Review Article the Link Between Depression and Chronic Pain: Neural Mechanisms in the Brain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) United States Patent (10) Patent No.: US 9,314.465 B2 Brew Et Al
US009314465B2 (12) United States Patent (10) Patent No.: US 9,314.465 B2 Brew et al. (45) Date of Patent: *Apr. 19, 2016 (54) DRUG COMBINATIONS AND USES IN 2008.0003280 A1 1/2008 Levine et al. ................. 424/456 TREATING A COUGHING CONDITION 2008/O176955 A1 7/2008 Hecket al. 2008, 0220078 A1 9, 2008 Morton et al. (71) Applicant: Infirst Healthcare Limited 2009, O136427 A1 5/2009 Croft et al. 2009, O220594 A1 9, 2009 Field (72) Inventors: John Brew, London (GB); Robin Mark 2012/O128738 A1 5, 2012 Brew et al. Bannister, London (GB) 2012fO252824 A1 10/2012 Brew et al. (73) Assignee: Infirst Healthcare Limited, London FOREIGN PATENT DOCUMENTS (GB) CN 1593451 3, 2005 CN 101024.014 A 8, 2007 (*) Notice: Subject to any disclaimer, the term of this CN 101112383 B 5, 2010 patent is extended or adjusted under 35 DE 4420708 A1 12, 1995 U.S.C. 154(b) by 0 days. EP 2050435 B1 4/2009 GB 2114001 A 8, 1983 This patent is Subject to a terminal dis GB 2284761 A 6, 1995 claimer. GB 2424.185 B 9, 2006 GB 2442828 A 4/2008 JP 62-249924 A 10, 1987 (21) Appl. No.: 14/287,014 JP H1O-316568 A 12/1998 JP 2001-518928 A 10, 2001 (22) Filed: May 24, 2014 JP 200219.3839. A T 2002 JP 2003-012514 A 1, 2003 (65) Prior Publication Data JP 20030552.58 A 2, 2003 JP 2003128549 A 5, 2003 US 2014/O256750 A1 Sep. 11, 2014 JP 2003-321357 A 11, 2003 JP 2005-516917 A 6, 2005 JP 2008O31146 A 2, 2008 Related U.S. -

WHO Drug Information Vol. 20, No. 3, 2006
WHO DRUG INFORMATION VOLUME 20• NUMBER 3 • 2006 RECOMMENDED INN LIST 56 INTERNATIONAL NONPROPRIETARY NAMES FOR PHARMACEUTICAL SUBSTANCES WORLD HEALTH ORGANIZATION • GENEVA WHO Drug Information Vol 20, No. 3, 2006 World Health Organization WHO Drug Information Contents Biomedicines and Vaccines Counterfeit taskforce launched 192 Fake artesunate warning sheet 193 Monoclonal antibodies: a special Resolution on counterfeiting 193 regulatory challenge? 165 Improving world health through regulation of biologicals 173 Regulatory Action and News Influenza virus vaccines for 2006–2007 Safety and Efficacy Issues northern hemisphere 196 Trastuzumab approved for primary Global progress in monitoring immuniza- breast cancer 196 tion adverse events 180 Emergency contraception over-the- Intracranial haemorrhage in patients counter 197 receiving tipranavir 180 Ocular Fusarium infections: ReNu Infliximab: hepatosplenic T cell MoistureLoc® voluntary withdrawal 197 lymphoma 181 Saquinavir: withdrawal of soft gel Lamotrigine: increased risk of non- capsule Fortovase® 197 syndromic oral clefts 181 Latest list of prequalified products and Biphosphonates: osteonecrosis of manufacturers 198 the jaw 181 Clopidogrel: new medical use 199 Enoxaparin dosage in chronic kidney Dronedarone: withdrawal of marketing disease 182 authorization 199 Terbinafine and life-threatening blood dyscrasias 183 Adverse reactions in children: why Recent Publications, report? 183 Hepatitis B reactivation and anti-TNF- Information and Events alpha agents 185 MSF issues ninth antiretroviral -

