Adaptive Specific Host Defenses 771
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
IFM Innate Immunity Infographic
UNDERSTANDING INNATE IMMUNITY INTRODUCTION The immune system is comprised of two arms that work together to protect the body – the innate and adaptive immune systems. INNATE ADAPTIVE γδ T Cell Dendritic B Cell Cell Macrophage Antibodies Natural Killer Lymphocites Neutrophil T Cell CD4+ CD8+ T Cell T Cell TIME 6 hours 12 hours 1 week INNATE IMMUNITY ADAPTIVE IMMUNITY Innate immunity is the body’s first The adaptive, or acquired, immune line of immunological response system is activated when the innate and reacts quickly to anything that immune system is not able to fully should not be present. address a threat, but responses are slow, taking up to a week to fully respond. Pathogen evades the innate Dendritic immune system T Cell Cell Through antigen Pathogen presentation, the dendritic cell informs T cells of the pathogen, which informs Macrophage B cells B Cell B cells create antibodies against the pathogen Macrophages engulf and destroy Antibodies label invading pathogens pathogens for destruction Scientists estimate innate immunity comprises approximately: The adaptive immune system develops of the immune memory of pathogen exposures, so that 80% system B and T cells can respond quickly to eliminate repeat invaders. IMMUNE SYSTEM AND DISEASE If the immune system consistently under-responds or over-responds, serious diseases can result. CANCER INFLAMMATION Innate system is TOO ACTIVE Innate system NOT ACTIVE ENOUGH Cancers grow and spread when tumor Certain diseases trigger the innate cells evade detection by the immune immune system to unnecessarily system. The innate immune system is respond and cause excessive inflammation. responsible for detecting cancer cells and This type of chronic inflammation is signaling to the adaptive immune system associated with autoimmune and for the destruction of the cancer cells. -

Gamma-Irradiated SARS-Cov-2 Vaccine Candidate, OZG-38.61.3, Confers Protection from SARS-Cov-2 Challenge in Human ACEII-Transgen
www.nature.com/scientificreports OPEN Gamma‑irradiated SARS‑CoV‑2 vaccine candidate, OZG‑38.61.3, confers protection from SARS‑CoV‑2 challenge in human ACEII‑transgenic mice Raife Dilek Turan1,2,19, Cihan Tastan1,3,4,19*, Derya Dilek Kancagi1,19, Bulut Yurtsever1,19, Gozde Sir Karakus1,19, Samed Ozer5, Selen Abanuz1,6, Didem Cakirsoy1,8, Gamze Tumentemur7, Sevda Demir2, Utku Seyis1, Recai Kuzay1, Muhammer Elek1,2, Miyase Ezgi Kocaoglu1, Gurcan Ertop7, Serap Arbak9, Merve Acikel Elmas9, Cansu Hemsinlioglu1, Ozden Hatirnaz Ng10, Sezer Akyoney10,11, Ilayda Sahin8,12, Cavit Kerem Kayhan13, Fatma Tokat14, Gurler Akpinar15, Murat Kasap15, Ayse Sesin Kocagoz16, Ugur Ozbek12, Dilek Telci2, Fikrettin Sahin2, Koray Yalcin1,17, Siret Ratip18, Umit Ince14 & Ercument Ovali1 The SARS‑CoV‑2 virus caused the most severe pandemic around the world, and vaccine development for urgent use became a crucial issue. Inactivated virus formulated vaccines such as Hepatitis A and smallpox proved to be reliable approaches for immunization for prolonged periods. In this study, a gamma‑irradiated inactivated virus vaccine does not require an extra purifcation process, unlike the chemically inactivated vaccines. Hence, the novelty of our vaccine candidate (OZG‑38.61.3) is that it is a non‑adjuvant added, gamma‑irradiated, and intradermally applied inactive viral vaccine. Efciency and safety dose (either 1013 or 1014 viral RNA copy per dose) of OZG‑38.61.3 was initially determined in BALB/c mice. This was followed by testing the immunogenicity and protective efcacy of the vaccine. Human ACE2‑encoding transgenic mice were immunized and then infected with the SARS‑CoV‑2 virus for the challenge test. -

Innate Immunity in the Lung: How Epithelial Cells Fight Against
