View the 2021 Index
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Health Hazard Evaluation Report 1983-0019-1562
r ILi:. llUr I Health Hazard . Evaluation HETA 83-019-1562 I BERLEX LABS. Report WAYNE., NEW JERSEY . "'-':'. ·· J· PREFACE .......~ The Hazard Evaluation~ ·- ~nd .. "rechni cal Assistance Branch of NIOSH conducts field i nyesti gations of possible hea.lth hazards i n the workplace. These investigations ~are conducted ~under the authority of Section 20(a)(6) of the Occupational Safety and.,Heal'ttr Act of 1970 , 29 u ~ s.c. 66~(a)(6) which authorizes t he Secretary of Health·and Human Services, following a written request from any employer of~ au~horized representative of employees, to determine whether any substance normally found in the place of employ~nt has potentiall~ toxic· .effects in such concentrations as used or fotmd. The Hazard Evaluations and Technical Assistance Branch also provides, upon request, medical, nursing, and industrial hygiene technical and consultative assistance (TA) to Federal, state, and local agencies; labor; industry and other groups or individuals to control occupational health hazards and to prevent related trauma and disease. Mention of company nair.es or products does not constitute e ndorsement by the National Institute for Occupational Safety and Health. HETA 83-019-1562 Investigators: SEPTEMBER, 1985 REVISED Raja Igliewicz, RN, MS BERLEX LABS. Michael Schmidt, MD WAYNE, NEW JERSEY Peter Gann, MD 1. SUMMARY In October, 1982, the National Institute for Occupational Safety and Health (NIOSH) received a request to evaluate workers involved in the production of a drug, quinidine gluconate at Berlex Laborateries, Wayne, N.J. These workers had developed work-related skin rashes and respiratory symptoms. Staff from the Occupational Health Program of the New Jersey State Department of Health performed the investigation under a cooperative agreement with NlOSH. -

Clinical an Urgent Care Approach to Complications and Conditions of Pregnancy Part 2
Clinical An Urgent Care Approach to Complications and Conditions of Pregnancy Part 2 Urgent message: From pregnancy confirmation to the evaluation of bleeding, urgent care centers are often the initial location for management of obstetric-related issues. Careful use of evidence-based guidelines is the key to successful outcomes. DAVID N. JACKSON, MD, FACOG and PETAR PLANINIC, MD, FACOG Introduction rgent care providers are called upon to manage a Uvariety of complaints in pregnancy. Some conditions can be managed at the urgent care center whereas others require stabilization and transport to a center with expert obstetrical capabilities. In all situations, practitioners should consider that a gestational age of fetal viability (many centers now use 23 to 24 weeks) is best served with referral for continuous fetal monitor- ing if there is bleeding, trauma, significant hypertension, relative hypoxemia (O2 saturation less than 95% for pregnant women), or contractions. Part 2 of this two- part series will discuss: Ⅲ Bleeding in pregnancy Ⅲ Ectopic gestation Ⅲ Trauma and pregnancy Ⅲ Acute abdominal pain in pregnancy Dr. Jackson is Professor of Maternal-Fetal Medicine at the University of Nevada, School of Medicine, Las Vegas, Nevada. Dr. Planinic is Assistant Professor of Obstetrics and Gynecology at the University of Nevada, School of Medicine, Las Vegas, Nevada. © gettyimages.com www.jucm.com JUCM The Journal of Urgent Care Medicine | September 2013 9 AN URGENT CARE APPROACH TO COMPLICATIONS AND CONDITIONS OF PREGNANCY Figure 1. Bleeding endocervical polyp with Evaluation of vaginal bleeding should follow a sys- inflammation tematic process. History of last menses and sexual activ- ity determines the possibility of pregnancy. -