WO 2008/104580 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (43) International Publication Date PCT (10) International Publication Number 4 September 2008 (04.09.2008) WO 2008/104580 Al (51) International Patent Classification: Hans-Ulrich [DE/DE]; Am Waldrand 13a, 06120 Halle / A61K 31/4164 (2006.01) C07D 405/12 (2006.01) Saale (DE). C07D 233/54 (2006.01) C07D 417/12 (2006.01) C07D 235/06 (2006.01) A61P 25/28 (2006.01) (74) Agent: HOFFMANN, Matthias; Probiodrag AG, Wein- C07D 403/12 (2006.01) bergweg 22, 06120 Halle / Saale (DE). (81) Designated States (unless otherwise indicated, for every (21) International Application Number: kind of national protection available): AE, AG, AL, AM, PCT/EP2008/05241 1 AO, AT,AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, (22) International Filing Date: EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, 28 February 2008 (28.02.2008) IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, (25) Filing Language: English MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PG, PH, PL, PT, RO, RS, RU, SC, SD, SE, SG, SK, SL, SM, SV, (26) Publication Language: English SY, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 60/892,265 1 March 2007 (0 1.03.2007) US kind of regional protection available): ARIPO (BW, GH, 11/685,881 14 March 2007 (14.03.2007) US GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, TM), (71) Applicant (for all designated States except US): PRO- European (AT,BE, BG, CH, CY, CZ, DE, DK, EE, ES, FI, BIODRUG AG [DE/DE]; Weinbergweg 22, 06120 Halle / FR, GB, GR, HR, HU, IE, IS, IT, LT,LU, LV,MC, MT, NL, Saale (DE). -

New Use of Glutaminyl Cyclase Inhibitors
(19) TZZ _Z T (11) EP 2 481 408 A2 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 01.08.2012 Bulletin 2012/31 A61K 31/4164 (2006.01) A61K 31/4184 (2006.01) A61K 31/422 (2006.01) A61K 31/4178 (2006.01) (2006.01) (2006.01) (21) Application number: 11192085.6 A61K 31/433 A61K 31/5415 A61K 31/517 (2006.01) A61P 25/28 (2006.01) (2006.01) (2006.01) (22) Date of filing: 28.02.2008 A61P 29/00 A61P 3/08 A61K 45/06 (2006.01) (84) Designated Contracting States: • Hoffmann, Torsten AT BE BG CH CY CZ DE DK EE ES FI FR GB GR 06114 Halle / Saale (DE) HR HU IE IS IT LI LT LU LV MC MT NL NO PL PT • Cynis, Holger RO SE SI SK TR 06110 Halle / Saale (DE) • Demuth, Hans-Ulrich (30) Priority: 01.03.2007 US 892265 P 06120 Halle / Saale (DE) 14.03.2007 US 685881 (74) Representative: Hoffmann, Matthias et al (62) Document number(s) of the earlier application(s) in Maikowski & Ninnemann accordance with Art. 76 EPC: Patentanwälte 08717208.6 / 2 117 540 Kurfürstendamm 54-55 10707 Berlin (DE) (71) Applicant: Probiodrug AG 06120 Halle/Saale (DE) Remarks: This application was filed on 06-12-2011 as a (72) Inventors: divisional application to the application mentioned • Schilling, Stephan under INID code 62. 06130 Halle / Saale (DE) (54) New use of glutaminyl cyclase inhibitors (57) The present invention relates in general to an c. fibrosis, e.g. lung fibrosis, liver fibrosis, renal fibrosis, inhibitor of a glutaminyl peptide cyclotransferase, and d. -

(12) United States Patent (10) Patent No.: US 8,680,042 B2 Bogdanova Et Al
USOO8680042B2 (12) United States Patent (10) Patent No.: US 8,680,042 B2 Bogdanova et al. (45) Date of Patent: Mar. 25, 2014 (54) METHODS OF TREATING SICKLE CELL (58) Field of Classification Search ANEMA-RELATED CONDITIONS WITH None MK-8O1 OR MEMANTINE See application file for complete search history. (75) Inventors: Anna Yulienva Bogdanova, Zürich (56) References Cited (CH); Max Gassman, Zürich (CH): Jeroen Goede, Wetzikon (CH) PUBLICATIONS ZempskyW. et al. “(399) Low-dose Ketamine for vasoocclusie pain (73) Assignee: Universität Zirich Prorektorat MNW, in pediatric patients with sicle cell disease: A case series' Journal of Zürich (CH) Pain, Saunders, Philadelphia vol. 9, No. 4, Apr. 1, 2008 p. 75. XPO25871572. (*) Notice: Subject to