Volume C: Addiction Medications and Special Populations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diazepam - Alcohol Withdrawal
Diazepam - alcohol withdrawal Why have I been prescribed diazepam? If a person stops drinking alcohol after a time of drinking too much they can experience withdrawal effects. These include “the shakes”, sweating, having fits, seeing things which are not there (hallucinations) and feeling anxious and low in mood. They can feel wound up and find it difficult to sleep. These withdrawal effects can be very uncomfortable and in extreme cases can be dangerous if they persist into “DTs” (delirium tremens). Diazepam is used to help reduce these withdrawal symptoms. It relieves anxiety and tension and aids sleep. Diazepam can also prevent fits. It controls the withdrawal symptoms until the body is free of alcohol and has settled down. This usually takes three to seven days from the time you stop drinking. What exactly is diazepam? Diazepam is a benzodiazepine. This group of medicines is also called anxiolytics or minor tranquillisers. Diazepam has many uses. It can be used to reduce symptoms of anxiety and insomnia, as well as to help people come off alcohol. Diazepam should only be prescribed and taken as a short course. Is diazepam safe to take? Diazepam is safe to take for a short period of time, but it doesn’t suit everyone. Below are a few conditions where diazepam may be less suitable. If any of these apply to you please tell your doctor or key-worker. If you have depression or a mental illness If you have lung disease or breathing problems, or suffer from liver or kidney trouble If you take any other medicines or drugs, including those on prescription and bought from a chemist If you take illicit drugs bought “on the street” If you are pregnant or breast-feeding What is the usual dose of diazepam? The dose of diazepam will usually be started at 10-20mg four times a day. -
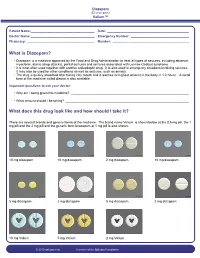
What Is Diazepam?
Diazepam (Di-a-ze-pam) Valium™ Patient Name: ___________________________________ Date: _____________________________________________ Doctor Name: ___________________________________ Emergency Number: ________________________________ Pharmacy: _____________________________________ Number: __________________________________________ What is Diazepam? • Diazepam is a medicine approved by the Food and Drug Administration to treat all types of seizures, including absence, myoclonic, atonic (drop attacks), partial seizures and seizures associated with Lennox-Gastaut syndrome. • It is most often used together with another antiepileptic drug. It is also used in emergency situations involving seizures. It may also be used for other conditions as well as seizures, such as anxiety. • The drug is quickly absorbed after taking it by mouth and it reaches its highest amount in the body in 1-2 hours. A rectal form of the medicine called diastat is also available. Important questions to ask your doctor: • Why am I being given this medicine? _________________________________________________________________ • What amount should I be taking? ____________________________________________________________________ What does this drug look like and how should I take it? There are several brands and generic forms of the medicine. The brand name Valium is shown below at the 0.5 mg pill, the 1 mg pill and the 2 mg pill and the generic form lorazepam at 1 mg pill is also shown. 10 mg diazepam 10 mg diazepam 2 mg diazepam 10 mg diazepam 5 mg diazepam 2 mg diazepam 5 mg diazepam 2 mg diazepam 10 mg Valium 5 mg Valium 2 mg Valium © 2010 epilepsy.com A service of the Epilepsy Foundation Diazepam (Di-a-ze-pam) Valium™ Frequently Asked Questions: How do I take Diazepam? To use the tablet form: chew tablets and swallow or swallow the tablet whole. -