Pulmonary Cancer And/Or GPA? Diagnostic Implications of Pulmonary Nodules
Gaceta Médica de México. 2016;152 Contents available at PubMed www.anmm.org.mx PERMANYER Gac Med Mex. 2016;152:468-74 www.permanyer.com GACETA MÉDICA DE MÉXICO ORIGINAL ARTICLE Pulmonary pseucotumor in granulomatosis with polyangiitis (GPA). Pulmonary cancer and/or GPA? Diagnostic implications of pulmonary nodules Gabriel Horta-Baas1*, Esteban Meza-Zempoaltecatl2, Mario Pérez-Cristóbal2 and Barile-Fabris Leonor Adriana2 1Rheumatology Department, Hospital General Regional 220, IMSS, Toluca; 2Rheumatology Department, Hospital de Especialidades, Centro Médico Nacional Siglo XXI, IMSS, Mexico City, Mexico Abstract Granulomatosis with polyangiitis (GPA), formerly known as Wegener’s granulomatosis, is a systemic necrotizing vasculitis, which affects small and medium sized blood vessels and is often associated with cytoplasmic anti-neutrophil cytoplasmic antibodies (ANCA). Inflammatory pseudotumor is a rare condition characterized by the appearance of a mass lesion that mimics a malignant tumor both clinically and on imaging studies, but that is thought to have an inflammatory/reactive pathogenesis. We report a patient with a GPA which was originally diagnosed as malignancy. (Gac Med Mex. 2016;152:468-74) Corresponding author: Gabriel Horta-Baas, [email protected] KEY WORDS: Granulomatosis with polyangiitis. Pseudotumor. Malignancy. Introduction Presentation of the case According to the 2012 revised Chapel Hill classifica- This is the case of a 39-year old male who was tion, granulomatosis with polyangiitis (GPA), previously admitted in the hospital presenting with asthenia, gen- known as Wegener’s granulomatosis (WG), is an auto- eral malaise, intermittent fever (3 to 4 times a month), immune systemic disease of unknown etiology, charac- diaphoresis with no time of day predominance and loss terized by necrotizing granulomatous inflammation of the of 10-kg weight in 6 months. -

USMLE – What's It
Purpose of this handout Congratulations on making it to Year 2 of medical school! You are that much closer to having your Doctor of Medicine degree. If you want to PRACTICE medicine, however, you have to be licensed, and in order to be licensed you must first pass all four United States Medical Licensing Exams. This book is intended as a starting point in your preparation for getting past the first hurdle, Step 1. It contains study tips, suggestions, resources, and advice. Please remember, however, that no single approach to studying is right for everyone. USMLE – What is it for? In order to become a licensed physician in the United States, individuals must pass a series of examinations conducted by the National Board of Medical Examiners (NBME). These examinations are the United States Medical Licensing Examinations, or USMLE. Currently there are four separate exams which must be passed in order to be eligible for medical licensure: Step 1, usually taken after the completion of the second year of medical school; Step 2 Clinical Knowledge (CK), this is usually taken by December 31st of Year 4 Step 2 Clinical Skills (CS), this is usually be taken by December 31st of Year 4 Step 3, typically taken during the first (intern) year of post graduate training. Requirements other than passing all of the above mentioned steps for licensure in each state are set by each state’s medical licensing board. For example, each state board determines the maximum number of times that a person may take each Step exam and still remain eligible for licensure. -
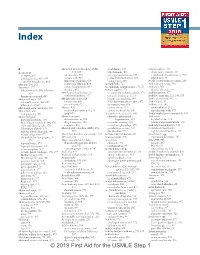
© 2019 First Aid for the USMLE Step 1 732 INDEX INDEX
Index A Abnormal uterine bleeding (AUB), heart failure, 306 Achondroplasia, 454 A-a gradient 618, 619 hypertension, 312 chromosome disorder, 64 in elderly, 654 adenomyosis, 634 naming convention for, 253 endochondral ossification in, 450 with hypoxemia, 654, 655 anemia with, 410 preload/afterload effects, 282 inheritance, 60 restrictive lung disease, 661 Asherman syndrome, 634 teratogenicity, 600 AChR (acetylcholine receptor), 229 Abacavir, 201, 203 leiomyoma (fibroid), 634 Acetaldehyde, 72 Acid-base physiology, 580 Abciximab, 122 polyps (endometrial), 634 Acetaldehyde dehydrogenase, 70, 72 Acidemia, 580 Glycoprotein IIb/IIIa inhibitors, thecoma, 632 Acetaminophen, 474 diuretic effect on, 595 429 ABO blood classification, 397 vs. aspirin for pediatric patients, 474 Acid-fast oocysts, 177 thrombogenesis and, 403 newborn hemolysis, 397 free radical injury and, 210 Acid-fast organisms, 125, 140, 155 Abdominal aorta, 357 Abruptio placentae, 626 hepatic necrosis from, 249 Acidic amino acids, 81 atherosclerosis in, 300, 687 cocaine use, 600 N-acetylcysteine for overdose, 671 Acid maltase, 86 bifurcation of, 649 preeclampsia, 629 for osteoarthritis, 458 Acidosis, 578, 580 Abdominal aortic aneurysm, 300 Abscess, 470 toxicity effects, 474 contractility in, 282 Abdominal colic acute inflammation and, 215 toxicity treatment for, 247 hyperkalemia with, 578 lead poisoning, 411 lung, 670 Acetazolamide, 252, 539, 594 Acid phosphatase in neutrophils, 398 Abdominal pain Absence seizures idiopathic intracranial Acid reflux bacterial peritonitis, 384 characteristics -

