Antioxidative and Neuroprotective Effects of Leea Macrophylla
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diazepam - Alcohol Withdrawal
Diazepam - alcohol withdrawal Why have I been prescribed diazepam? If a person stops drinking alcohol after a time of drinking too much they can experience withdrawal effects. These include “the shakes”, sweating, having fits, seeing things which are not there (hallucinations) and feeling anxious and low in mood. They can feel wound up and find it difficult to sleep. These withdrawal effects can be very uncomfortable and in extreme cases can be dangerous if they persist into “DTs” (delirium tremens). Diazepam is used to help reduce these withdrawal symptoms. It relieves anxiety and tension and aids sleep. Diazepam can also prevent fits. It controls the withdrawal symptoms until the body is free of alcohol and has settled down. This usually takes three to seven days from the time you stop drinking. What exactly is diazepam? Diazepam is a benzodiazepine. This group of medicines is also called anxiolytics or minor tranquillisers. Diazepam has many uses. It can be used to reduce symptoms of anxiety and insomnia, as well as to help people come off alcohol. Diazepam should only be prescribed and taken as a short course. Is diazepam safe to take? Diazepam is safe to take for a short period of time, but it doesn’t suit everyone. Below are a few conditions where diazepam may be less suitable. If any of these apply to you please tell your doctor or key-worker. If you have depression or a mental illness If you have lung disease or breathing problems, or suffer from liver or kidney trouble If you take any other medicines or drugs, including those on prescription and bought from a chemist If you take illicit drugs bought “on the street” If you are pregnant or breast-feeding What is the usual dose of diazepam? The dose of diazepam will usually be started at 10-20mg four times a day. -
What Is Diazepam?
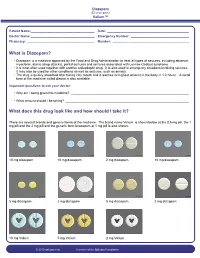
Diazepam (Di-a-ze-pam) Valium™ Patient Name: ___________________________________ Date: _____________________________________________ Doctor Name: ___________________________________ Emergency Number: ________________________________ Pharmacy: _____________________________________ Number: __________________________________________ What is Diazepam? • Diazepam is a medicine approved by the Food and Drug Administration to treat all types of seizures, including absence, myoclonic, atonic (drop attacks), partial seizures and seizures associated with Lennox-Gastaut syndrome. • It is most often used together with another antiepileptic drug. It is also used in emergency situations involving seizures. It may also be used for other conditions as well as seizures, such as anxiety. • The drug is quickly absorbed after taking it by mouth and it reaches its highest amount in the body in 1-2 hours. A rectal form of the medicine called diastat is also available. Important questions to ask your doctor: • Why am I being given this medicine? _________________________________________________________________ • What amount should I be taking? ____________________________________________________________________ What does this drug look like and how should I take it? There are several brands and generic forms of the medicine. The brand name Valium is shown below at the 0.5 mg pill, the 1 mg pill and the 2 mg pill and the generic form lorazepam at 1 mg pill is also shown. 10 mg diazepam 10 mg diazepam 2 mg diazepam 10 mg diazepam 5 mg diazepam 2 mg diazepam 5 mg diazepam 2 mg diazepam 10 mg Valium 5 mg Valium 2 mg Valium © 2010 epilepsy.com A service of the Epilepsy Foundation Diazepam (Di-a-ze-pam) Valium™ Frequently Asked Questions: How do I take Diazepam? To use the tablet form: chew tablets and swallow or swallow the tablet whole. -