any disclaimer, the term of this Wong et al. “The Anticonvulsant MK-801 is a Potent N Methyl-D- patent is extended or adjusted under 35 Aspartate Antagonist Proceedings of the National Academy of Sci U.S.C. 154(b) by 0 days. ences of the United States of America vol. 83, No. 18, 1986, pp. 7104-7 108, XP002585977. Mosca et al. “17' International Symposium of the European Asso (21) Appl. No.: 13/265,709 ciation for Red Cell Research, EARCR2009, Triuggio, Milano, Italy, Apr. 23-27, 2009” Clinical Biochemistry, Elsevier Inc, US CA (22) PCT Filed: Apr. 18, 2010 LNKD vol. 42, No. 18, Dec. 1, 2009, pp. 1851-1863, XPO26782104. (86). PCT No.: PCT/EP2010/055.077 Primary Examiner — Robert Landsman S371 (c)(1), (74) Attorney, Agent, or Firm — Cozen O'Connor (2), (4) Date: Jan. 19, 2012 (57) ABSTRACT (87) PCT Pub. -

WO 2011/089216 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date t 28 July 2011 (28.07.2011) WO 2011/089216 Al (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 47/48 (2006.01) C07K 1/13 (2006.01) kind of national protection available): AE, AG, AL, AM, C07K 1/1 07 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) Number: International Application DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/EP201 1/050821 HN, HR, HU, ID, J , IN, IS, JP, KE, KG, KM, KN, KP, (22) International Filing Date: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 2 1 January 201 1 (21 .01 .201 1) ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, (26) Publication Language: English TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 1015 1465. 1 22 January 2010 (22.01 .2010) EP kind of regional protection available): ARIPO (BW, GH, GM, KE, LR, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, (71) Applicant (for all designated States except US): AS- ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, CENDIS PHARMA AS [DK/DK]; Tuborg Boulevard TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, 12, DK-2900 Hellerup (DK). -

(12) Patent Application Publication (10) Pub. No.: US 2012/0157420 A1 Schneider (43) Pub
US 2012O157420A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2012/0157420 A1 Schneider (43) Pub. Date: Jun. 21, 2012 (54) TREATMENT AND PREVENTION OF A 6LX 3L/505 (2006.01) SECONDARY INTURY AFTER TRAUMA OR A6IP 29/00 (2006.01) DAMAGE TO THE CENTRAL NERVOUS A6II 3/47 (2006.01) SYSTEM A6IP 25/00 (2006.01) A6IP3/06 (2006.01) (76) Inventor: Eric B Schneider, Glen Arm, MD A6IP 9/00 (2006.01) (US) A6IP 25/22 (2006.01) A6IP 25/24 (2006.01) (21) Appl. No.: 13/392,371 A63L/366 (2006.01) A6II 3/40 (2006.01) (22) PCT Filed: Aug. 31, 2010 (52) U.S. Cl. ......... 514/171; 514/460, 514/419:514/510; (86). PCT No.: PCT/US 10/472O6 514/277; 514/275: 514/423: 514/311 S371 (c)(1), (57) ABSTRACT (2), (4) Date: Feb. 24, 2012 A method of administering one or multiple medications to human patients with CNS injury through oral or parenteral Related U.S. Application Data (including transdermal, intravenous, Subcutaneous, intra (60) Provisional application No. 61/238,453, filed on Aug. muscular) routes. Inflammatory and immunological pro 31, 2009. cesses have been shown to cause secondary damage to CNS s tissues in individuals with acute CNS injury. The present O O invention administers one or more of the following medica Publication Classification tions, which have properties that mitigate the inflammatory (51) Int. Cl. and immunological processes that lead to secondary CNS A6 IK3I/56 (2006.01) damage, via trans-dermal absorption: a statin compound A6 IK 3/405 (2006.01) (e.g., a HMG-CoA reductase inhibitor), a progesterone com A6 IK 3L/25 (2006.01) pound, or a cholinesterase inhibiting compound, among oth A6 IK 3/448 (2006.01) ers, either alone or in combination with other compounds. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