Pharmacology/Therapeutics Ii Block 1 Handouts – 2015-16
PHARMACOLOGY/THERAPEUTICS II BLOCK 1 HANDOUTS – 2015‐16 55. H2 Blockers, PPls – Moorman 56. Palliation of Contipation & Nausea/Vomiting – Kristopaitis 57. On‐Line Only – Principles of Clinical Toxicology – Kennedy 58. Anti‐Parasitic Agents – Johnson Histamine Antagonists and PPIs January 6, 2016 Debra Hoppensteadt Moorman, Ph.D. Histamine Antagonists and PPIs Debra Hoppensteadt Moorman, Ph.D. Office # 64625 Email: [email protected] KEY CONCEPTS AND LEARNING OBJECTIVES . 1 To understand the clinical uses of H2 receptor antagonists. 2 To describe the drug interactions associated with the use of H2 receptor antagonists. 3 To understand the mechanism of action of PPIs 4 To describe the adverse effects and drugs interactions with PPIs 5 To understand when the histamine antagonists and the PPIs are to be used for treatment 6 To describe the drugs used to treat H. pylori infection Drug List: See Summary Table. Histamine Antagonists and PPIs January 6, 2016 Debra Hoppensteadt Moorman, Ph.D. Histamine Antagonists and PPIs I. H2 Receptor Antagonists These drugs reduce gastric acid secretion, and are used to treat peptic ulcer disease and gastric acid hypersecretion. These are remarkably safe drugs, and are now available over the counter. The H2 antagonists are available OTC: 1. Cimetidine (Tagamet®) 2. Famotidine (Pepcid®) 3. Nizatidine (Axid®) 4. Ranitidine (Zantac®) All of these have different structures and, therefore, different side-effects. The H2 antagonists are rapidly and well absorbed after oral administration (bioavailability 50-90%). Peak plasma concentrations are reached in 1-3 hours, and the drugs have a t1/2 of 1-3 hours. H2 antagonists also inhibit stimulated (due to feeding, gastrin, hypoglycemia, vagal) acid secretion and are useful in controlling nocturnal acidity – useful when added to proton pump therapy to control “nocturnal acid breakthrough”. -

Developmental Venous Anomaly: MR and Angiographic Features
JBR–BTR, 2014, 97: 17-20. DEVELOPMENTAL VENOUS ANOMALY: MR AND ANGIOGRAPHIC FEATURES M. Faure1, M. Voormolen1, T. Van der Zijden1, P.M. Parizel1 Developmental venous anomaly (DVA) is probably the most common anomaly of the intracranial vasculature. DVAs consist of multiple, radially oriented dilated medullary veins that converge into a transcerebral vein. We describe the imaging findings of this vascular anomaly in different patients and the role of different imaging modalities. Key-words: Cerebral blood vessels, abnormalities – Cerebral blood vessels, MR – Cerebral angiography. Developmental venous anomaly (DVA) was first considered a rare vascular malformation (1, 2). Nowa- days, with the advent of Computed Tomography (CT) and especially Magnetic Resonance Imaging (MRI), DVAs are seen every week to month by radiologists (3, 4). Most DVAs are solitary, asymptomatic lesions and are discovered incidentally. They have a relatively benign nature with a low incidence of hemorrhage. When they do bleed, this is thought to be due to associated vascular mal- formations, like cavernous angiomas. The typical angiographic appearance of a DVA is a caput medusae appear- ance in the venous phase. MRI com- bined with MR angiography (MRA) replaces angiography in most un- A B complicated cases as a non-invasive alternative (3, 5). Case reports Case 1 A 32-year-old woman presented with headache, with no particular location and no neurological deficit. MRI of the brain was made in another hospital that showed a flow void running transcerebral, suggestive for a vascular malformation (Fig. 1A,B). Initially, there was no gadolinium contrast given and an arterial feeder could thus not be excluded with MRI. -