Comparison of Short-And Long-Acting Benzodiazepine-Receptor Agonists
J Pharmacol Sci 107, 277 – 284 (2008)3 Journal of Pharmacological Sciences ©2008 The Japanese Pharmacological Society Full Paper Comparison of Short- and Long-Acting Benzodiazepine-Receptor Agonists With Different Receptor Selectivity on Motor Coordination and Muscle Relaxation Following Thiopental-Induced Anesthesia in Mice Mamoru Tanaka1, Katsuya Suemaru1,2,*, Shinichi Watanabe1, Ranji Cui2, Bingjin Li2, and Hiroaki Araki1,2 1Division of Pharmacy, Ehime University Hospital, Shitsukawa, Toon, Ehime 791-0295, Japan 2Department of Clinical Pharmacology and Pharmacy, Neuroscience, Ehime University Graduate School of Medicine, Shitsukawa, Toon, Ehime 791-0295, Japan Received November 7, 2007; Accepted May 15, 2008 Abstract. In this study, we compared the effects of Type I benzodiazepine receptor–selective agonists (zolpidem, quazepam) and Type I/II non-selective agonists (zopiclone, triazolam, nitrazepam) with either an ultra-short action (zolpidem, zopiclone, triazolam) or long action (quazepam, nitrazepam) on motor coordination (rota-rod test) and muscle relaxation (traction test) following the recovery from thiopental-induced anesthesia (20 mg/kg) in ddY mice. Zolpidem (3 mg/kg), zopiclone (6 mg/kg), and triazolam (0.3 mg/kg) similarly caused an approximately 2-fold prolongation of the thiopental-induced anesthesia. Nitrazepam (1 mg/kg) and quazepam (3 mg/kg) showed a 6- or 10-fold prolongation of the anesthesia, respectively. Zolpidem and zopiclone had no effect on the rota-rod and traction test. Moreover, zolpidem did not affect motor coordination and caused no muscle relaxation following the recovery from the thiopental-induced anesthesia. However, zopiclone significantly impaired the motor coordination at the beginning of the recovery. Triazolam significantly impaired the motor coordination and muscle relaxant activity by itself, and these impairments were markedly exacerbated after the recovery from anesthesia. -

Red with Nitrazepam and Placebo in Acute Emergency Driving Situations and in Monotonous Simulated Driving
109 A 1986 The Carry-over Effects of Triazolam Compa- red with Nitrazepam and Placebo in Acute Emergency Driving Situations and in Mono- tonous Simulated Driving Hans Laurell and Jan Törnroos Reprint from Acta Pharmacologica et toxicologica 1986 v Väg06/7 Efi/( Statens väg- och trafikinstitut (VTI) * 581 01 Linköping [St]tlltet Swedish Road and Traffic Research Institute * S-581 01 Linköping Sweden Acta pharmacol. et toxicol. 1986, 58, 182186. From the National Swedish Road and Traffic Research Institute, (V.T.I.), S-58 101 Linköping, Sweden The Carry-over Effects of Triazolam Compared with Nitrazepam and Placebo in Acute Emergency Driving Situations and in Monotonous Simulated Driving Hans Laurell and Jan Törnros (Received October 9, 1985; Accepted January 9, 1986) Abstract: Eighteen healthy volunteers of both sexes, aged 2034, were tested in the morning while undertaking real car driving avoidance manoeuvres and during monotonous simulated driving after 1 and 3 nights of medication with triazolam 0.25 mg, nitrazepam 5 mg or placebo. The study was a double-blind, randomized, cross-over study, where a minimum of 7 days wash-out separated the 3 treatment periods. Nitrazepam was found to impair performance in the simulated task after 1 but not after 3 nights of medication. Performance in the triazolam condition was not signicantly different from the other conditions on this task on either day. However, after one night of medication triazolam tended to score worse than placebo but better than nitrazepam. In real car driving a tendency was noted for nitrazepam to score worst, whereas the difference between placebo and triazolam was hardly noticeable. -

Calculating Equivalent Doses of Oral Benzodiazepines
Calculating equivalent doses of oral benzodiazepines Background Benzodiazepines are the most commonly used anxiolytics and hypnotics (1). There are major differences in potency between different benzodiazepines and this difference in potency is important when switching from one benzodiazepine to another (2). Benzodiazepines also differ markedly in the speed in which they are metabolised and eliminated. With repeated daily dosing accumulation occurs and high concentrations can build up in the body (mainly in fatty tissues) (2). The degree of sedation that they induce also varies, making it difficult to determine exact equivalents (3). Answer Advice on benzodiazepine conversion NB: Before using Table 1, read the notes below and the Limitations statement at the end of this document. Switching benzodiazepines may be advantageous for a variety of reasons, e.g. to a drug with a different half-life pre-discontinuation (4) or in the event of non-availability of a specific benzodiazepine. With relatively short-acting benzodiazepines such as alprazolam and lorazepam, it is not possible to achieve a smooth decline in blood and tissue concentrations during benzodiazepine withdrawal. These drugs are eliminated fairly rapidly with the result that concentrations fluctuate with peaks and troughs between each dose. It is necessary to take the tablets several times a day and many people experience a "mini-withdrawal", sometimes a craving, between each dose. For people withdrawing from these potent, short-acting drugs it has been advised that they switch to an equivalent dose of a benzodiazepine with a long half life such as diazepam (5). Diazepam is available as 2mg tablets which can be halved to give 1mg doses. -