Meta-Analysis of Benzodiazepine Use in the Treatment of Insomnia
Meta-analysis of benzodiazepine use in the treatment of insomnia Review Anne M. Holbrook, Renée Crowther, Ann Lotter, Chiachen Cheng, Derek King Synthèse Abstract From the Centre for Evaluation of Medicines, Objective: To systematically review the benefits and risks associated with the use St. Joseph’s Hospital of benzodiazepines to treat insomnia in adults. and McMaster University, Data sources: MEDLINE and the Cochrane Controlled Trials Registry were Hamilton, Ont. searched for English-language articles published from 1966 to December 1998 that described randomized controlled trials of benzodiazepines for the treatment This article has been peer reviewed. of insomnia. Key words included “benzodiazepines” (exploded), “randomized controlled trial” and “insomnia.” Bibliographies of relevant articles were re- CMAJ 2000;162(2):225-33 viewed for additional studies and manufacturers of benzodiazepines were asked to submit additional randomized controlled trial reports not in the literature. ß An overview of the diagnosis and management of insomnia in clinical Study selection: Articles were considered for the meta-analysis if they were ran- practice appears on page 216. domized controlled trials involving patients with insomnia and compared a ben- zodiazepine with placebo or another active agent. Of the 89 trials originally identified, 45 met our criteria, representing a total of 2672 patients. January 25, 2000 Data extraction: Data were extracted regarding the participants, the setting, details Table of Contents of the intervention, the outcomes (including adverse effects) and the method- ologic quality of the studies. Data synthesis: The meta-analyses of sleep records indicated that, when compared with placebo, benzodiazepines decreased sleep latency by 4.2 minutes (non- significant; 95% confidence interval [CI] –0.7 to 9.2) and significantly increased total sleep duration by 61.8 minutes (95% CI 37.4 to 86.2). -

Effects of Brotizolam, a New Thieno-Triazolo-Diazepine Derivative, on the Central Nervous System
In the present study, its actions on the central nervous system were investigated. Effects of Brotizolam, a New Thieno-Triazolo-Diazepine Derivative, on the Central Nervous System Kenjiro KIMISHIMA, Kyoko TANABE, Yukako KINOSHITA, Kooji TOKUYOSHI, Daisuke HOURI and Tatsuo KOBAYASHI Department of Pharmacology, Tottori University School of Medicine, Yonago 683, Japan Accepted August 24, 1984 Abstract-The effects of brotizolam, a new thieno-triazolo-diazepine derivative, on the central nervous system were analyzed in mice, rats and rabbits. Diazepam, estazolam and triazolam were used as control drugs. Brotizolam inhibited spon taneous motor activities; performances in the rotarod test, staircase test, and maximal electroshock seizure test; and pentetrazol or bemegride-induced convulsion. Moreover, catalepsy inducing action and potentiating effect on sleep elicited by pentobarbital or ethanol were observed. Following intraperitoneal or oral admin istration of brotizolam to rabbits with chronically implanted electrodes , the electro encephalographic profile in spontaneous EEG was characterized by slow waves with high amplitudes in the neocortex. The arousal responses by stimulation of the midbrain reticular formation and posterior hypothalamus were slightly inhibited, but the recruiting responses induced by stimulation of the diffuse thalamic projecting system were not inhibited, and seizure discharges induced by stimulation of the dorsal hippocampus were inhibited markedly. When motor activities and pente trazol-induced convulsions were observed as indices of tolerance for brotizolam, tolerance was not developed by repeated administration of brotizolam up to 14 days. These results suggested that brotizolam, a new thieno-triazolo-diazepine derivative, is judged to be a safer and stronger sleep inducer than diazepam and estazolam . Since the pioneering paper by Randall et et al. -

S1 Table. List of Medications Analyzed in Present Study Drug
S1 Table. List of medications analyzed in present study Drug class Drugs Propofol, ketamine, etomidate, Barbiturate (1) (thiopental) Benzodiazepines (28) (midazolam, lorazepam, clonazepam, diazepam, chlordiazepoxide, oxazepam, potassium Sedatives clorazepate, bromazepam, clobazam, alprazolam, pinazepam, (32 drugs) nordazepam, fludiazepam, ethyl loflazepate, etizolam, clotiazepam, tofisopam, flurazepam, flunitrazepam, estazolam, triazolam, lormetazepam, temazepam, brotizolam, quazepam, loprazolam, zopiclone, zolpidem) Fentanyl, alfentanil, sufentanil, remifentanil, morphine, Opioid analgesics hydromorphone, nicomorphine, oxycodone, tramadol, (10 drugs) pethidine Acetaminophen, Non-steroidal anti-inflammatory drugs (36) (celecoxib, polmacoxib, etoricoxib, nimesulide, aceclofenac, acemetacin, amfenac, cinnoxicam, dexibuprofen, diclofenac, emorfazone, Non-opioid analgesics etodolac, fenoprofen, flufenamic acid, flurbiprofen, ibuprofen, (44 drugs) ketoprofen, ketorolac, lornoxicam, loxoprofen, mefenamiate, meloxicam, nabumetone, naproxen, oxaprozin, piroxicam, pranoprofen, proglumetacin, sulindac, talniflumate, tenoxicam, tiaprofenic acid, zaltoprofen, morniflumate, pelubiprofen, indomethacin), Anticonvulsants (7) (gabapentin, pregabalin, lamotrigine, levetiracetam, carbamazepine, valproic acid, lacosamide) Vecuronium, rocuronium bromide, cisatracurium, atracurium, Neuromuscular hexafluronium, pipecuronium bromide, doxacurium chloride, blocking agents fazadinium bromide, mivacurium chloride, (12 drugs) pancuronium, gallamine, succinylcholine -

