Volunteer Handbook
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

America's Army Manual
America’s Army Game Manual Updated: 5/13/16 America’s Army 3 Game Manual AA3 Installation and Setup The America’s Army game provides civilians with an inside perspective and a virtual role in world's premier land force: the U.S. Army. The game is designed to provide an accurate portrayal of Soldier experiences across a number of occupations. In the game, players will explore progressive individual and collective training events within the game. Once they have successfully completed these events they will advance to multiplayer operations in small units. This chapter covers: AA3 System Requirements AA3 Downloading and Installation AA3 Player Account Setup AA3 Account Management Website AA3 System Requirements There are minimum system requirements for America’s Army. Please ensure your system meets these requirements, otherwise you may experience difficulties running the game. For better results, system specifications meeting or exceeding the recommended requirements are necessary. Note that each computer is different, and therefore performance may vary between systems. Minimum System Requirements Operating System (OS) Microsoft Windows XP (with Service Pack 2) Microsoft Windows Vista Processor (CPU) 3.0+ GHz Single Core CPU Memory (RAM) 1GB RAM (Minimum) Video Card Direct X 9.0c compliant Shader 3.0 enabled video card with 256MB RAM (NVIDIA 6600 or better/ATI X1300 or better) Sound Card Direct X 9.0c compliant sound card Hard Drive Space 5GB free hard drive space Network Broadband Internet Connection DVD-ROM 4x DVD-ROM (Disc Copies Only) -

NPRC) VIP List, 2009
Description of document: National Archives National Personnel Records Center (NPRC) VIP list, 2009 Requested date: December 2007 Released date: March 2008 Posted date: 04-January-2010 Source of document: National Personnel Records Center Military Personnel Records 9700 Page Avenue St. Louis, MO 63132-5100 Note: NPRC staff has compiled a list of prominent persons whose military records files they hold. They call this their VIP Listing. You can ask for a copy of any of these files simply by submitting a Freedom of Information Act request to the address above. The governmentattic.org web site (“the site”) is noncommercial and free to the public. The site and materials made available on the site, such as this file, are for reference only. The governmentattic.org web site and its principals have made every effort to make this information as complete and as accurate as possible, however, there may be mistakes and omissions, both typographical and in content. The governmentattic.org web site and its principals shall have neither liability nor responsibility to any person or entity with respect to any loss or damage caused, or alleged to have been caused, directly or indirectly, by the information provided on the governmentattic.org web site or in this file. The public records published on the site were obtained from government agencies using proper legal channels. Each document is identified as to the source. Any concerns about the contents of the site should be directed to the agency originating the document in question. GovernmentAttic.org is not responsible for the contents of documents published on the website. -

Stereophonics
Stereophonics: Gli Stereophonics hanno annunciato il loro più grande tour europeo, che partirà il 24 gennaio da Madrid e terminerà il 12 febbraio ad Amburgo con tappe in Spagna, Francia, Olanda, Germania, Italia, Svizzera e Lussemburgo. 22/10/2019 DEL PANORAMA ROCK MADE . 6 ALBUM DIRETTAMENTE ALLA #1 DELLE CLASSIFICHE IN U.K. CON OLTRE 10 MILIONI DI ALBUM VENDUTI IN TUTTO IL MONDO “KIND” È IL TITOLO DEL NUOVO ALBUM IN USCITA IL 25 OTTOBRE VIA WARNER ANNUNCIATO UN NUOVO TOUR CHE ARRIVERÀ IN ITALIA PER UNA DATA UNICA SABATO 8 FEBBRAIO @ MILANO LORENZINI DISTRICT Prezzi biglietti: Posto unico: 35,00 € + diritti di prevendita Biglietti in prevendita esclusiva per gli iscritti My Live Nation dalle ore 10:00 di giovedì 24 ottobre Biglietti disponibili su www.ticketmaster.it , www.ticketone.it e in tutti i punti vendita autorizzati dalle ore 10:00 di venerdì 25 ottobre L'organizzatore declina ogni responsabilità in caso di acquisto di biglietti fuori dai circuiti di biglietteria autorizzati non presenti nei nostri comunicati ufficiali Gli Stereophonics hanno annunciato il loro più grande tour europeo, che partirà il 24 gennaio da Madrid e terminerà il 12 febbraio ad Amburgo con tappe in Spagna, Francia, Olanda, Germania, Italia, Svizzera e Lussemburgo. Con oltre dieci milioni di copie di album venduti in tutto il mondo, gli Stereophonics sono una delle band gallesi di maggior successo di tutti i tempi. Word Gets Around è il titolo dell’album di debutto (1997) che ha conquistato la #6 posizione nelle classifiche britanniche, trainato dai singoli Local Boy in the Photograph, More Life in a Tramps Vest e A Thousand Trees. -