Copyright #ERSJournals Ltd 2004 EurRespir J 2004;23: 327– 333 EuropeanRespiratory Journal DOI: 10.1183/09031936.03.00098803 ISSN0903-1936 Printedin UK –allrights reserved REVIEW Innateimmunity in the lung: how epithelialcells ght against respiratorypathogens R. Bals*,P.S. Hiemstra # Innateimmunity in the lung: how epithelial cells ® ghtagainst respiratory pathogens *Deptof Internal Medicine, Division of R Bals, P S Hiemstra #ERS JournalsLtd 2004 PulmonaryMedicine, Hospital of the Uni- versityof Marburg, Philipps-University, ABSTRACT: Thehuman lung is exposed to a largenumber of airborne pathogens as a # resultof the daily inhalation of 10,000 litres of air Theobservation that respiratory Marburg,Germany; Deptof Pulmonology, LeidenUniversity Medical Center, Leiden, infectionsare nevertheless rare is testimony to the presence of anef®cient host defence TheNetherlands systemat the mucosal surface of the lung Theairway epithelium is strategically positioned at the interface with the Correspondence:P S Hiemstra,Dept of environment,and thus plays a keyrole in this host defence system Recognition Pulmonology,Leiden University Medical systemsemployed by airwayepithelial cells to respond to microbialexposure include the Center, P O Box9600, 2300 RC Leiden, The actionof the toll-like receptors Netherlands Theairway epithelium responds to such exposure by increasing its production of Fax:31 715266927 mediatorssuch as cytokines, chemokines and antimicrobial peptides Recent® ndings E-mail: p s hiemstra@lumc nl indicatethe importance of these peptides -

(ACIP) General Best Guidance for Immunization
8. Altered Immunocompetence Updates This section incorporates general content from the Infectious Diseases Society of America policy statement, 2013 IDSA Clinical Practice Guideline for Vaccination of the Immunocompromised Host (1), to which CDC provided input in November 2011. The evidence supporting this guidance is based on expert opinion and arrived at by consensus. General Principles Altered immunocompetence, a term often used synonymously with immunosuppression, immunodeficiency, and immunocompromise, can be classified as primary or secondary. Primary immunodeficiencies generally are inherited and include conditions defined by an inherent absence or quantitative deficiency of cellular, humoral, or both components that provide immunity. Examples include congenital immunodeficiency diseases such as X- linked agammaglobulinemia, SCID, and chronic granulomatous disease. Secondary immunodeficiency is acquired and is defined by loss or qualitative deficiency in cellular or humoral immune components that occurs as a result of a disease process or its therapy. Examples of secondary immunodeficiency include HIV infection, hematopoietic malignancies, treatment with radiation, and treatment with immunosuppressive drugs. The degree to which immunosuppressive drugs cause clinically significant immunodeficiency generally is dose related and varies by drug. Primary and secondary immunodeficiencies might include a combination of deficits in both cellular and humoral immunity. Certain conditions like asplenia and chronic renal disease also can cause altered immunocompetence. Determination of altered immunocompetence is important to the vaccine provider because incidence or severity of some vaccine-preventable diseases is higher in persons with altered immunocompetence; therefore, certain vaccines (e.g., inactivated influenza vaccine, pneumococcal vaccines) are recommended specifically for persons with these diseases (2,3). Administration of live vaccines might need to be deferred until immune function has improved. -
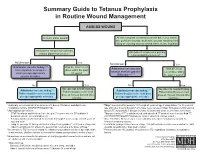
Summary Guide to Tetanus Prophylaxis in Routine Wound Management
Summary Guide to Tetanus Prophylaxis in Routine Wound Management ASSESS WOUND A clean, minor wound All other wounds (contaminated with dirt, feces, saliva, soil; puncture wounds; avulsions; wounds resulting from flying or crushing objects, animal bites, burns, frostbite) Has patient completed a primary Has patient completed a primary tetanus diphtheria series?1, 7 tetanus diphtheria series?1, 7 No/Unknown Yes No/Unknown Yes Administer vaccine today.2,3,4 Was the most recent Administer vaccine and Was the most Instruct patient to complete dose within the past tetanus immune gobulin recent dose within series per age-appropriate 10 years? (TIG) now.2,4,5,6,7 the past 5 years?7 vaccine schedule. No Yes No Yes Vaccine not needed today. Vaccine not needed