Rhinotillexomania in a Cystic Fibrosis Patient Resulting in Septal Perforation Mark Gelpi1*, Emily N Ahadizadeh1,2, Brian D’Anzaa1 and Kenneth Rodriguez1
ISSN: 2572-4193 Gelpi et al. J Otolaryngol Rhinol 2018, 4:036 DOI: 10.23937/2572-4193.1510036 Volume 4 | Issue 1 Journal of Open Access Otolaryngology and Rhinology CASE REPORT Rhinotillexomania in a Cystic Fibrosis Patient Resulting in Septal Perforation Mark Gelpi1*, Emily N Ahadizadeh1,2, Brian D’Anzaa1 and Kenneth Rodriguez1 1 Check for University Hospitals Cleveland Medical Center, USA updates 2Case Western Reserve University School of Medicine, USA *Corresponding author: Mark Gelpi, MD, University Hospitals Cleveland Medical Center, 11100 Euclid Avenue, Cleveland, OH 44106, USA, Tel: (216)-844-8433, Fax: (216)-201-4479, E-mail: [email protected] paranasal sinuses [1,4]. Nasal symptoms in CF patients Abstract occur early, manifesting between 5-14 years of age, and Cystic fibrosis (CF) is a multisystem disease that can have represent a life-long problem in this population [5]. Pa- significant sinonasal manifestations. Viscous secretions are one of several factors in CF that result in chronic sinona- tients with CF can develop thick nasal secretions con- sal pathology, such as sinusitis, polyposis, congestion, and tributing to chronic rhinosinusitis (CRS), nasal conges- obstructive crusting. Persistent discomfort and nasal man- tion, nasal polyposis, headaches, and hyposmia [6-8]. ifestations of this disease significantly affect quality of life. Sinonasal symptoms of CF are managed medically with Digital manipulation and removal of crusting by the patient in an attempt to alleviate the discomfort can have unfore- topical agents and antibiotics, however surgery can be seen damaging consequences. We present one such case warranted due to the chronic and refractory nature of and investigate other cases of septal damage secondary to the symptoms, with 20-25% of CF patients undergoing digital trauma, as well as discuss the importance of sinona- sinus surgery in their lifetime [8]. -

Retained Neonatal Reflexes | the Chiropractic Office of Dr
Retained Neonatal Reflexes | The Chiropractic Office of Dr. Bob Apol 12/24/16, 1:56 PM Temper tantrums Hypersensitive to touch, sound, change in visual field Moro Reflex The Moro Reflex is present at 9-12 weeks after conception and is normally fully developed at birth. It is the baby’s “danger signal”. The baby is ill-equipped to determine whether a signal is threatening or not, and will undergo instantaneous arousal. This may be due to sudden unexpected occurrences such as change in head position, noise, sudden movement or change of light or even pain or temperature change. This activates the stress response system of “fight or flight”. If the Moro Reflex is present after 6 months of age, the following signs may be present: Reaction to foods Poor regulation of blood sugar Fatigues easily, if adrenalin stores have been depleted Anxiety Mood swings, tense muscles and tone, inability to accept criticism Hyperactivity Low self-esteem and insecurity Juvenile Suck Reflex This is active together with the “Rooting Reflex” which allows the baby to feed and suck. If this reflex is not sufficiently integrated, the baby will continue to thrust their tongue forward, pushing on the upper jaw and causing an overbite. This by nature affects the jaw and bite position. This may affect: Chewing Difficulties with solid foods Dribbling Rooting Reflex Light touch around the mouth and cheek causes the baby’s head to turn to the stimulation, the mouth to open and tongue extended in preparation for feeding. It is present from birth usually to 4 months. -