Kellogg Community College Nursing Student Clinical Orientation Manual A
KELLOGG COMMUNITY COLLEGE NURSING STUDENT CLINICAL ORIENTATION MANUAL 2016-2017 Page 1 of 154 Kellogg Community College Nursing Education Nursing Student Clinical Orientation Manual This manual was designed to assist the nursing student in becoming familiar with some of the policies and procedures that are used by the facilities that you will attend for clinical experience. Both hospitals and nursing homes function under standards which are set for them by accrediting bodies as well as state and federal government regulations. You need to familiarize yourself with these standards, policies, and procedures so that you can function as an informed student nurse while you are learning in a specific facility. It is required that staff in these facilities undergo review of this information every year and it will be required of you to do that as well. You will receive any updates that need to be added to this manual over the course of a school year and it should be part of the materials that you bring to orientation at all facilities that you attend. You will be required to obtain a new clinical orientation manual each school year and to take a competency test over the information contained in the manual. Upon completion of your orientation at each facility you will be asked by your clinical instructor to sign a form for the facility which will indicate that you have reviewed the contents of this manual and completed orientation to the clinical facility. You may also be asked to sign a confidentiality form for each facility that you are assigned a clinical rotation. -

Grunts Meet the 'Pocket Artilleryq (See Pages 6 and 7) Page 2, Thwaii !Hosier, Oct
&II Ali ailt I al Ria Grunts meet the 'pocket artilleryq (See pages 6 and 7) Page 2, thwaii !Hosier, Oct. 25, 1974 110111111111111111111111110111111111NINNISHINWWWW111111#111111111I WNW VMS SW W 3ii W Ni W MS W lii IiiIISIWIlt W WI Editorial IR ill IR 111 IR IM M LCPL. STEVEN LEWANDOWSKI SSGT. WILLIAM HILL it iit good times MAG-24 Back COMM. HQTRS to it SUFI. A di My To be a . 21 by. The parades oriOnal WI When 1 was a child in a small town seems to have passed me IR ambition was to success at whatever . Day honor veterans are few and far VI ; A# in southeast Missouri, Armistice to AA become a pafeont 0- I have to do. By A ranked second only to Christmas on the between and any gathering of Americans IN 1 . AM A logist. I took great MOS, a rit gala event scale. The day had all the on Monday now seems to be tinged with a A stock in the study... helicopter t4 trappings to make a child's eyes light up solemnity that just doesn't jibe with my ...we. IN IN of prehistoric life 4.!Po' mechanic, but I'm early memories. it it including bands, flags waving majestically A while I was in high i working as a IR in the breeze, fireworks and picnics at There are undoubtedly many WI school. After my ' logistics chief. which the kids ate too much candy and reasons for this and some of them are IN WI WI hitch in the Corps, When 1 first was it grown-ups drank too much beer. -

Southampton University's Finest Entertainment Publication 29Th September 2007
Southampton University's Finest Entertainment Publication 29th September 2007 We “Pull the Pin” on Stereophonics’ latest release 29th September 2007 A Word From Akon and Jackson? Helium voiced Rap superstar Akon has revealed that he is currently working with Michael Jackson, on a collaborative The Editor record. Hello and welcome to this year’s first However, Akon has kept the deatils close to his chest, issue of The Edge. Hope you all had refusing to disclose the specifics of the collaboration, a great summer and you’re all rested perhaps fearing the cold, swift sting of a slap round the face and ready for the crazy fun and games from the King of Pop’s signature gloved hand. However he of Freshers Week...not to mention the did say this; carnage, hangovers and flu... “He’s incredible. He’s a genius. Just to be in the same room Old readers of The Edge might notice (with him), I felt everything I wanted to accomplish in life something a bit different about the has been achieved. magazine, as we’re now colouring it in. We might have exploited this a “We’re about to shake the world up, man. You know how you be with somebody and you can’t even explain?”, he little in the first issue, so if the neon continued. glow of each page makes you want throw up in your frosties, let us know. “The way he thinks...some artists think regional, some think In fact if you have any comments or national, I was thinking international. -

