Basic Laboratory Tests Basic Urine Tests (Urinalysis)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Ketones, Urine
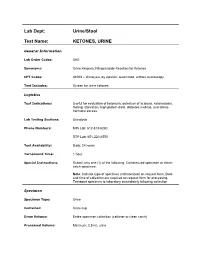
Lab Dept: Urine/Stool Test Name: KETONES, URINE General Information Lab Order Codes: UKE Synonyms: Urine Ketones; Nitroprusside Reaction for Ketones CPT Codes: 81003 – Urinalysis, by dipstick; automated, without microscopy Test Includes: Screen for urine ketones. Logistics Test Indications: Useful for evaluation of ketonuria, detection of acidosis, ketoacidosis, fasting, starvation, high protein diets, diabetes mellitus, and stress- hormone excess. Lab Testing Sections: Urinalysis Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 1 hour Special Instructions: Submit only one (1) of the following: Catheterized specimen or clean- catch specimen. Note: Indicate type of specimen (catheterized) on request form. Date and time of collection are required on request form for processing. Transport specimen to laboratory immediately following collection Specimen Specimen Type: Urine Container: Urine cup Draw Volume: Entire specimen collection (catheter or clean catch) Processed Volume: Minimum: 0.5 mL urine Collection: A specimen collected by catheterization is optimal; however, a clean- catch or mid-stream specimen is also acceptable. Random, voided specimens will be accepted, but are the least desirable and are not recommended if a urine culture is also being requested. Special Processing: N/A Patient Preparation: None Sample Rejection: Less than 0.5 mL urine submitted; mislabeled or unlabeled specimen Interpretive Reference Range: Negative Critical Values: N/A Limitations: Specimens containing -
Basic Skills in Interpreting Laboratory Data
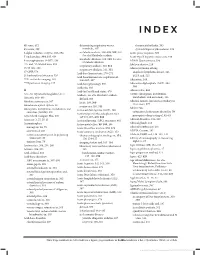
INDEX 4K score, 612 determining respiratory versus rheumatoid arthritis, 505 4Ts score, 399 metabolic, 307 systemic lupus erythematosus, 509 5-alpha reductase enzyme, 593–594 metabolic acidosis, 308–309, 309, 310. Acute phase response, 500 See also Metabolic acidosis 5' nucleotidase, 334, 335, 636 Acute type B hepatitis (minicase), 349 metabolic alkalosis, 309, 310. See also 6-mercaptopurine (6-MP), 138 ADAM Questionnaire, 596 Metabolic alkalosis 13C- and 14C-labeled urea, 353 Addison disease, 219 respiratory acidosis, 310, 311 15/15 rule, 208 Adenocarcinoma of lung respiratory alkalosis, 311, 311 17-OHP, 578 anaplastic lymphoma kinase, 526 Acid-base homeostasis, 270–271 21-hydroxylase deficiency, 526 EGFR and, 525 Acid-base homeostasis, regulation of, 99m Tc-sestamibi imaging, 165 306–307, 307 Adenosine, 164 201 TI perfusion imaging, 165 Acid-base physiology, 306 Adenosine diphosphate (ADP), 394, Acidemia, 303 394 A Acid-fast bacilli and stains, 470 Adenoviridae, 456 A1c. See Glycated hemoglobin (A1c) Acidosis. See also Metabolic acidosis ADME (absorption, distribution, metabolism, and excretion), 136 Abacavir, 468–469 defined, 303 Adnexal tumors, hirsutism secondary to Absolute neutropenia, 387 lactic, 308, 309 (minicase), 577 Absorbance optical system, 28 respiratory, 310, 311 Adolescents Absorption, distribution, metabolism, and Activated clotting time (ACT), 408 excretion (ADME), 136 categories of substances abused by, 70 Activated partial thromboplastin time prerequisite drug testing of, 82–83 Accu Check Compact Plus, 200 (aPTT), -