Physical Esxam
Pearls in the Musculoskeletal Exam Frank Caruso MPS, PA-C, EMT-P Skin, Bones, Hearts & Private Parts 2019 Examination Key Points • Area that needs to be examined, gown your patients - well exposed • Understand normal functional anatomy • Observe normal activity • Palpation • Range of Motion • Strength/neuro-vascular assessment • Special Tests General Exam Musculoskeletal Overview Physical Exam Preview Watch Your Patients Walk!! Inspection • Posture – Erectness – Symmetry – Alignment • Skin and subcutaneous tissues – Swelling – Redness – Masses Inspection • Extremities – Size – Deformities – Enlargement – Alignment – Contour – Symmetry Inspection • Muscles – Bilateral symmetry – Hypertrophy – Atrophy – Fasciculations – Spasms Palpation • Palpate bones, joints, and surrounding muscles for the following: – Heat – Tenderness – Swelling – Fluctuation – Crepitus – Resistance to pressure – Muscle tone Muscles • Size and strength affected by the following: – Genetics – Exercise – Nutrition • Muscles move joints through range of motion (ROM). Muscle Strength • Compare bilateral muscles – Strength – Symmetry – Equality – Resistance End Feel Think About It!! • The sensation the examiner feels in the joint as it reaches the end of the range of motion of each passive movement • Bone to bone: This is hard, unyielding – normal would be elbow extension. • Soft–tissue approximation: yielding compression that stops further movement – elbow and knee flexion. End Feel • Tissue stretch: hard – springy type of movement with a slight give – toward the end of range of motion – most common type of normal end feel : knee extension and metacarpophalangeal joint extension. Abnormal End Feel • Muscle spasm: invoked by movement with a sudden dramatic arrest of movement often accompanied by pain - sudden hard – “vibrant twang” • Capsular: Similar to tissue stretch but it does not occur where one would expect – range of motion usually reduced. -
Intro to Pediatric HCC Module
A Message from Mark Baiada BAYADA Home Health Care has a special purpose—to help people have a safe home life with comfort, independence, and dignity. BAYADA will only succeed with your involvement and commitment as a member of our home health care team. I recognize your importance to the organization and appreciate your compassion, excellence, and reliability. I value the skills, expertise, and experience that you bring with you. And, as an organization, BAYADA is committed to providing you with opportunities to help broaden your expertise and experience. Acquiring new skills will allow you to participate in the care of a wider variety of clients. That makes you an increasingly valuable member of our home health care team. Most importantly, our clients benefit when you successfully master new skills that contribute to their safety and well-being. BAYADA University and the School of Nursing courses are designed to help you perfect your knowledge and skill to achieve clinical excellence in the care of clients. I applaud your willingness to continue the journey of life-long learning and wish you continued success in your professional development as an important member of the BAYADA team. Sincerely, Mark Baiada President Table of Contents Welcome ...........................................................................................................................iv Introduction to home care ................................................................................................. 1 Psychosocial .................................................................................................................. -

Venous Angiomas of the Brain A
- REVIEW ARTICLE systems," Venous angiomas may be Venous angiomas of quite small, draining a limited region of the brain, or may be very large, the brain a sometimes draining an entire hemi- • sphere. They can be single or multi- ple, and even bilateral.P" The com- review monest sites of occurrence are in the frontal and parietal lobes of the cere- venous anomaly' or DVA, pointing bral hemispheres and in the cerebel- Ian C Duncan out that these abnormalities actual- Ium.':" They can also be found in the ly represented an extreme anatomi- FFRad(D)SA occipital and temporal lobes, basal cal variant of the normal venous ganglia and pons." Unitas Interventional Unit POBox 14031 drainage of the brain. Lytlelton Imaging 0140 Pathology The classical radiographic appear- The theory of the development of ance of these abnormalities accurately venous angiomas is that there is fail- reflects the anatomical picture with Introduction ure of regression of normal embryon- multiple enlarged transmedullary Venous angiomas of the brain, also ic transmedullary venous channels. veins radiating in a wedge or radial termed venous malformations or These persistent transmedullary veins pattern toward the larger collecting developmental venous anomalies run axially through the white matter vein producing the pathognomic (DVA) are commonest of the to drain into a single larger calibre col- 'caput medusae' or 'spoke wheel' intracranial vascular malformations lecting venous trunk. The dilated ter- appearance during the venous phase comprising between 50% and 63% of minal collecting vein then penetrates of a cerebral angiogram (Figs 1,2).14,15 all intracranial vascular malforma- the cortex to drain either superficially A similar appearance is often seen on tions.