This and That by Janine L
This and That By Janine L. Kock, Observer Editor and Publisher PAGE 4 -- THE OBSERVER -- THURSDAY, AUGUST 9, 2012 June 4, 2012 That date is another one that will definitely be engraved in the memories of our family forever. That was the date that my husband, having injured his hand badly enough over Memorial Week- end that he needed to visit the emergency room for stitches and a tetanus shot, visited the doctor’s office to have the stitches removed. While there, he mentioned to Dr. Ervelli that he had been experiencing some “balance issues” -- that the bottoms of his feet were numb and he had had some problems in the past couple days walking in a straight line. While Davey had failed to mention the balance problem to me, it immediately set in motion a series of events that continue today to get to the bottom of the problem. Dr. Ervelli immediately ordered a CAT scan of Davey’s head at the Carroll hospital to rule out a brain tumor, and, with that problem checked off the list, a visit to a neurologist in Ames was set up. After a consultation and a variety of tests, the doctors were a bit -- or a lot -- baffled. The symptoms, which continued to grow worse as June progressed, pointed toward a rare malady called Guillain-Barre Syndrome, although Davey wasn’t a textbook case, especially since many patients suffering from the syndrome end up hospitalized and on a ventilator within a few days because the rapidly-progressing symptoms render the patients’ respiratory systems and other bodily functions incapable of working on their own. -
Chartsplus Year-End 2007
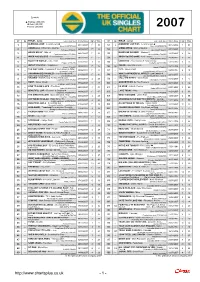
Symbols: p Platinum (600,000) ä Gold (400,000) è Silver (200,000) 2007 07 06 TITLE - Artist Label (Cat. No.) Entry Date High Wks 07 06 TITLE - Artist Label (Cat. No.) Entry Date High Wks ä 7 p 4 1 -- BLEEDING LOVE - Leona Lewis 03/11/2007 1 10 51 2 A MOMENT LIKE THIS - Leona Lewis 30/12/2006 1 31 Syco (88697175622) Syco (88697050872) è 10 2 -- UMBRELLA - Rihanna ft. Jay-Z 26/05/2007 1 33 52 -- GIMME MORE - Britney Spears 27/10/2007 3 11 Def Jam (1735491) Jive (88697186802) è 5 3 -- GRACE KELLY - Mika 20/01/2007 1 51 53 -- MAKES ME WONDER - Maroon 5 19/05/2007 2 20 Casablanca/Island (1721083) Octone/A&M (1734956) 4 -- WHEN YOU BELIEVE - Leon Jackson 29/12/2007 12 2 54 -- WHEN YOU'RE GONE - Avril Lavigne 28/04/2007 3 31 Syco (88697220162) RCA (88697119262) 5 -- RULE THE WORLD - Take That 27/10/2007 2 11 55 -- UNINVITED - Freemasons ft. Bailey Tzuke 13/10/2007 8 13 Polydor (1746285) Loaded (LOAD118CD) 6 -- ABOUT YOU NOW - Sugababes 29/09/2007 14 15 56 85 REHAB - Amy Winehouse 28/10/2006 7 63 Island (1748657) Island (1709535) 7 -- THE WAY I ARE - Timbaland ft. Keri Hilson [& DOE] 30/06/2007 12 28 57 -- 1973 - James Blunt 08/09/2007 4 18 Interscope (1742316) Custard/Atlantic (AT0285CDX) 8 -- (I'M GONNA BE) 500 MILES - The Proclaimers ft. 24/03/2007 13 14 58 -- WHAT A WONDERFUL WORLD - Eva Cassidy & 22/12/2007 1 3 Brian Potter & Andy Pipkin è EMI (COMICCD01) Katie Melua Blix Street/Dramatico (TD001) 9 -- VALERIE - Mark Ronson ft. -