A Abacavir Abacavirum Abakaviiri Abagovomab Abagovomabum
A abacavir abacavirum abakaviiri abagovomab abagovomabum abagovomabi abamectin abamectinum abamektiini abametapir abametapirum abametapiiri abanoquil abanoquilum abanokiili abaperidone abaperidonum abaperidoni abarelix abarelixum abareliksi abatacept abataceptum abatasepti abciximab abciximabum absiksimabi abecarnil abecarnilum abekarniili abediterol abediterolum abediteroli abetimus abetimusum abetimuusi abexinostat abexinostatum abeksinostaatti abicipar pegol abiciparum pegolum abisipaaripegoli abiraterone abirateronum abirateroni abitesartan abitesartanum abitesartaani ablukast ablukastum ablukasti abrilumab abrilumabum abrilumabi abrineurin abrineurinum abrineuriini abunidazol abunidazolum abunidatsoli acadesine acadesinum akadesiini acamprosate acamprosatum akamprosaatti acarbose acarbosum akarboosi acebrochol acebrocholum asebrokoli aceburic acid acidum aceburicum asebuurihappo acebutolol acebutololum asebutololi acecainide acecainidum asekainidi acecarbromal acecarbromalum asekarbromaali aceclidine aceclidinum aseklidiini aceclofenac aceclofenacum aseklofenaakki acedapsone acedapsonum asedapsoni acediasulfone sodium acediasulfonum natricum asediasulfoninatrium acefluranol acefluranolum asefluranoli acefurtiamine acefurtiaminum asefurtiamiini acefylline clofibrol acefyllinum clofibrolum asefylliiniklofibroli acefylline piperazine acefyllinum piperazinum asefylliinipiperatsiini aceglatone aceglatonum aseglatoni aceglutamide aceglutamidum aseglutamidi acemannan acemannanum asemannaani acemetacin acemetacinum asemetasiini aceneuramic -

(TENS) Intag Av Smärtstillande Läkemedel?
Detta är ett svar från SBU:s Upplysningstjänst den 4 december 2012. SBU:s Upplysningstjänst svarar på avgränsade medicinska frågor. Svaret bygger inte på en systematisk litteraturöversikt, varför resultaten av litteratursökningen kan vara ofullständiga. Kvaliteten på ingående studier har inte bedömts. Detta svar har tagits fram av SBU:s kansli och har inte granskats av SBU:s råd eller nämnd. Minskar transkutan elektrisk nervstimulering (TENS) intag av smärtstillande läkemedel? Transkutan elektrisk nervstimulering (TENS) används för att minska både akut och långvarig smärta. Det finns en osäkerhet angående hur effektiv TENS-behandling är och om den kan minska intag av smärtstillande läkemedel. Fråga: Dfgdfg”Minskar transkutan elektrisk nervstimulering (TENS) intag av smärtstillande läkemedel vid akut eller långvarig smärta?” Sammanfattning I en systematisk översikt analyserar författarna om TENS minskar smärta och påverkar konsumtionen av smärtstillande läkemedel vid menskramper. I den andra systematiska översikten och i åtta randomiserade kontrollerade studier (RCT:er) studeras om TENS minskar konsumtionen av smärtstillande läkemedel efter operation. I ytterligare en RCT studerar författarna om TENS-behandling kan minska långvarig smärta som uppkommer vid bröstcancerbehandling och påverka konsumtion av smärtstillande läkemedel. Författarna till de systematiska översikterna menar att dubbelblindning är svårt att utföra i TENS-studier, vilket kan leda till systematiska fel. Behandling med TENS ges i vissa studier av patienterna själva och i andra studier av sjukvårdspersonal. När TENS utförs av patienterna kan det bli stora variationer i hur elektroderna placeras på kroppen, vilket kan påverka resultatet. Sammanfattningsvis drar författarna till studierna, i vilka man undersöker patienter efter operation, slutsatsen att TENS-behandling kan minska konsumtion av smärtstillande läkemedel. -