today. Administer vaccine today.2,4 2,4 Patient should receive next Administer vaccine today. Patient should receive next Patient should receive next dose Patient should receive next dose dose at 10-year interval after dose at 10-year interval after per age-appropriate schedule. per age-appropriate schedule. last dose. last dose. 1 A primary series consists of a minimum of 3 doses of tetanus- and diphtheria- 4 Tdap* is preferred for persons 11 through 64 years of age if using Adacel* or 10 years of containing vaccine (DTaP/DTP/Tdap/DT/Td). age and older if using Boostrix* who have never received Tdap. Td is preferred to tetanus 2 Age-appropriate vaccine: toxoid (TT) for persons 7 through 9 years, 65 years and older, or who have received a • DTaP for infants and children 6 weeks up to 7 years of age (or DT pediatric if Tdap previously. -
Information and Communication Guide on Vaccines
Module 2 EUROPEAN NURSE Information and Communication Guide ON VACCINES The European Specialist Nurses Organisation (ESNO) is a non-profit organisation with the goal to facilitate and provide an effective framework for communication and co-operation between the European Specialist Nurses Organisations and its constituent members. ESNO represents the mutual interests and benefits of these organisations to the wider European community in the interest of the public health. Members of ESNO consist of individual European specialist nurses member organizations and associates, both institutional and individual. The organisation focusses on enhancing the capacity and capability of specialists nurses to deliver hight quality healthcare by raising and harmonise specialist nursing education standards and actively contribute to health themes and threats, providing the best possible expertise, both national and in European cross border context. A publication from the European Specialist Nurses Organisation April 2021 - www.esno.org Copyright: ©2021 European Specialist Nurses Organisation. All rights reserved. No part of this publication may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the publisher, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law. CONTENTS Vaccination 1 Introduction 5 2 Principles of vaccination 6 2.1 Principle -
Calreticulin—Multifunctional Chaperone in Immunogenic Cell Death: Potential Significance As a Prognostic Biomarker in Ovarian
cells Review Calreticulin—Multifunctional Chaperone in Immunogenic Cell Death: Potential Significance as a Prognostic Biomarker in Ovarian Cancer Patients Michal Kielbik *, Izabela Szulc-Kielbik and Magdalena Klink Institute of Medical Biology, Polish Academy of Sciences, 106 Lodowa Str., 93-232 Lodz, Poland; [email protected] (I.S.-K.); [email protected] (M.K.) * Correspondence: [email protected]; Tel.: +48-42-27-23-636 Abstract: Immunogenic cell death (ICD) is a type of death, which has the hallmarks of necroptosis and apoptosis, and is best characterized in malignant diseases. Chemotherapeutics, radiotherapy and photodynamic therapy induce intracellular stress response pathways in tumor cells, leading to a secretion of various factors belonging to a family of damage-associated molecular patterns molecules, capable of inducing the adaptive immune response. One of them is calreticulin (CRT), an endoplasmic reticulum-associated chaperone. Its presence on the surface of dying tumor cells serves as an “eat me” signal for antigen presenting cells (APC). Engulfment of tumor cells by APCs results in the presentation of tumor’s antigens to cytotoxic T-cells and production of cytokines/chemokines, which activate immune cells responsible for tumor cells killing. Thus, the development of ICD and the expression of CRT can help standard therapy to eradicate tumor cells. Here, we review the physiological functions of CRT and its involvement in the ICD appearance in malignant dis- ease. Moreover, we also focus on the ability of various anti-cancer drugs to induce expression of surface CRT on ovarian cancer cells. The second aim of this work is to discuss and summarize the prognostic/predictive value of CRT in ovarian cancer patients. -

Vaccines 101 the Very Last Day That I Was a Pediatric Resident. Um, Many