Bilirubin (Urine) Interpretive Summary
Bilirubin (Urine) Interpretive Summary Description: Bilirubinuria is an indicator of conjugated bilirubin in the urine. Excessive bilirubinuria in a dog or any bilirubinuria in a cat is an indication to evaluate serum bilirubin concentrations. Decreased Bilirubin Common Causes Normal Artifact o Exposure to UV light or room air o Delayed analysis o Centrifugation of urine prior to analysis o Ascorbic acid (Vitamin C) Increased Bilirubin Common Causes Normal dogs (especially males with concentrated urine) Liver disease, bile duct obstruction RBC destruction (hemolysis) o Immune-mediated hemolytic anemia o Zinc or onion toxicity o RBC parasites Uncommon Causes Hemoglobinuria Fever Prolonged anorexia False positive reactions due to medications o Phenothiazines (e.g., chlorpromazine) o Etodolac Related Findings Liver disease, biliary obstruction o Increased serum bilirubin, ALT, ALP, GGT, AST o Increased serum bile acids o Decreased albumin, cholesterol, BUN and glucose in severe cases o Abnormalities in liver and/or biliary tract on abdominal ultrasound RBC destruction o Decreased hematocrit, RBC, hemoglobin o Increased reticulocytes, increased MCV and decreased MCHC, polychromasia o Increased serum bilirubin o Spherocytosis (in dogs), autoagglutination o Hemoglobinuria o Positive Coombs or saline agglutination test may or may not be present with IMHA Generated by VetConnect® PLUS: Bilirubin (Urine) Page 1 of 2 Additional Information Physiology Conjugated bilirubin passes freely through the glomerular filtration barrier and is excreted in urine. Unconjugated bilirubin is bound to albumin and does not normally pass through the glomerular filtration barrier. Therefore, it is not detectable in urine (unless albuminuria or glomerular disease is present). Bilirubinuria usually precedes hyperbilirubinemia and icterus Dogs: Clinically normal dogs (especially males) may have detectable bilirubinuria in concentrated urine due to a low renal threshold for bilirubin. -

Leukocyte Esterase Activity in Vaginal Fluid of Pregnant and Non-Pregnant Women with Vaginitis/Vaginosis and in Controls
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by PubMed Central Infect Dis Obstet Gynecol 2003;11:19–26 Leukocyte esterase activity in vaginal fluid of pregnant and non-pregnant women with vaginitis/vaginosis and in controls Per-Anders Mårdh 1, Natalia Novikova 1, Ola Niklasson 1, Zoltan Bekassy 1 and Lennart Skude 2 1Department of Obstetrics and Gynecology, University Hospital, Lund and 2Department of Clinical Chemistry, County Hospital, Halmstad, Sweden Objectives: Todeterminethe leukocyteesterase (LE) activity invaginal lavage fluid ofwomen with acuteand recurrentvulvovaginal candidosis (VVC and RVVC respectively), bacterial vaginosis(BV), and in pregnant and non-pregnantwomen without evidenceof the threeconditions. Also tocompare the resultof LEtestsin women consultingat differentweeks inthe cycle andtrimesters of pregnancy.The LEactivity was correlatedto vaginal pH, numberof inflammatory cells instained vaginal smears,type of predominatingvaginal bacteria andpresence of yeast morphotypes. Methods: Onehundred and thirteen women with ahistoryof RVVC,i.e. with at least fourattacks of the conditionduring the previousyear and who had consultedwith anassumed new attack ofthe condition,were studied.Furthermore, we studied16 women with VVC,15 women with BV,and 27 women attendingfor control of cytological abnormalities, who all presentedwithout evidenceof either vaginitisor vaginosis. Finally, 73 pregnantwomen wereinvestigated. The LEactivity invaginal fluid duringdifferent weeks inthe cycle of 53 of the women was measured. Results: Inthe non-pregnantwomen, anincreased LE activity was foundin 96, 88, 73 and56% of those with RVVC,VVC and BV andin the non-VVC/BVcases,respectively. In 73% of pregnantwomen inthe second trimester,and 76% of thosein the third,the LEtestwas positive.In all groupsof non-pregnantwomen tested, the LEactivity correlatedwith the numberof leukocytesin vaginal smears,but it didnot in those who were pregnant.There was nocorrelation between LE activity andweek incycle. -