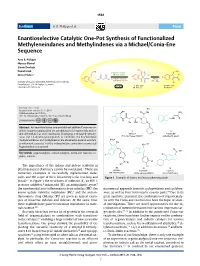
Enantioselective Catalytic One-Pot Synthesis of Functionalized Methyleneindanes and Methylindenes Via a Michael/Conia-Ene Sequence
SYNTHESIS0039-78811437-210X © Georg Thieme Verlag Stuttgart · New York 2017, 49, 1538–1546 1538 paper Syn thesis A. R. Philipps et al. Paper Enantioselective Catalytic One-Pot Synthesis of Functionalized Methyleneindanes and Methylindenes via a Michael/Conia-Ene Sequence Arne R. Philipps Marcus Blümel Simon Dochain O2N Daniel Hack NO NO2 2 1) Organocatalytic O 2 Dieter Enders* O O Michael addition R2 R + R1 R1 2 1 2 2 2) Indium-catalyzed R – ketene R R R O Conia-ene reaction (R2 = Me) Institute of Organic Chemistry, RWTH Aachen University, O Me Landoltweg 1, 52074 Aachen, Germany one pot 3–98% yield 23–99% yield [email protected] 76–99% ee 95–99% ee Received: 09.11.2016 tBu Accepted after revision: 11.11.2016 OH O NH NH2 Published online: 06.12.2016 O DOI: 10.1055/s-0036-1588113; Art ID: ss-2016-z0789-op N N NH O H Bn OH N Abstract An enantioselective one-pot Michael addition/Conia-ene re- action sequence catalyzed by the combination of a squaramide and in- I II N dium(III) triflate has been developed. Employing 2-ethynyl-β-nitrosty- indinavir indantadol renes and 1,3-dicarbonyl compounds as substrates, the functionalized HIV-1 protease inhibitor antiepileptic agent methyleneindanes and methylindenes are obtained in good to excellent CO2H Me enantiomeric excesses. For the indane/indene conversion a concerted HN Me fragmentation is proposed. O OH Key words organocatalysis, indium catalysis, Conia-ene reaction, in- Cl danes, indenes F Cl S O Me The importance of the indane and indene scaffolds in Cl 1 III IV V pharmaceutical chemistry cannot be overstated. -
Who Drug Information
WHO DRUG INFORMATION VOLUME 19 NUMBER 4 • 2005 PROPOSED INN LIST 94 INTERNATIONAL NONPROPRIETARY NAMES FOR PHARMACEUTICAL SUBSTANCES WORLD HEALTH ORGANIZATION - GENEVA WHO Drug Information Vol 19, No. 4, 2005 World Health Organization WHO Drug Information Contents Drug Management Regulatory Action and News Avian influenza: impact on health Safety update on paediatric use of programmes 273 oseltamivir 301 Influenza antiviral medicinal products for Influenza virus composition for 2006 potential use during a pandemic 274 southern hemisphere winter 301 International biosafety guidelines for Safety and Efficacy Issues influenza vaccine production 301 Veralipride: withdrawal following review of Safety challenges of preventing malaria risk/benefit 302 during pregnancy 286 Pemoline: liver injury risk and market WHO International Drug Monitoring withdrawal 302 Programme: 28th meeting 287 Nelarabine approved for leukaemia and Statins and memory loss 288 lymphoma 303 New safety information on long-acting EMEA proposes new, faster scientific beta-2 agonists 289 advice procedure 303 Meningococcal vaccine and Guillain Barre Withdrawal of Infanrix HepB® 303 syndrome 290 Precautionary suspension of Hexavac®: Trastuzumab and possible cardiotoxicity 291 lowered immunogenicity 304 Trastuzumab: interim treatment Environmental risk assessment for human recommendations 291 and veterinary medicinal products 304 Oseltamivir paediatric adverse events 291 Duloxetine hydrochloride and hepatic effects 292 Intrathecal baclofen: incidents with implantable Recent Publications,