Calculating Equivalent Doses of Oral Benzodiazepines
Calculating equivalent doses of oral benzodiazepines Background Benzodiazepines are the most commonly used anxiolytics and hypnotics (1). There are major differences in potency between different benzodiazepines and this difference in potency is important when switching from one benzodiazepine to another (2). Benzodiazepines also differ markedly in the speed in which they are metabolised and eliminated. With repeated daily dosing accumulation occurs and high concentrations can build up in the body (mainly in fatty tissues) (2). The degree of sedation that they induce also varies, making it difficult to determine exact equivalents (3). Answer Advice on benzodiazepine conversion NB: Before using Table 1, read the notes below and the Limitations statement at the end of this document. Switching benzodiazepines may be advantageous for a variety of reasons, e.g. to a drug with a different half-life pre-discontinuation (4) or in the event of non-availability of a specific benzodiazepine. With relatively short-acting benzodiazepines such as alprazolam and lorazepam, it is not possible to achieve a smooth decline in blood and tissue concentrations during benzodiazepine withdrawal. These drugs are eliminated fairly rapidly with the result that concentrations fluctuate with peaks and troughs between each dose. It is necessary to take the tablets several times a day and many people experience a "mini-withdrawal", sometimes a craving, between each dose. For people withdrawing from these potent, short-acting drugs it has been advised that they switch to an equivalent dose of a benzodiazepine with a long half life such as diazepam (5). Diazepam is available as 2mg tablets which can be halved to give 1mg doses. -

Drugs of Abuse: Benzodiazepines
Drugs of Abuse: Benzodiazepines What are Benzodiazepines? Benzodiazepines are central nervous system depressants that produce sedation, induce sleep, relieve anxiety and muscle spasms, and prevent seizures. What is their origin? Benzodiazepines are only legally available through prescription. Many abusers maintain their drug supply by getting prescriptions from several doctors, forging prescriptions, or buying them illicitly. Alprazolam and diazepam are the two most frequently encountered benzodiazepines on the illicit market. Benzodiazepines are What are common street names? depressants legally available Common street names include Benzos and Downers. through prescription. Abuse is associated with What do they look like? adolescents and young The most common benzodiazepines are the prescription drugs ® ® ® ® ® adults who take the drug Valium , Xanax , Halcion , Ativan , and Klonopin . Tolerance can orally or crush it up and develop, although at variable rates and to different degrees. short it to get high. Shorter-acting benzodiazepines used to manage insomnia include estazolam (ProSom®), flurazepam (Dalmane®), temazepam (Restoril®), Benzodiazepines slow down and triazolam (Halcion®). Midazolam (Versed®), a short-acting the central nervous system. benzodiazepine, is utilized for sedation, anxiety, and amnesia in critical Overdose effects include care settings and prior to anesthesia. It is available in the United States shallow respiration, clammy as an injectable preparation and as a syrup (primarily for pediatric skin, dilated pupils, weak patients). and rapid pulse, coma, and possible death. Benzodiazepines with a longer duration of action are utilized to treat insomnia in patients with daytime anxiety. These benzodiazepines include alprazolam (Xanax®), chlordiazepoxide (Librium®), clorazepate (Tranxene®), diazepam (Valium®), halazepam (Paxipam®), lorzepam (Ativan®), oxazepam (Serax®), prazepam (Centrax®), and quazepam (Doral®). -

