Community Palliative Care Service
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WTO GPA Statistical Report 2010-Revised 3Rd Version (
STATISTICS REPORTED UNDER ARTICLE XIX : 5 OF THE AGREEMENT ON GOVERNMENT PROCUREMENT OF THE WORLD TRADE ORGANIZATION, GENEVA PERIOD : 1.1.2010 - 31.12.2010 HONG KONG, CHINA ENTITY: HOSPITAL AUTHORITY Table of Content Part A - Reports Report No. 1 - Statistics on estimated number and value of contracts awarded for products and services, both equal or above and below the threshold value Report No. 2 - Statistics on total number and value of contracts awarded equal or above the threshold value, broken down by categories of products and services, under open, selective and limited tendering procedures Report No. 3 - Statistics on total number and value of contracts awarded under each of the cases of Article XV, paragraph 1 - limited tendering, broken down by categories of products and services Report No. 4 - Statistics on total number and value of contracts awarded for products and (where necessary) services under derogations to the Agreement Part B - Global Statistics and Details on Contracts Awarded for Products and Services to Individual Countries/Regions Part A Report No. 1 Article XIX Paragraph 5(a) Statistics on estimated number and value of contracts awarded, both equal or above and below the threshold value Tendering Procedures Equal or Above the Threshold Value Below the Threshold Value Total Construction Construction Construction Goods Services Services Goods Services Services Goods Services Services Open (No.) 99 12 - - - - 99 12 - (Value in 180,640.59 95,881.70 - - - - 180,640.59 95,881.70 - '000 SDR) Selective(No.) 1 - 2 - - - 1 - 2 (Value in 1,269.54 - 31,229.86 - - - 1,269.54 - 31,229.86 '000 SDR) Limited (No.) 76 1 - - - - 76 1 - (Value in 186,083.54 745.89 - - - - 186,083.54 745.89 - '000 SDR) Grand Total :(No.) 176 13 2 - - - 176 13 2 (Value in 367,993.67 96,627.59 31,229.86 - - - 367,993.67 96,627.59 31,229.86 '000 SDR) Notes : There may be a slight discrepancy between the sum of individual items and the total as shown in the tables owing to rounding. -

Hospital Authority Annual Plan 2005/06 I
HOSPITAL AUTHORITY ANNUAL PLAN 2005/06 Table of Contents EXECUTIVE SUMMARY 1 PLANNING BACKGROUND 1. Introduction 10 2. Review of Progress 13 3. Planning Environment 14 4. Budget Allocation 17 MAJOR DIRECTIONS AND PROGRAMME INITIATIVES FOR 2005/06 HA ANNUAL PLAN 5. Major Directions for HA Annual Plan 2005/06 20 6. Improving Population Health 22 7. Enhancing Organisational Performance 25 8. Enhancing Healthcare System Sustainability 30 9. Improving Service Quality and Clinical Governance 34 10. Building Human Resources Capability 40 CLUSTER PLANS 11. Hong Kong East Cluster 45 12. Hong Kong West Cluster 50 13. Kowloon East Cluster 54 14. Kowloon Central Cluster 58 15. Kowloon West Cluster 62 16. New Territories East Cluster 66 17. New Territories West Cluster 70 Hospital Authority Annual Plan 2005/06 i Table of Contents APPENDICES Appendix 1: List of Public Hospitals and Institutions 74 Appendix 2: List of Ambulatory Care Facilities 75 Appendix 3: Background Information on Hospital Authority 79 Appendix 4: Statistics of the Controlling Officer’s Report 81 ii Hospital Authority Annual Plan 2005/06 Executive Summary OVERVIEW 1. The Hospital Authority (HA) is responsible for delivering a comprehensive range of hospital, outpatient and community-based services through its network of healthcare facilities. As part of its commitment to enhance accountability and transparency to the community, it has been publishing its Annual Plan since 1992/93, which provides a structured mechanism for the organisation to turn its corporate vision and directions into strategies, goals and operational targets. 2. There are a number of major changes in the external and internal environment of HA that shape the major directions adopted and presented in this Annual Plan for 2005/06: (a) Key people changes after the SARS epidemic could have important bearings on the healthcare environment as well as the work of HA. -

Our Ref : TP/VAL/Q575/A