Drugs of Abuse: Benzodiazepines
Drugs of Abuse: Benzodiazepines What are Benzodiazepines? Benzodiazepines are central nervous system depressants that produce sedation, induce sleep, relieve anxiety and muscle spasms, and prevent seizures. What is their origin? Benzodiazepines are only legally available through prescription. Many abusers maintain their drug supply by getting prescriptions from several doctors, forging prescriptions, or buying them illicitly. Alprazolam and diazepam are the two most frequently encountered benzodiazepines on the illicit market. Benzodiazepines are What are common street names? depressants legally available Common street names include Benzos and Downers. through prescription. Abuse is associated with What do they look like? adolescents and young The most common benzodiazepines are the prescription drugs ® ® ® ® ® adults who take the drug Valium , Xanax , Halcion , Ativan , and Klonopin . Tolerance can orally or crush it up and develop, although at variable rates and to different degrees. short it to get high. Shorter-acting benzodiazepines used to manage insomnia include estazolam (ProSom®), flurazepam (Dalmane®), temazepam (Restoril®), Benzodiazepines slow down and triazolam (Halcion®). Midazolam (Versed®), a short-acting the central nervous system. benzodiazepine, is utilized for sedation, anxiety, and amnesia in critical Overdose effects include care settings and prior to anesthesia. It is available in the United States shallow respiration, clammy as an injectable preparation and as a syrup (primarily for pediatric skin, dilated pupils, weak patients). and rapid pulse, coma, and possible death. Benzodiazepines with a longer duration of action are utilized to treat insomnia in patients with daytime anxiety. These benzodiazepines include alprazolam (Xanax®), chlordiazepoxide (Librium®), clorazepate (Tranxene®), diazepam (Valium®), halazepam (Paxipam®), lorzepam (Ativan®), oxazepam (Serax®), prazepam (Centrax®), and quazepam (Doral®). -

Intermittent Treatment of Febrile Convulsions with Nitrazepam Michel Vanasse, Pierre Masson, Guy Geoffroy, Albert Larbrisseau and Pierre C
LE JOURNAL CANADIEN DES SCIENCES NEUROLOGIQUES Intermittent Treatment of Febrile Convulsions with Nitrazepam Michel Vanasse, Pierre Masson, Guy Geoffroy, Albert Larbrisseau and Pierre C. David ABSTRACT: Intermittent oral or rectal administration of diazepam for the prophylactic treatment of febriie convulsions has given results comparable to the continuous use of phenobarbital while limiting side effects and risks of toxicity. Since we believe that nitrazepam is a better anticonvulsant than diazepam, we performed a study to evaluate the effectiveness of this medication in the prophylactic treatment of febrile convulsions. Nitrazepam was given only when the children had fever and almost exclusively in children with a high risk of recurrence (less than 12 months of age at first convulsion; atypical convulsion; one or several previous convulsions). Thirty one children with a high risk of recurrence received nitrazepam. The rate of recurrence in this group was 19.3% after a follow-up of 16 months, compared to 45.8% in 24 children who also had a high risk of recurrence but in whom the parents refused the medication or gave it inadequately (p<0.05). Fifty one children with a low risk of recurrence also were evaluated and followed for at least 12 months (mean 15.4 months). Six were treated with nitrazepam, mostly because of parental anxiety, and none had a recurrence; of the 45 untreated children in this group, 6 (13.6%) had another convulsion. These results show the efficiency of nitrazepam in the prophylactic treatment of febrile convulsions. RESUME: L'utilisation intermittente du diazepam par voie orale ou rectale pour le traitement prophylactique des convulsions febriles a donne d'aussi bons resultats que l'utilisation continue du phenobarbital. -

