseudo‐lipoblasts • Fat easily destroyed (oil globules) & lost with preparation Lipoma & Variants . Angiolipoma (prominent vessels) . Myolipoma (smooth muscle) . Angiomyolipoma (vessels + smooth muscle) . Myelolipoma (hematopoietic elements) . Chondroid lipoma (chondromyxoid matrix) . Spindle cell lipoma (CD34+ spindle cells) . Pleomorphic lipoma . Intramuscular lipoma Lipoma 4 4/1/2020 Angiolipoma Myelolipoma Lipoblasts • Typically multivacuolated • Can be monovacuolated • Hyperchromatic nuclei • Irregular (scalloped) nuclei • Nucleoli not typically seen 5 4/1/2020 WD liposarcoma Layfield et al. -

PROPOSED REGULATION of the STATE BOARD of HEALTH LCB File No. R057-16
PROPOSED REGULATION OF THE STATE BOARD OF HEALTH LCB File No. R057-16 Section 1. Chapter 457 of NAC is hereby amended by adding thereto the following provision: 1. The Division may impose an administrative penalty of $5,000 against any person or organization who is responsible for reporting information on cancer who violates the provisions of NRS 457. 230 and 457.250. 2. The Division shall give notice in the manner set forth in NAC 439.345 before imposing any administrative penalty 3. Any person or organization upon whom the Division imposes an administrative penalty pursuant to this section may appeal the action pursuant to the procedures set forth in NAC 439.300 to 439. 395, inclusive. Section 2. NAC 457.010 is here by amended to read as follows: As used in NAC 457.010 to 457.150, inclusive, unless the context otherwise requires: 1. “Cancer” has the meaning ascribed to it in NRS 457.020. 2. “Division” means the Division of Public and Behavioral Health of the Department of Health and Human Services. 3. “Health care facility” has the meaning ascribed to it in NRS 457.020. 4. “[Malignant neoplasm” means a virulent or potentially virulent tumor, regardless of the tissue of origin. [4] “Medical laboratory” has the meaning ascribed to it in NRS 652.060. 5. “Neoplasm” means a virulent or potentially virulent tumor, regardless of the tissue of origin. 6. “[Physician] Provider of health care” means a [physician] provider of health care licensed pursuant to chapter [630 or 633] 629.031 of NRS. 7. “Registry” means the office in which the Chief Medical Officer conducts the program for reporting information on cancer and maintains records containing that information. -

Practical Veterinary Dermatopathology for the Small Animal Clinician
Dermatopathology_FINAL.qxd 2/14/06 11:19 AM Page i Practical Veterinary Dermatopathology for the Small Animal Clinician Sonya V. Bettenay, BVSc Dip. Ed, MACVSc, FACVSc CSU Diagnostic Laboratory Dermatopathology Service Department of Clinical Sciences Colorado State University Fort Collins, CO Ann M. Hargis, DVM, MS Diplomate, ACVP DermatoDiagnostics, Edmonds, WA Department of Comparative Medicine University of Washington, Seattle, WA Phoenix Central Laboratory Everett, WA Jackson,Wyoming www.veterinarywire.com Teton NewMedia Teton NewMedia 90 East Simpson, Suite 110 Jackson, WY 83001 © 2003 by Tenton NewMedia Exclusive worldwide distribution by CRC Press an imprint of Taylor & Francis Group, an Informa business Version Date: 20140103 International Standard Book Number-13: 978-1-4822-4128-0 (eBook - PDF) This book contains information obtained from authentic and highly regarded sources. While all reasonable efforts have been made to publish reliable data and information, neither the author[s] nor the publisher can accept any legal responsibility or liability for any errors or omissions that may be made. The publishers wish to make clear that any views or opinions expressed in this book by individual editors, authors or contributors are personal to them and do not necessarily reflect the views/opinions of the publishers. The information or guidance contained in this book is intended for use by medical, scientific or health-care professionals and is provided strictly as a supplement to the medical or other professional’s own judgement, their knowledge of the patient’s medical history, relevant manufacturer’s instructions and the appropriate best practice guide- lines. Because of the rapid advances in medical science, any information or advice on dosages, procedures or diagnoses should be independently verified. -

Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

Aderomyoma of the Common Bile Duct --Report of a Case
Yamanashl Med. J. 4 (2), 83"v87, 1989 Case Report AdeRomyoma of the Common Bile Duct --Report of a Case Yoshiro MATsuMoTe, Masatoshi MoGAKi, Hidehisa AoyAMA, Takayoshi SEKmAwA, Katsnhiko SuGAHARA, Koichi SuDAi), and Masayuki FuJiNo2) DePa,rt・ment of Surge7pu. i)DePartment of Pathology, 2)DePartment of lnte7"nal Medicine, YamanasJzi Medical Coglege, Tamaho, Nakakoma, Ya?nanashi 409-38, JaPan Abstract: Adenomyomas in the extrahepatic biie duc£ are extremely rare. In a 75-year- old male with acute cholangitis due to adenomyoma £erming a protruding lesion iR the terminal bile duct, pamacreatoduodenectomy was carried out, resulting complete cure, Key words: Adenomyoma of the common bile duct, Early bile dact cancer, Obstructive jaundice formed, aRd £rom the histologic examina- INTRODUCTION tion of the surgical specimen, adenomyoma Adenomyoma in the biliary ductal system of the common bile duct was confirmed. is most freguently fouRd in the gallbladder. Although beRign neoplasma o£ the bile The gallbiadder wall is more abuRdant in duct system are uncommon, the tumors are muscle fibers than is the wall o£ the bile clinically very important because they can duct. Adenomyoma in the gallbladder is cause obstructive jaundice4) and require knowlt to be closely re}ated to the forma- differentiation £rom eary cancer of the bile tion of gallstones. In other parts of the duct. biliary ductal system, kex4xeve]-, adeno- We report here the surgical results and myoma is very rarei)・2), although a few pathologic findings in a case of adeno- cases of a tumor arising from the papil}a myoma of the terminal bile duct. of Vater3) have beelt reported. -

Optimal Management of Common Acquired Melanocytic Nevi (Moles): Current Perspectives
Clinical, Cosmetic and Investigational Dermatology Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Optimal management of common acquired melanocytic nevi (moles): current perspectives Kabir Sardana Abstract: Although common acquired melanocytic nevi are largely benign, they are probably Payal Chakravarty one of the most common indications for cosmetic surgery encountered by dermatologists. With Khushbu Goel recent advances, noninvasive tools can largely determine the potential for malignancy, although they cannot supplant histology. Although surgical shave excision with its myriad modifications Department of Dermatology and STD, Maulana Azad Medical College and has been in vogue for decades, the lack of an adequate histological sample, the largely blind Lok Nayak Hospital, New Delhi, Delhi, nature of the procedure, and the possibility of recurrence are persisting issues. Pigment-specific India lasers were initially used in the Q-switched mode, which was based on the thermal relaxation time of the melanocyte (size 7 µm; 1 µsec), which is not the primary target in melanocytic nevus. The cluster of nevus cells (100 µm) probably lends itself to treatment with a millisecond laser rather than a nanosecond laser. Thus, normal mode pigment-specific lasers and pulsed ablative lasers (CO2/erbium [Er]:yttrium aluminum garnet [YAG]) are more suited to treat acquired melanocytic nevi. The complexities of treating this disorder can be overcome by following a structured approach by using lasers that achieve the appropriate depth to treat the three subtypes of nevi: junctional, compound, and dermal. Thus, junctional nevi respond to Q-switched/normal mode pigment lasers, where for the compound and dermal nevi, pulsed ablative laser (CO2/ Er:YAG) may be needed. -

TUMOR and STAGING DATA Primary Site Code
SECTION IV - TUMOR and STAGING DATA Primary Site Code NAACCR Version 11.1 field "Primary Site", Item 400, columns 291-294 It is unclear how the 2007 MP/H rules may alter rules for assigning the best Primary Site Formatted: Left Code to each primary. Continue to use the following rules until new rules are issued. Enter the code for the site of origin from the Topography section of ICD-O-3. [Note that ICD-O-2 code C14.1, laryngopharynx, should not be used for diagnoses made on or after January 1, 1995. "Laryngopharynx" became an equivalent term under C13.9 (hypopharynx, NOS) as of this diagnosis date. Code C14.1 is not an ICD-O-3 code.] Enter the site code that matches the narrative primary site indicated in the medical record, or the site code most appropriate for the case. Site codes are found in ICD-O-3's Numerical Lists - Topography section (pages 45-65) and in its Alphabetic Index (pages 105-218). In ICD-O-3 primary site codes consist of the letter "C" followed by two digits, a decimal point, and a third digit. "C" should be entered but the decimal point should not be entered. Example: The primary site is "cardia of stomach". Look this up in the Alphabetic Index of ICD-O-3 under "stomach" or "cardia", and the corresponding code "C16.0" is found. Enter C160. Most sites include a third digit of "8" to be used for single tumors that overlap the boundaries of two or more anatomically contiguous subsites and whose exact point of origin cannot be determined, unless the combination of sites is specifically indexed elsewhere.