For Discussion WCDC Paper On 09.01.2018 No.: 2/2018 Proposed Amendments to the Road Improvement Works at Kennedy Road, and the Junction of Queen’s Road East and Kennedy Road, Wan Chai PURPOSE 1. This paper aims to seek Members’ views on the proposed amendments to the Road Improvement Works (“RIW”) following the presentation by the representatives of Hopewell Holdings Limited to Wan Chai District Council on 10 January 2017 regarding the latest development scheme of Hopewell Centre II and the associated RIW amendments. BACKGROUND 2. The original RIW was gazetted in April 2009 and authorized by the Chief Executive in Council in July 2010. The RIW comprises three parts; namely road widening at Kennedy Road, road widening at the junction of Queen’s Road East and Kennedy Road, and road widening at the junction of Spring Garden Lane and Queen’s Road East Note 1. Please refer to the Key Plan in 2009 Gazette at Appendix 1. 3. In order to preserve more trees, during the detailed design of the road work, Hopewell Holdings Limited proposed to amend the RIW at Kennedy Road and at the junction of Queen’s Road East and Kennedy Road. The proposed amendments to the RIW have been submitted to the relevant Government departments for comment and are considered acceptable in principle. On 11 August 2017, the planning application (No. A/H5/408) of the latest development scheme of Hopewell Centre II was approved with conditions by the Metro Planning Committee of the Town Planning Board including an approval condition on the design and implementation of the related RIW. -

Hospital Authority
HOSPITAL AUTHORITY New Territories West Cluster Medical Report and Patient Information Application Form (for Castle Peak Hospital and Siu Lam Hospital) Note : • Please read the information leaflet carefully before completing this form (Please return this form to the medical report section after payment is done) . • Each application is for One Hospital ONLY, please “” the suitable box below. To : Medical Report Section (Please “” ONE suitable hospital ONLY) Tuen Mun Hospital (including General Outpatient Clinics under TMH) Pok Oi Hospital Castle Peak Hospital Siu Lam Hospital Tin Shui Wai Hospital A: Patient’s Particulars (This section must be completed) For Account Use Only Name: (English) Hospital: * TMH / POH / CPH / SLH / TSWH (Chinese) No. of report or certificate required HK$ * HKID / Passport No.: Sex: * M / F Date of Birth: Charge: $895 × Address: $230 × Total Charge: Receipt No.: Tel. No.:(Day Time) Other Tel. No.: Date: B. Information Requested (Please ‘✓’ the suitable box) B1. Nature of Request ☐ Medical Report ($895 - $3,580) Other documents ($230 each): ☐ Confirmation of granted sick leave (no indicating of diagnosis) ☐ Certified true copy ☐ Confirmation of hospital fee (please submit to Account office) ☐ Others – please specify : _____________ B2. Period of information requested Period : From to Specialty: _____________________________________ Request Form attached (Please indicate the type of request form): ______________________________________ (if doctor completes the attached request form, then no additional medical -

For Basic Surgical Trainee Endorsed by HKICBSC Council on 27 May 2016 1
Rules & Regulations For Basic Surgical Trainee_ Endorsed by HKICBSC Council on 27 May 2016 1 HONG KONG INTERCOLLEGIATE BOARD OF SURGICAL COLLEGES Rules & Regulations For Basic Surgical Trainee For general enquiry, please contact HKICBSC Secretariat: Tel: (852) 2871 8799 Fax: (852) 2515 3198 Email: [email protected] Relevant forms are available at the website of CSHK at http://www.cshk.org. 20210226 Rules & Regulations For Basic Surgical Trainee_ Endorsed by HKICBSC Council on 27 May 2016 2 HONG KONG INTERCOLLEGIATE BOARD OF SURGICAL COLLEGES Rules & Regulations REGISTRATION Basic Surgical Training takes no less than two years after internship. In this period, Basic Trainees must register with one of the four Surgical Colleges of Hong Kong and the Hong Kong Intercollegiate Board of Surgical Colleges (HKICBSC). HKICBSC composes of the College of Surgeons of Hong Kong (CSHK), the Hong Kong College of Emergency Medicine (HKCEM), the Hong Kong College of Orthopaedic Surgeons (HKCOS) and the Hong Kong College of Otorhinolaryngologists (HKCORL). Basic Training is under the auspices of HKICBSC. A Register of Basic Surgical Trainees is maintained at CSHK. ELIGIBILIY FOR ADMISSION TO BASIC SURGICAL TRAINING To enter the Basic Surgical Training Programme of HKICBSC in Hong Kong, applicants must fulfill the following requirements: One must be fully registered with the Medical Council of Hong Kong. One must obtain a training post from the approved hospitals or institutions in Hong Kong. Please refer to the “Eligibility for Basic Surgical Training” for further details. SUBMISSION DEADLINE All trainees who decide to enroll into Basic Training Programme under HKICBSC must register with HKICBSC within the first month of training. -