Proteinuria and Bilirubinuria As Potential Risk Indicators of Acute Kidney Injury During Running in Outpatient Settings
medicina Article Proteinuria and Bilirubinuria as Potential Risk Indicators of Acute Kidney Injury during Running in Outpatient Settings Daniel Rojas-Valverde 1,2,* , Guillermo Olcina 2,* , Braulio Sánchez-Ureña 3 , José Pino-Ortega 4 , Ismael Martínez-Guardado 2 and Rafael Timón 2,* 1 Centro de Investigación y Diagnóstico en Salud y Deporte (CIDISAD), Escuela Ciencias del Movimiento Humano y Calidad de Vida (CIEMHCAVI), Universidad Nacional, Heredia 86-3000, Costa Rica 2 Grupo en Avances en el Entrenamiento Deportivo y Acondicionamiento Físico (GAEDAF), Facultad Ciencias del Deporte, Universidad de Extremadura, 10005 Cáceres, Spain; [email protected] 3 Programa Ciencias del Ejercicio y la Salud (PROCESA), Escuela Ciencias del Movimiento Humano y Calidad de Vida (CIEMHCAVI), Universidad Nacional, Heredia 86-3000, Costa Rica; [email protected] 4 Departmento de Actividad Física y Deporte, Facultad Ciencias del Deporte, 30720 Murcia, Spain; [email protected] * Correspondence: [email protected] (D.R.-V.); [email protected] (G.O.); [email protected] (R.T.); Tel.: +506-8825-0219 (D.R.-V.) Received: 2 September 2020; Accepted: 19 October 2020; Published: 27 October 2020 Abstract: Background and objectives: The purpose of this study was to explore which urinary markers could indicate acute kidney injury (AKI) during prolonged trail running in outpatient settings. Materials and Methods: Twenty-nine experienced trail runners (age 39.1 8.8 years, weight 71.9 11 kg, ± ± height 171.9 8.3 cm) completed a 35 km event (cumulative positive ascend of 1815 m, altitude = 906 to ± 1178 m.a.s.l.) under a temperature of 25.52 1.98 C and humidity of 79.25 7.45%). -

Surgeons, Columbia University, New York City) (Received for Publication August 9, 1932)
THE ADDIS SEDIMENT COUNT IN NORMAL CHILDREN By JOHN D. LYTTLE (From the Babies Hospit and the Department of Pediatrics, Colege of Physicians and Surgeons, Columbia University, New York City) (Received for publication August 9, 1932) THE METHOD In 1925 Addis (1) described a method by which, in a concentrated acid urine, the rate of excretion of protein, casts and red and white cells could be determined. His method, with certain modifications, has been followed here. All of the counts were made on the 12 hour night specimen from 7 or 8 P.M. to 7 or 8 A.M. Addis recommended that fluids be restricted during, and for 12 hours preceding the collection, since in dilute and alkaline urine hyaline casts dissolve and red cells may be completely lysed. With children this rigid restriction of fluid proved impossible. Withholding fluid during the afternoon and night except for 200 cc. at the evening meal, gave urines of such concentration and acidity that they were suitable for a count. Most children had an early supper and col- lections were started at 7 or 8 P.M. Under these conditions, the urinary pH was between 5.0 and 6.0 and the specific gravity usually well above 1.020. The specimens were treated as described by Addis: "the con- centrated night urine is thoroughly mixed by repeated inversion of the rubber-stoppered bottle and a 10 cc. sample is transferred to a special graduated tube, and centrifugalized for five minutes at 1,800 revolutions per minute. The supernatant urine is decanted and pipetted down to a known volume which varies with the amount of sediment as judged by direct observation. -

Different Response of Body Weight Change According to Ketonuria After Fasting in the Healthy Obese
ORIGINAL ARTICLE Endocrinology, Nutrition & Metabolism http://dx.doi.org/10.3346/jkms.2012.27.3.250 • J Korean Med Sci 2012; 27: 250-254 Different Response of Body Weight Change According to Ketonuria after Fasting in the Healthy Obese Hyeon-Jeong Kim1, Nam-Seok Joo1, The relationship between obesity and ketonuria is not well-established. We conducted a Kwang-Min Kim1, Duck-Joo Lee1, retrospective observational study to evaluate whether their body weight reduction response and Sang-Man Kim2 differed by the presence of ketonuria after fasting in the healthy obese. We used the data of 42 subjects, who had medical records of initial urinalysis at routine health check-up and 1Department of Family Practice and Community Health, Ajou University School of Medicine, Suwon; follow-up urinalysis in the out-patient clinic, one week later. All subjects in the initial 2Department of Family Medicine, CHA Biomedical urinalysis showed no ketonuria. However, according to the follow-up urinalysis after three Center, CHA University College of Medicine, Seoul, subsequent meals fasts, the patients were divided into a non-ketonuria group and Korea ketonuria group. We compared the data of conventional low-calorie diet programs for ± Received: 20 August 2011 3 months for both groups. Significantly greater reduction of body weight (-8.6 3.6 kg vs 2 2 Accepted: 17 January 2012 -1.1 ± 2.2 kg, P < 0.001), body mass index (-3.16 ± 1.25 kg/m vs -0.43 ± 0.86 kg/m , P < 0.001) and waist circumference (-6.92 ± 1.22 vs -2.32 ± 1.01, P < 0.001) was Address for Correspondence: observed in the ketonuria group compared to the non-ketonuria group. -