Vaccines 101 The very last day that I was a pediatric resident. Um, many years ago, a toddler walked into the emergency room and uh, and progressively got sicker and sicker. That's Dr. Katherine Edwards, a world expert in pediatric infectious disease in vaccinology. She's also a professor of pediatrics at Vanderbilt university and she's been working on vaccines for 40 years. I did a spinal tap on her and realized that she had Haemophilus influenza, typ e B meningitis, Haemophilus influenza, type B or HIB is it bacteria normally found in our nose and throat that can lead to very serious life threatening infections and no matter what I did in that day and into the night in terms of prompt antibiotics and she'd just been sick a few hours and, and fluids and all the, you know, ventilators and all the best things that modern medicine, she died, the vaccine for hip was not available until the 1990s. And until it did become available, hip disease affected approximately 25,000 children each year with things like meningitis, pneumonia, and bloodstream infections. And at that time in the hospital that I was practicing at any one time, there were generally five or six patients that had Haemophilus meningitis or invasive disease or some complication of this particular infection. And we knew that from the basic science that if you had antibody to the capsule or to the coat of the organism, that you were protected from disease. But we really didn't know how to make little kids make antibody. -

Bcch 2019-20 Flu Vaccine – Oncology Clinic
BCCH 2019-20 FLU VACCINE – ONCOLOGY CLINIC We are providing influenza vaccines for patients who are on therapy and have platelets > 50,000 and ANC over 0.5 (and expected to stay above 0.5 for the next 48 hours, in order to minimize risk of admission in case of fever). Please do not schedule appointments for flu shots only. Please advise the family that immunization of all family members is recommended. The Oncology Outpatient Clinic is not providing immunizations for family members or for those patients who are OFF therapy. Flu shots can be given by family doctors to patients and their families, or they can get a flu shot at the BCCH drop-in Family Immunization clinic in the Ambulatory Care Building, across from the Ambulatory Care Pharmacy on week days in the fall months. Pediatric oncology patients can also get a flu shot at almost any community pharmacy at no cost as they are considered “at risk.” Age Dose** Doses required 6 months – 9 years 0.5 mL IM 1 or 2* > 9 years 0.5 mL IM 1 Less than 6 months Not recommended *Two doses administered at least 4 weeks apart are recommended for children under 9 years of age who are receiving influenza vaccine for the first time. **The recommended site of vaccination is the deltoid muscle for adults and older children. The preferred site for infants and young children is the anterolateral aspect of the thigh. Contraindications: • Febrile illness • Thimerosal sensitivity Special considerations: • Egg allergic individuals (including those who have experienced anaphylaxis following egg ingestion) can be immunized with inactivated influenza vaccine (such as Flulaval tetra) • Thimerosal allergic patients should be vaccinated using Agriflu which can be obtained from local public health units, (but not in the oncology clinic). -

COVID-19 Vaccination Strategy in China: a Case Study
Article COVID-19 Vaccination Strategy in China: A Case Study Marjan Mohamadi 1,†, Yuling Lin 1,*,† ,Mélissa Vuillet Soit Vulliet 1,†, Antoine Flahault 1, Liudmila Rozanova 1 and Guilhem Fabre 2 1 Institute of Global Health, University of Geneva, 1211 Geneva, Switzerland; [email protected] (M.M.); [email protected] (M.V.S.V.); antoine.fl[email protected] (A.F.); [email protected] (L.R.) 2 Department of Chinese, UFR 2, Université Paul Valéry Montpellier 3, 34199 Montpellier, France; [email protected] * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: The coronavirus disease 2019 (COVID-19) outbreak in China was first reported to the World Health Organization on 31 December 2019, after the first cases were officially identified around 8 December 2019. However, the case of an infected