BMJ Open Is Committed to Open Peer Review. As Part of This Commitment We Make the Peer Review History of Every Article We Publish Publicly Available
BMJ Open: first published as 10.1136/bmjopen-2018-023070 on 15 October 2018. Downloaded from BMJ Open is committed to open peer review. As part of this commitment we make the peer review history of every article we publish publicly available. When an article is published we post the peer reviewers’ comments and the authors’ responses online. We also post the versions of the paper that were used during peer review. These are the versions that the peer review comments apply to. The versions of the paper that follow are the versions that were submitted during the peer review process. They are not the versions of record or the final published versions. They should not be cited or distributed as the published version of this manuscript. BMJ Open is an open access journal and the full, final, typeset and author-corrected version of record of the manuscript is available on our site with no access controls, subscription charges or pay-per-view fees (http://bmjopen.bmj.com). If you have any questions on BMJ Open’s open peer review process please email [email protected] http://bmjopen.bmj.com/ on September 29, 2021 by guest. Protected copyright. BMJ Open BMJ Open: first published as 10.1136/bmjopen-2018-023070 on 15 October 2018. Downloaded from 10-year Risk Prediction Models of Complications and Mortality of Diabetes Mellitus in Chinese Patients in Primary Care in Hong Kong study protocol ForJournal: peerBMJ Open review only Manuscript ID bmjopen-2018-023070 Article Type: Protocol Date Submitted by the Author: 19-Mar-2018 Complete List of Authors: -

Kowloon West Cluster 九龍西聯網
Kowloon West Cluster 九龍西聯網 Section 1 : Selected Statistics Kowloon West Cluster 第一章 : 選定的統計數字 九龍西聯網 Service Capacity as at 31 March 2018 截至2018年3月31日的服務容量 No. of hospital beds 醫院病床數目 4 707 No. of psychiatric day places 精衶科日間醫院名額 303 No. of geriatric day places# 老人科日間醫院名額# 160 Service Throughputs in 2017-18 2017-18年度服務量 Inpatient and day No. of discharges and deaths 出院人次及死亡人數 297 075 inpatient services No. of live births 活產嬰兒數目 4 623 住院及日間住院服務 No. of allied health attendances 專職醫療就診人次 860 108 No. of accident and emergency attendances 急症室就診人次 483 885 No. of specialist outpatient (clinical) attendances 專科門診(臨床)就診人次 1 345 950 Ambulatory Services No. of primary care attendances 基層醫療就診人次 1 104 472 日間服務 No. of allied health attendances 專職醫療就診人次 382 862 No. of geriatric day attendances# 老人科日間醫院就診人次# 35 844 No. of psychiatric day attendances 精神科日間醫院就診人次 66 607 No. of home visits by community nurses 社康護士家訪次數 156 748 Outreach Services No. of allied health attendances 專職醫療就診人次 4 473 外展服務 No. of geriatric outreach attendances 接受老人科外展服務人次 130 668 No. of psychiatric outreach attendances 接受精神科外展服務人次 91 857 Other Services No. of radiodiagnostic attendances 放射診斷就診人次 680 025 其他服務 No. of operations done inside operating theatres 在手術室內進行的手術數目 27 156 # : Figures also include places / attendances under Integrated Discharge Support Programme for Elderly Patients (IDSP). # : 數字也包括參與離院長者綜合支援計劃的醫院名額 / 就診人次。 As at 31 Mar 2018 Hospital / Institution Specialist Outpatient Clinic General Outpatient Clinic 截至2018年3月31日 醫院 / 機構 專科門診診所 普通科門診診所 Number 數目 5 8 16 ❶ Caritas -

E-Newsletter