Antioxidative and Neuroprotective Effects of Leea Macrophylla
Ferdousy et al. Clinical Phytoscience (2016) 2:17 DOI 10.1186/s40816-016-0031-6 ORIGINAL CONTRIBUTION Open Access Antioxidative and neuroprotective effects of Leea macrophylla methanol root extracts on diazepam-induced memory impairment in amnesic Wistar albino rat Sakia Ferdousy1, Md Atiar Rahman1*, Md Mamun Al-Amin2, Jannatul Aklima1 and J. M. Kamirul Hasan Chowdhury1 Abstract Background: A neurological disorder is becoming one of the major health problems worldwide. Synthetic drugs for neurological disorders often produce unwanted effects while traditional plant- derived drugs offer a unique strategy in combating the neurological diseases. This study investigated how the antioxidative properties of Leea macrophylla root extracts integratively help as neuroprotective and antiamnesic in animal model. Methods: Leea macrophylla root methanol extract (LM) was assessed by open field test, hole cross test, elevated plus maze test and thiopental sodium induced sleeping time test for screening neuropharmacological effect on Wistar albino rats using the LM at 100 & 200 mg/kg body weight. Antiamnesic effect of LM was studied on diazepam induced anterograde amnesia in Wistar albino rats. Morris water maze test was performed to evaluate whether the learning and memory of rats are impaired by amnesia produced by diazepam. The antioxidative enzymes superoxide dismutase, catalase, glutathione peroxidase and oxidative biomarkers malondialdehyde, nitric oxide, advanced oxidation protein product from the hippocampus of decapitated animals were measured to assess the antioxidative potential of the extract. Results: LM was found to show significant (p <0.05) reduction in locomotor activity and increase in the duration of sleeping of animals. Morris water maze test showed that animals treated with LM significantly (p <0.05) decreased the mean escape latency compared to animals in diazepam group. -
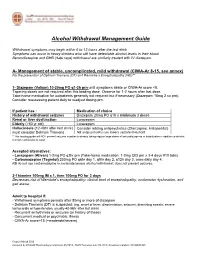
Alcohol Withdrawal Management Guide
Alcohol Withdrawal Management Guide Withdrawal symptoms may begin within 6 to 12 hours after the last drink Symptoms can occur in heavy drinkers who still have detectable alcohol levels in their blood. Benzodiazepine and GHB (date rape) withdrawal are similarly treated with IV diazepam. A- Management of stable, uncomplicated, mild withdrawal (CIWA-Ar 8-15, see annex) For the prevention of Delirium Tremens (DT) and Wernicke’s Encephalopathy (WE)** 1- Diazepam (Valium) 10-20mg PO q1-2h prn until symptoms abate or CIWA-Ar score <8. Tapering doses are not required after this loading dose. Observe for 1-2 hours after last dose. Take-home medication for outpatients generally not required but if necessary (Diazepam 10mg 2 co prn). Consider reassessing patient daily to readjust dosing prn. If patient has : Medication of choice History of withdrawal seizures Diazepam 20mg PO q1h x minimum 3 doses Renal or liver dysfunction Lorazepam Elderly (>60 yr old) Lorazepam Hallucinosis (12-48hr after last drink) Consider adding antipsychotics (Olanzapine, Haloperidol) must consider Delirium Tremens NB antipsychotics can lowers seizure threshold **This loading guide will NOT prevent seizures in patients already taking regular large doses of benzodiazepines or barbiturates in addition to alcohol. Consider admission to ward. Accepted alternatives: - Lorazepam (Ativan) 1-2mg PO q2hr prn (Take-home medication: 1-2mg QID prn x 3-4 days #10 tabs). - Carbamazepine (Tegretol) 200mg PO q6hr day 1, q8hr day 2, q12h day 3, once daily day 4. NB do not use carbamazepine in moderate/severe alcohol withdrawal: does not prevent seizures. 2-Thiamine 100mg IM x 1, then 100mg PO for 3 days Decreases risk of Wernicke's encephalopathy: clinical triad of encephalopathy, oculomotor dysfunction, and gait ataxia. -