patient of 55 years old can probably be traced back on 17 November. The spreading has been rapid and heterogeneous. Economic, political and social impacts have not been long overdue. This paper, based on English, French and Chinese research in national and international databases, aims to study the COVID-19 situation in China through the management of the outbreak and the Chinese response to vaccination strategy. The coronavirus disease pandemic is under control in China through non-pharmaceutical interventions, and the mass vaccination program has been launched to further prevent the disease and progressed steadily with Citation: Mohamadi, M.; Lin, Y.; 483.34 million doses having been administered across the country by 21 May 2021. China is also Vulliet, M.V.S.; Flahault, A.; acting as an important player in the development and production of SARS-CoV-2 vaccines. -
Immunisation How Vaccines Work
Immunisation How vaccines work Dr Fiona Ryan Consultant in Public Health Medicine, Department of Public Health April 2015 Presentation Outline • An understanding of the following principles • Overview of immunity • Different types of vaccines and vaccine contents • Vaccine failures • Time intervals between vaccine doses • Vaccine overload • Adverse reactions • Herd immunity Immunity Immunity • – The ability of the human body to protect itself from infectious disease The immune system • Cells with a protective function in the – bone marrow –thymus – lymphatic system of ducts and nodes – spleen – blood Types of immunity Source: http://en.wikipedia.org/wiki/Immunological_memory Natural (innate) immunity Non-specific mechanisms – Physical barriers • skin and mucous membranes – Chemical barriers • gastric and digestive enzymes – Cellular and protein secretions • phagocytes, macrophages, complement system ** No “memory” of protection exists afterwards ** Passive immunity – adaptive mechanisms Natural • maternal transfer of antibodies to infant via placenta Artificial • administration of pre- formed substance to provide immediate but short-term protection (anti- toxin, antibodies) Protection is temporary and wanes with time (usually few months) Active immunity – adaptive mechanisms Natural • following contact with organism Artificial • administration of agent to stimulate immune response (immunisation) Acquired through contact with an micro-organism Protection produced by individual’s own immune system Protection often life-long but may need -

Qnas with Max D. Cooper and Jacques F. A. P. Miller
QNAS QnAswithMaxD.CooperandJacquesF.A.P.Miller QNAS Brian Doctrow, Science Writer Anyone who has ever contracted chicken pox can thank the adaptive immune system for future pro- tection against the disease. It is also thanks to this system that vaccines prevent diseases. The adaptive immune system provides organisms with a memory of past infections, enabling the body to quickly kill returning infections before they can do significant damage. Immunologists Jacques F. A. P. Miller and Max D. Cooper determined that adaptive immunity requires 2 distinct cell types that perform comple- mentary functions. Miller’s findings, published in the early 1960s in Lancet (1) and Proceedings of the Royal Society (2), showed that the ability to distinguish one’s own cells from foreign cells, a key feature of the adap- tive immune system, depends on lymphocytes, now known as T cells, matured in an organ called the thy- mus. Subsequently, Cooper reported in Nature (3) that Max Dale Cooper. Image courtesy of Georgia Research antibody production depends on a separate set of Alliance/Billy Howard. lymphocytes, dubbed B cells. The division of labor between T and B cells is a fundamental organizing principle of the adaptive immune system, the discov- did cancer research. I started working on leukemia and ery of which laid the groundwork for modern immu- this gave me an interest in lymphocytes. nology and made possible many subsequent medical advances, including monoclonal antibody produc- Cooper: I became interested through patients that I tion, vaccine development, and checkpoint inhibi- was taking care of: Children that had deficient immune tion therapies for cancer.