E-Newsletter INAUGURATION ISSUE 2016 With the support of The Hong Kong Jockey Club Charities Trust, a three-year initiative, Jockey Club End-of-Life Community Care (JCECC) Project, was launched in 2015. The project aims at improving the quality of end-of-life care, enhancing the capacity of service providers and raising public awareness. FEATURE On February 25, 2016, The JCECC Project, together with Hospital Authority and Hong Kong Society of Palliative Medicine, organised a Symposium on Collaboration and Communications in Health and Social Care for End-of-Life Care. The Symposium featured three knowledgeable speakers including Professor Ilora Finlay from University of Cardiff, Mr. Richard Yuen from Food and Health Bureau and Professor Cecilia Chan from the JCECC Project. In Hong Kong, the proportion of deaths of people aged 65 or over has increased from 67.2% (in 1991) to 78.4% (in 2011), amounting to a 73% increase in actual deaths. In the same period, the overall number of deaths also increased; therefore, the demand for end-of-life care has grown tremendously. Despite that, the development of end-of-life care in Hong Kong has been below average. In the 2015 Quality of Death Index, Hong Kong was ranked only 22nd out of 80 regions, behind other developed Asian regions like Taiwan, Singapore, Japan and South Korea. The United Kingdom ranked 1st in the index and there are a lot of experience that can be learnt from the UK on end-of-life care in terms of systems, infrastructures and community education. Professor Finlay, The Baroness Finlay of Llandaff and Professor of Palliative Medicine in Cardiff University, with Mr. -
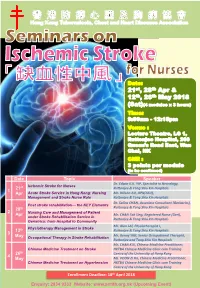
21St, 28Th Apr & 12Th, 26Th May 2018 (Sat)(4 Modules X 3 Hours)
Date: 21st, 28th Apr & 12th, 26th May 2018 (Sat)(4 modules x 3 hours) Time: 9:00am - 12:15pm Venue : Lecture Theatre, LG 1, Ruttonjee Hospital, 266 Queen’s Road East, Wan Chai, HK CNE : 3 points per module (to be confirmed) Date Topic Speaker Dr. Edwin K.K. YIP, Specialist in Neurology, Ischemic Stroke for Nurses 21st Ruttonjee & Tang Shiu Kin Hospitals 1 Apr Acute Stroke Service in Hong Kong: Nursing Mr. Wilson AU, APN(ASU), Management and Stroke Nurse Role Ruttonjee & Tang Shiu Kin Hospitals Dr. Selina CHAN, Associate Consultant (Geriatrics), Post stroke rehabilitation— the KEY Elements 28th Ruttonjee & Tang Shiu Kin Hospitals 2 Nursing Care and Management of Patient Apr Mr. CHAN Tak Sing, Registered Nurse (Geri), under Stroke Rehabilitation Service in Ruttonjee & Tang Shiu Kin Hospitals Geriatrics: from Hospital to Community Mr. Alan LAI, Physiotherapist I, Physiotherapy Management in Stroke 12th Ruttonjee & Tang Shiu Kin Hospitals 3 Mr. Benny YIM, Senior Occupational Therapist, May Occupational Therapy in Stroke Rehabilitation Ruttonjee and Tang Shiu Kin Hospitals Mr. CHAN KUI, Chinese Medicine Practitioner, Chinese Medicine Treatment on Stroke HKTBA Chinese Medicine Clinic cum Training 26th Centre of the University of Hong Kong 4 May Ms. POON Zi Ha, Chinese Medicine Practitioner, Chinese Medicine Treatment on Hypertension HKTBA Chinese Medicine Clinic cum Training Centre of the University of Hong Kong Enrollment Deadline: 18th April 2018 Enquiry: 2834 9333 Website: www.antitb.org.hk (Upcoming Event) Seminars on “Ischemic Stroke” for Nurses Objectives a) To strengthen, update and develop knowledge of nurses on the topic of endocrine system. b) To enhance the skills and technique in daily practice. -
Service Setting Briefing Social Work in Medical Setting (MSS& MSP) Rundown
Service Setting Briefing Social Work in Medical Setting (MSS& MSP) Rundown 3:30-4:30 • Mutual Introduction • Brief Overview of Social Work Services in Hong Kong Medical Settings • Exercise 4:30-4:45 • Do’s and don’ts in medical settings 4:45-5:00 • Useful Resources • Related Training and Orientation • Mid-Placement Sharing Where are you posted? • Adolescent Medical Centre, QEH • Patient Resource • Ap Lei Chau Clinic Centre, QEH • CancerCare & Support, • MSSU (HA), KH (+HK QMH Eye Hospital) • Community & Patient • MSSU (Psy.), PYH Resource Department, • MSSU (Psy.), YFSPC PYH • Health Resource Centre, YCH Where are you posted? Implication? Clustering of HA Service Hong Kong West Cluster • Grantham Hospital • MacLehose Medical Rehabilitation Centre • Queen Mary Hospital • The Duchess of Kent Children's Hospital at Sandy Bay • Tsan Yuk Hospital • Tung Wah Group of Hospitals Fung Yiu King Hospital • Tung Wah Hospital • Why should I be bothered by things happening in HA? • I’m a social worker doing social work in a medical setting only HA Strategic