Deficient Diabetic Mice
Diminished Loss of Proteoglycans and Lack of Albuminuria in Protein Kinase C-␣–Deficient Diabetic Mice Jan Menne,1,2 Joon-Keun Park,2 Martin Boehne,2 Marlies Elger,2 Carsten Lindschau,2 Torsten Kirsch,2 Matthias Meier,2 Faikah Gueler,2 Annette Fiebeler,3 Ferdinand H. Bahlmann,2 Michael Leitges,4 and Hermann Haller2 Activation of protein kinase C (PKC) isoforms has been implicated in the pathogenesis of diabetic nephropathy. We showed earlier that PKC-␣ is activated in the kid- iabetes affects Ͼ300 million people worldwide; -neys of hyperglycemic animals. We now used PKC-␣؊/؊ 20–40% will develop overt nephropathy. Diabe mice to test the hypothesis that this PKC isoform tes is the most common cause of end-stage mediates streptozotocin-induced diabetic nephropathy. Drenal disease. The earliest clinical sign of ne- We observed that renal and glomerular hypertrophy was phropathy is microalbuminuria. Microalbuminuria also ؊ ؊ similar in diabetic wild-type and PKC-␣ / mice. How- heralds impending cardiovascular morbidity and mortality ever, the development of albuminuria was almost absent (1–4). Microalbuminuria predicts overt proteinuria, which ؊/؊␣ in the diabetic PKC- mice. The hyperglycemia-in- is now believed to actively promote renal insufficiency (5). duced downregulation of the negatively charged base- Therefore, successful treatment of diabetic patients ment membrane heparan sulfate proteoglycan perlecan -؊ ؊ should aim for the prevention or regression of albumin was completely prevented in the PKC-␣ / mice, com- pared with controls. We then asked whether transform- uria. Hyperglycemia seems to cause microalbuminuria in   diabetic patients (6,7). However, how the metabolic dis- ing growth factor- 1 (TGF- 1) and/or vascular endothelial growth factor (VEGF) is implicated in the turbance causes cellular effects is incompletely under- PKC-␣–mediated changes in the basement membrane. -

Ileal Neobladder: an Important Cause of Non-Anion Gap Metabolic Acidosis
The Journal of Emergency Medicine, Vol. 52, No. 5, pp. e179–e182, 2017 Ó 2017 Elsevier Inc. All rights reserved. 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2016.12.036 Clinical Communications: Adult ILEAL NEOBLADDER: AN IMPORTANT CAUSE OF NON-ANION GAP METABOLIC ACIDOSIS Jesse W. St. Clair, MD and Matthew L. Wong, MD, MPH Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, Massachusetts and Department of Emergency Medicine, Harvard Medical School, Boston, Massachusetts Reprint Address: Matthew L. Wong, MD, MPH, Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Rosenberg Building, 2nd Floor, 1 Deaconess Road, Boston, MA 02446 , Abstract—Background: The differential diagnosis for a disease, or medications such as acetazolamide. non-anion gap metabolic acidosis is probably less well Commonly used mnemonics to remember the differential known than the differential diagnosis for an anion gap for the non-anion gap metabolic acidosis include metabolic acidosis. One etiology of a non-anion gap acidosis ‘‘ABCD’’ for ‘‘Addison’s, Bicarbonate loss, Chloride is the consequence of ileal neobladder urinary diversion (administration), and Drugs,’’ as well as ‘‘HARDUP’’ for the treatment of bladder cancer. Case Report: We pre- for ‘‘Hyperchloremia, Acetazolamide and Addison’s, sent a case of a patient with an ileal neobladder with a severe non-anion gap metabolic acidosis caused by a Renal Tubular Acidosis, Diarrhea, Ureteroenterostomies, urinary tract infection and ureteroenterostomy. Why and Pancreaticoenterostomies’’ (Table 1) (1). Should an Emergency Physician Be Aware of This?: Part Ureteroenterostomies are when the ureter has an of the ileal neobladder surgery includes ureteroenteros- abnormal connection with a segment of intestine. -
Interpretation of Canine and Feline Urinalysis
$50. 00 Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Preface Urine is that golden body fluid that has the potential to reveal the answers to many of the body’s mysteries. As Thomas McCrae (1870-1935) said, “More is missed by not looking than not knowing.” And so, the authors would like to dedicate this handbook to three pioneers of veterinary nephrology and urology who emphasized the importance of “looking,” that is, the importance of conducting routine urinalysis in the diagnosis and treatment of diseases of dogs and cats. To Dr. Carl A. Osborne , for his tireless campaign to convince veterinarians of the importance of routine urinalysis; to Dr. Richard C. Scott , for his emphasis on evaluation of fresh urine sediments; and to Dr. Gerald V. Ling for his advancement of the technique of cystocentesis. Published by The Gloyd Group, Inc. Wilmington, Delaware © 2004 by Nestlé Purina PetCare Company. All rights reserved. Printed in the United States of America. Nestlé Purina PetCare Company: Checkerboard Square, Saint Louis, Missouri, 63188 First printing, 1998. Laboratory slides reproduced by permission of Dennis J. Chew, DVM and Stephen P. DiBartola, DVM. This book is protected by copyright. ISBN 0-9678005-2-8 Table of Contents Introduction ............................................1 Part I Chapter 1 Sample Collection ...............................................5 -