Drug Information Sheet("Kusuri-No-Shiori")
Drug Information Sheet("Kusuri-no-Shiori") Internal Published: 08/2015 The information on this sheet is based on approvals granted by the Japanese regulatory authority. Approval details may vary by country. Medicines have adverse reactions (risks) as well as efficacies (benefits). It is important to minimize adverse reactions and maximize efficacy. To obtain a better therapeutic response, patients should understand their medication and cooperate with the treatment. Brand name:BROTIZOLAM TABLETS 0.25mg 「OHARA」 Active ingredient:Brotizolam Dosage form:white tablet with split line on one side, diameter: 8.0 mm, thickness: 2.3 mm Print on wrapping:ブロチゾラム錠 0.25mg「オーハラ」, ブロチゾラム, 0.25mg, OH-54, Brotizolam 0.25mg「OHARA」 Effects of this medicine This medicine intensifies the effect of GABA (γ-aminobutyric acid), a typical inhibitory transmitter of central nervous system, and suppresses hypothalamic area and cerebral limbic system which control emotion. It consequently blocks unnecessary stimulation from the autonomic nervous system and shows central nervous system depressant effect including hypnotic/sedative/anti-anxiety effect. It is usually used to treat insomnia and for anesthetic premedication. Before using this medicine, be sure to tell your doctor and pharmacist ・If you have previously experienced any allergic reactions (itch, rash, etc.) to any medicines. If you have glaucoma, myasthenia gravis or respiratory disability. ・If you are pregnant or breastfeeding. ・If you are taking any other medicinal products. (Some medicines may interact to enhance or diminish medicinal effects. Beware of over-the-counter medicines and dietary supplements as well as other prescription medicines.) Dosing schedule (How to take this medicine) ・Your dosing schedule prescribed by your doctor is<< to be written by a healthcare professional>> ・For insomnia: In general, for adults, take 1 tablet (0.25 mg of the active ingredient) at a time right before bedtime. -
Alcohol Withdrawal Management Guide
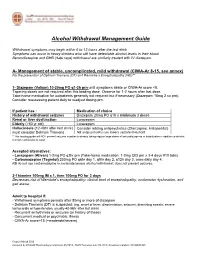
Alcohol Withdrawal Management Guide Withdrawal symptoms may begin within 6 to 12 hours after the last drink Symptoms can occur in heavy drinkers who still have detectable alcohol levels in their blood. Benzodiazepine and GHB (date rape) withdrawal are similarly treated with IV diazepam. A- Management of stable, uncomplicated, mild withdrawal (CIWA-Ar 8-15, see annex) For the prevention of Delirium Tremens (DT) and Wernicke’s Encephalopathy (WE)** 1- Diazepam (Valium) 10-20mg PO q1-2h prn until symptoms abate or CIWA-Ar score <8. Tapering doses are not required after this loading dose. Observe for 1-2 hours after last dose. Take-home medication for outpatients generally not required but if necessary (Diazepam 10mg 2 co prn). Consider reassessing patient daily to readjust dosing prn. If patient has : Medication of choice History of withdrawal seizures Diazepam 20mg PO q1h x minimum 3 doses Renal or liver dysfunction Lorazepam Elderly (>60 yr old) Lorazepam Hallucinosis (12-48hr after last drink) Consider adding antipsychotics (Olanzapine, Haloperidol) must consider Delirium Tremens NB antipsychotics can lowers seizure threshold **This loading guide will NOT prevent seizures in patients already taking regular large doses of benzodiazepines or barbiturates in addition to alcohol. Consider admission to ward. Accepted alternatives: - Lorazepam (Ativan) 1-2mg PO q2hr prn (Take-home medication: 1-2mg QID prn x 3-4 days #10 tabs). - Carbamazepine (Tegretol) 200mg PO q6hr day 1, q8hr day 2, q12h day 3, once daily day 4. NB do not use carbamazepine in moderate/severe alcohol withdrawal: does not prevent seizures. 2-Thiamine 100mg IM x 1, then 100mg PO for 3 days Decreases risk of Wernicke's encephalopathy: clinical triad of encephalopathy, oculomotor dysfunction, and gait ataxia. -