Plan 2017-2022 • Provide patient-centred care: ensuring patients have timely access to high quality and responsive services which place patients firmly at the heart of their care 1. Improving Service Quality 2. Optimizing Demand Management Hospital/Clinic = Secondary Setting => Meaning to me?? Improving Service Quality • Promote day services to reduce reliance on inpatient care • Strengthening service coordination and collaboration through the development of cluster/network-based service • Enhancing community-based care • Promote partnership with patients by empowering patients for self-care, engaging patients in shared decision-making about their care… Optimizing Demand Management • Raise the capacity of priority services of HA, particularly for high demand services having regard to the projected demand arising from a growing and ageing population… • Share out the demand with community partners, such as through public-private partnerships C.R.1 24/8/2018 Pt’s e. -

From 1.1.2021 Onwards
Updated as of 30 June 2021 Hong Kong College of Radiologists Page 1 CME/ CPD Application (Association/Personal) 1.1.2021-30.6.2021 Ref. No. HKAM Ref. Association Conference / Lecture Date / Duration Application Points Association / No. Date Personal Application 2021-475 AA02635 CME Committee "It's not COPD, but Heart Failure" - From 18.5.21 19.4.21 1 (Cat. B) Asso Association of Private Medical Prevention to Management (Online) 7-8pm Specialists of Hong Kong 2021-319 AA02466 Centre for Medical Ethics and Law (Webinar) Gross Negligence Manslaughter: 9.4.21 10.3.21 2 (Cat. B) Asso The University of Hong Kong Should it apply to healthcare practitioners? 4-6pm (Online) 2021-463 AA02611 The Federation of Medical Societies of [IBD Intensive Course Lecture 3] Anti-TNF 4.5.21 13.4.21 1 (Cat. B) Asso Hong Kong Therapy in Inflammatory Bowel Disease: 8-9pm Past, Present and Future (Online) 2021-579 AA02747 The Federation of Medical Societies of [IBD Intensive Course Lecture 5] 8.6.21 17.5.21 1 (Cat. B) Asso Hong Kong Management of Acute Severe UC: Pearls and 7-8pm Pitfalls (Online) 2021-635 AA02805 The Federation of Medical Societies of [IBD Intensive Course Lecture 6] Surgical 22.6.21 4.6.21 1 (Cat. B) Asso Hong Kong Management of Ulcerative Colitis: What 7-8pm Physicians Need to Know (Online) 2021-685 AA02867 The Federation of Medical Societies of [IBD Intensive Course Lecture 7] Perianal and 13.7.21 16.6.21 1 (Cat. B) Asso Hong Kong Fistulizing Crohn’s Disease: How Do I Tackle 9-10pm Them (Online) 2021-380 AA02529 The Federation of Medical Societies of [IBD Intensive Course: Lecture 2] Non- 23.4.21 25.3.21 1 (Cat. -

Report of the Steering Committee on Review of Hospital Authority
Report of the Steering Committee on Review of Hospital Authority July 2015 CONTENTS Glossary .................................................................................................................. iii Executive Summary ................................................................................................ v Chapter 1 Introduction ...................................................................................... 1 Chapter 2 Work of the Steering Committee ...................................................... 6 Chapter 3 Major Challenges Facing the Hospital Authority ............................ 9 Chapter 4 Management and Organisation Structure ....................................... 13 Chapter 5 Resource Management ................................................................... 26 Chapter 6 Staff Management .......................................................................... 42 Chapter 7 Cost Effectiveness and Service Management ................................ 59 Chapter 8 Overall Management and Control .................................................. 87 Chapter 9 Conclusion ...................................................................................... 96 Annex 1 Membership of the Steering Committee on Review of Hospital Authority ....................................................................................... 102 Annex 2 Report of the Public Engagement Programme ............................. 103 Annex 3 Clustering of Hospitals and Institutions ......................................