A Dipstick Test Combined with Urine Specific Gravity Improved the Accuracy of Proteinuria Determination in Pregnancy Screening
Kobe J. Med. Sci., Vol. 56, No. 4, pp. E165-E172, 2010 A Dipstick Test Combined with Urine Specific Gravity Improved the Accuracy of Proteinuria Determination in Pregnancy Screening NATSUKO MAKIHARA1, MINEO YAMASAKI1,2, HIROKI MORITA1, and HIDETO YAMADA1* 1Division of Obstetrics and Gynecology, Department of Surgery-related, and 2Division of Integrated Medical Education, Department of Community Medicine and Social Healthcare Science, Kobe University Graduate School of Medicine, 7-5-1 Kusunoki-cho, Chuo-ku, Kobe, 650-0017, Japan. Received 12 July 2010/ Accepted 20 August 2010 Key Words: dipstick test, pregnancy proteinuria, protein/creatinine ratio, urine specific gravity Proteinuria screening using a semi-quantitative dipstick test of the spot urine in antenatal clinic is known to have high false-positive rates. The aim of this study was to assess availability of a dipstick test combined with the urine specific gravity for the determination of pathological proteinuria. A dipstick test was performed on 582 urine samples obtained from 283 pregnant women comprising 260 with normal blood pressure and 23 with pregnancy-induced hypertension. The urine protein (P) and creatinine (C) concentrations, specific gravity (SG), P/C ratio were determined, and compared with dipstick test results. The P concentration increased along the stepwise augmentations in dipstick test result. Frequencies of the urine samples with 0.265 or more P/C ratio were 0.7% with − dipstick test result, 0.7% with the ± result, 3.3% with the 1+ result, and 88.9% with the ≥2+ result. However, if the urine specific gravity was low, frequencies of the high P/C ratio were 5.0% with ± dipstick test result and 9.3% with the 1+ result. -

Paroxysmal Nocturnal Hemoglobinuria
Paroxysmal nocturnal hemoglobinuria Description Paroxysmal nocturnal hemoglobinuria is an acquired disorder that leads to the premature death and impaired production of blood cells. The disorder affects red blood cells (erythrocytes), which carry oxygen; white blood cells (leukocytes), which protect the body from infection; and platelets (thrombocytes), which are involved in blood clotting. Paroxysmal nocturnal hemoglobinuria affects both sexes equally, and can occur at any age, although it is most often diagnosed in young adulthood. People with paroxysmal nocturnal hemoglobinuria have sudden, recurring episodes of symptoms (paroxysmal symptoms), which may be triggered by stresses on the body, such as infections or physical exertion. During these episodes, red blood cells are prematurely destroyed (hemolysis). Affected individuals may pass dark-colored urine due to the presence of hemoglobin, the oxygen-carrying protein in blood. The abnormal presence of hemoglobin in the urine is called hemoglobinuria. In many, but not all cases, hemoglobinuria is most noticeable in the morning, upon passing urine that has accumulated in the bladder during the night (nocturnal). The premature destruction of red blood cells results in a deficiency of these cells in the blood (hemolytic anemia), which can cause signs and symptoms such as fatigue, weakness, abnormally pale skin (pallor), shortness of breath, and an increased heart rate. People with paroxysmal nocturnal hemoglobinuria may also be prone to infections due to a deficiency of white blood cells. Abnormal platelets associated with paroxysmal nocturnal hemoglobinuria can cause problems in the blood clotting process. As a result, people with this disorder may experience abnormal blood clotting (thrombosis), especially in large abdominal veins; or, less often, episodes of severe bleeding (hemorrhage).