A Review of the Evidence of Use and Harms of Novel Benzodiazepines
ACMD Advisory Council on the Misuse of Drugs Novel Benzodiazepines A review of the evidence of use and harms of Novel Benzodiazepines April 2020 1 Contents 1. Introduction ................................................................................................................................. 4 2. Legal control of benzodiazepines .......................................................................................... 4 3. Benzodiazepine chemistry and pharmacology .................................................................. 6 4. Benzodiazepine misuse............................................................................................................ 7 Benzodiazepine use with opioids ................................................................................................... 9 Social harms of benzodiazepine use .......................................................................................... 10 Suicide ............................................................................................................................................. 11 5. Prevalence and harm summaries of Novel Benzodiazepines ...................................... 11 1. Flualprazolam ......................................................................................................................... 11 2. Norfludiazepam ....................................................................................................................... 13 3. Flunitrazolam .......................................................................................................................... -

Chloral Hydrate: Summary Report
Chloral Hydrate: Summary Report Item Type Report Authors Yuen, Melissa V.; Gianturco, Stephanie L.; Pavlech, Laura L.; Storm, Kathena D.; Yoon, SeJeong; Mattingly, Ashlee N. Publication Date 2020-02 Keywords Compounding; Food, Drug, and Cosmetic Act, Section 503B; Food and Drug Administration; Outsourcing facility; Drug compounding; Legislation, Drug; United States Food and Drug Administration; Chloral Hydrate Rights Attribution-NoDerivatives 4.0 International Download date 26/09/2021 09:06:16 Item License http://creativecommons.org/licenses/by-nd/4.0/ Link to Item http://hdl.handle.net/10713/12087 Summary Report Chloral Hydrate Prepared for: Food and Drug Administration Clinical use of bulk drug substances nominated for inclusion on the 503B Bulks List Grant number: 2U01FD005946 Prepared by: University of Maryland Center of Excellence in Regulatory Science and Innovation (M-CERSI) University of Maryland School of Pharmacy February 2020 This report was supported by the Food and Drug Administration (FDA) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award (U01FD005946) totaling $2,342,364, with 100 percent funded by the FDA/HHS. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement by, the FDA/HHS or the U.S. Government. 1 Table of Contents REVIEW OF NOMINATION ..................................................................................................... 4 METHODOLOGY ................................................................................................................... -

Tranxene (Clorazepate Dipotassium)
Tranxene* T-TAB® Tablets (clorazepate dipotassium tablets, USP) Rx only DESCRIPTION Chemically, TRANXENE is a benzodiazepine. The empirical formula is C16H11ClK2N2O4; the molecular weight is 408.92; 1H-1, 4-Benzodiazepine-3-carboxylic acid, 7-chloro-2,3 dihydro-2-oxo-5-phenyl-, potassium salt compound with potassium hydroxide (1:1) and the structural formula may be represented as follows: The compound occurs as a fine, light yellow, practically odorless powder. It is insoluble in the common organic solvents, but very soluble in water. Aqueous solutions are unstable, clear, light yellow, and alkaline. TRANXENE T-TAB tablets contain either 3.75 mg, 7.5 mg or 15 mg of clorazepate dipotassium for oral administration. Inactive ingredients for TRANXENE T-TAB Tablets: Colloidal silicon dioxide, FD&C Blue No. 2 (3.75 mg only), FD&C Yellow No. 6 (7.5 mg only), FD&C Red No. 3 (15 mg only), magnesium oxide, magnesium stearate, microcrystalline cellulose, potassium carbonate, potassium chloride, and talc. CLINICAL PHARMACOLOGY Pharmacologically, clorazepate dipotassium has the characteristics of the benzodiazepines. It has depressant effects on the central nervous system. The primary metabolite, nordiazepam, quickly appears in the blood stream. The serum half-life is about 2 days. The drug is metabolized in the liver and excreted primarily in the urine. Studies in healthy men have shown that clorazepate dipotassium has depressant effects on the central nervous system. Prolonged administration of single daily doses as high as 120 mg was without toxic effects. Abrupt cessation of high doses was followed in some patients by nervousness, insomnia, irritability, diarrhea, muscle aches, or memory impairment.