Stereophonics Pull the Pin Mp3, Flac, Wma
Stereophonics Pull The Pin mp3, flac, wma DOWNLOAD LINKS (Clickable) Genre: Rock Album: Pull The Pin Country: Australia & New Zealand Released: 2007 Style: Alternative Rock MP3 version RAR size: 1641 mb FLAC version RAR size: 1143 mb WMA version RAR size: 1225 mb Rating: 4.3 Votes: 539 Other Formats: MPC AAC MOD MIDI APE XM AU Tracklist Hide Credits 1 Soldiers Make Good Targets 4:37 2 Pass The Buck 3:24 3 It Means Nothing 3:48 4 Bank Holiday Monday 3:14 5 Daisy Lane 3:38 6 Stone 4:17 7 My Friends 3:35 I Could Lose Ya 8 3:17 Lyrics By – Kelly JonesWritten-By – Javier Weyler, Richard Jones 9 Bright Red Star 3:39 10 Ladyluck 3:45 11 Crush 3:56 12 Drowning 5:08 Companies, etc. Phonographic Copyright (p) – V2 Music Ltd. Copyright (c) – V2 Music Ltd. Published By – Universal Music Publishing Credits Artwork By [Art Direction] – Graham Rounthwaite, Stereophonics Bass – Richard Jones Drums – Javier Weyler Engineer [Assistant] – Alex Dromgoole, Dario Dendi, Marco Migliari, Rowen Rossiter Mastered By – Ted Jensen Mixed By – Mark "Spike" Stent* Photography [Band] – Hans Peter Van Velthoven Photography [Cover] – Miles Aldridge Producer – Jim Lowe, Kelly Jones Vocals, Guitar – Kelly Jones Written-By – Kelly Jones Notes Special Indonesia Edition. Manufactured and Printed in Indonesia. Barcode and Other Identifiers Barcode: 6 02517 53043 0 Other versions Category Artist Title (Format) Label Category Country Year Pull The Pin V2, Nettwerk VVR1048562 Stereophonics VVR1048562 Europe 2007 (CD, Album) Music Group Pull The Pin 602517530430 Stereophonics V2 -
None of You Have Ever Lived in an Apartment Before and You Just Don't
volume 9 - issue 11 - tuesday, april 12, 2011 - uvm, burlington, vt uvm.edu/~watertwr - thewatertower.tumblr.com why furnishing your new pad is your first priority by dansuder Housewarming parties are Good Times. It’s a rule or law or theorem or something, but it’s pretty much always true. You and your friends have just moved into a new place, it’s asbestos-free and loaded with all the carbon-monoxide detectors money can buy. It still has that freshly cleaned carpet smell, which weeks-old pizza and unwashed socks will eventually overpow- er. But now, on this one Friday or Satur- day night, “Like a G6” pumps through the speakers, and the party begins. But sadly for everyone involved, this party is an exception to the Good Times Rule. Why? Because you are unprepared. You and your crew have a laptop and speakers, you’ve got your neighbor’s wifi, and you have beer. But none of you have ever lived in an apartment before and you just don’t know what it takes. The party crumbles under the weight of a million don’t-haves and should-have-boughts. It’s tragic, and it goes downhill right from the start. Here’s how it goes down. Guests ar- rive, and you immediately point them to the keg. And then to the empty cabinet where, ideally, in a perfect world (or just a normal one), there would be cups. But there are no cups. Strike one. And really, strike two and three also, because this party sucks and you look like an amateur. -
Castle Department Handbook
Castle Department Handbook Arcade, Redemption, Golf, Laser Tag, Cars, Boats, & Pizza Mesa Golfland 155 W. Hampton Ave. Mesa, AZ 85210 2 Congratulations and welcome to the Castle Department at Mesa Golfland SunSplash. This department has been around since Mesa Golfland first opened its doors in 1983. Many things have changed since the beginning but our objective remains the same; to provide excellent customer service to every guest that comes to the park. Our department is unique in that it encompasses several operational departments under the umbrella of the Castle Department. You will receive training on working each position in each of the sub-departments. This handbook is to serve as a supplement to the Employee Handbook and as an additional reference guide throughout your employment. Many policies and procedures are outlined here and you will be held accountable for knowing the information within these pages. The handbook is organized by department and not in any order that you will be trained in. Again, this is a reference guide. Read this handbook carefully as you will be tested on its contents as you receive training and you will be expected to know it. Good luck and happy reading. Further Requirements All Castle employees are required to obtain a Food Workers Permit from the Maricopa County Environmental Services Division. Study materials can be found online on the employee internet or on the County’s website. The test may also be taken online and the permit obtained the same way via the County’s website provided you have a web camera with your computer. -
REDACTED Final Porewater Sampling
825 NE Mul tnomah, 15 00 LCT Portland, OR 97232 phone (503) 8 13-5036 May 22, 2014 Via E-Mail Sean Sheldrake U.S. Environmental Protection Agency 1200 Sixth Avenue, Suite 900 M/S ECL-115 Seattle, WA 98101 [email protected] Re: Supplemental RI/FS Work at the River Mile 1 lE Project Area Portland Harbor Superfund Site (PHSS) Transmittal of the Final Porewater Sampling and Analysis Plan Dear Mr. Sheldrake: Attached for your review and approval is the Final Porewater Sampling and Analysis Plan (SAP) for the River Mile 1 lE Project Area. The Final SAP addresses the final round of comments that the U.S. Environmental Protection Agency (EPA) transmitted to the River Mile (RM) 1 lE on April 25, 2014. To assist with the review of the document, we have attached a copy of the comment table that EPA and the RMl lE Group have been exchanging that denotes (in red) where the SAP has been updated to address each ofEPA's comments. Please do not hesitate to contact me if you have any questions. I Jacqueline Thi ell Wetzsteon RMl lE Project Coordinator ec: River Mile 1 lE Respondents AOC Notice Recipients (Paragraph 97.c through m) Paul Fuglevand Porewater Sampling and Analysis Plan River Mile 11 East Willamette River Portland, Oregon May 2014 Prepared for RM11E GROUP Prepared by Smmc• & Engmnring for th• Environment DALTON OLMSTED FUGLEVAND DOF Water Solutions, Inc. This page intentionally left blank. Porewater Sampling and Analysis Plan Page ii River Mile 11 East - Portland, Oregon May 2014 Contents Section 1.