Chloral Hydrate: Summary Report
Chloral Hydrate: Summary Report Item Type Report Authors Yuen, Melissa V.; Gianturco, Stephanie L.; Pavlech, Laura L.; Storm, Kathena D.; Yoon, SeJeong; Mattingly, Ashlee N. Publication Date 2020-02 Keywords Compounding; Food, Drug, and Cosmetic Act, Section 503B; Food and Drug Administration; Outsourcing facility; Drug compounding; Legislation, Drug; United States Food and Drug Administration; Chloral Hydrate Rights Attribution-NoDerivatives 4.0 International Download date 26/09/2021 09:06:16 Item License http://creativecommons.org/licenses/by-nd/4.0/ Link to Item http://hdl.handle.net/10713/12087 Summary Report Chloral Hydrate Prepared for: Food and Drug Administration Clinical use of bulk drug substances nominated for inclusion on the 503B Bulks List Grant number: 2U01FD005946 Prepared by: University of Maryland Center of Excellence in Regulatory Science and Innovation (M-CERSI) University of Maryland School of Pharmacy February 2020 This report was supported by the Food and Drug Administration (FDA) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award (U01FD005946) totaling $2,342,364, with 100 percent funded by the FDA/HHS. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement by, the FDA/HHS or the U.S. Government. 1 Table of Contents REVIEW OF NOMINATION ..................................................................................................... 4 METHODOLOGY ................................................................................................................... -

Tranxene (Clorazepate Dipotassium)
Tranxene* T-TAB® Tablets (clorazepate dipotassium tablets, USP) Rx only DESCRIPTION Chemically, TRANXENE is a benzodiazepine. The empirical formula is C16H11ClK2N2O4; the molecular weight is 408.92; 1H-1, 4-Benzodiazepine-3-carboxylic acid, 7-chloro-2,3 dihydro-2-oxo-5-phenyl-, potassium salt compound with potassium hydroxide (1:1) and the structural formula may be represented as follows: The compound occurs as a fine, light yellow, practically odorless powder. It is insoluble in the common organic solvents, but very soluble in water. Aqueous solutions are unstable, clear, light yellow, and alkaline. TRANXENE T-TAB tablets contain either 3.75 mg, 7.5 mg or 15 mg of clorazepate dipotassium for oral administration. Inactive ingredients for TRANXENE T-TAB Tablets: Colloidal silicon dioxide, FD&C Blue No. 2 (3.75 mg only), FD&C Yellow No. 6 (7.5 mg only), FD&C Red No. 3 (15 mg only), magnesium oxide, magnesium stearate, microcrystalline cellulose, potassium carbonate, potassium chloride, and talc. CLINICAL PHARMACOLOGY Pharmacologically, clorazepate dipotassium has the characteristics of the benzodiazepines. It has depressant effects on the central nervous system. The primary metabolite, nordiazepam, quickly appears in the blood stream. The serum half-life is about 2 days. The drug is metabolized in the liver and excreted primarily in the urine. Studies in healthy men have shown that clorazepate dipotassium has depressant effects on the central nervous system. Prolonged administration of single daily doses as high as 120 mg was without toxic effects. Abrupt cessation of high doses was followed in some patients by nervousness, insomnia, irritability, diarrhea, muscle aches, or memory impairment. -

Diazepam | Memorial Sloan Kettering Cancer Center
PATIENT & CAREGIVER EDUCATION Diazepam This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. Brand Names: US Diastat AcuDial; Diastat Pediatric; diazePAM Intensol; Valium; Valtoco 10 MG Dose; Valtoco 15 MG Dose; Valtoco 20 MG Dose; Valtoco 5 MG Dose Brand Names: Canada BIO-Diazepam; Diastat; PMS-Diazepam [DSC]; Valium Warning This drug is a benzodiazepine. The use of a benzodiazepine drug along with opioid drugs has led to very bad side effects. Side effects that have happened include slowed or trouble breathing and death. Opioid drugs include drugs like codeine, oxycodone, and morphine. Opioid drugs are used to treat pain and some are used to treat cough. Talk with the doctor. If you are taking this drug with an opioid drug, get medical help right away if you feel very sleepy or dizzy; if you have slow, shallow, or trouble breathing; or if you pass out. Caregivers or Diazepam 1/15 others need to get medical help right away if the patient does not respond, does not answer or react like normal, or will not wake up. Benzodiazepines can put you at risk for addiction, abuse, and misuse. Misuse or abuse of this drug can lead to overdose or death, especially when used along with certain other drugs, alcohol, or street drugs. Addiction can happen even if you take this drug as your doctor has told you. Get medical help right away if you have changes in mood or behavior, suicidal thoughts or actions, seizures, or trouble breathing.