134Xxx Spums Contents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(Ua) Scientific Diving Safety Manual
UNIVERSITY OF ALASKA (UA) SCIENTIFIC DIVING SAFETY MANUAL AVAILABLE ON-LINE AT: http://www.uaf.edu/sfos/research/scientific-diving/ Revised 2/2019 Page 1 FOREWORD Since 1951 the scientific diving community has endeavored to promote safe, effective diving through self-imposed diver training and education programs. Over the years, manuals for diving safety have been circulated between organizations, revised and modified for local implementation, and have resulted in an enviable safety record. This document represents the minimal safety standards for scientific diving at the present day. As diving science progresses so must this standard, and it is the responsibility of every member of the Academy to see that it always reflects state of the art, safe diving practice. The policies, procedures and standards set forth in this Scientific Diving Safety Manual are intended to govern the training and diving operations of all personnel participating in the Scientific Diving Program at the University of Alaska (UA). It applies to all divers operating under UA auspices, including visiting divers, and to those UA Fairbanks, UA Anchorage, and UA Southeast campus officers responsible for the administration of this scuba program. Revision History May 1 1991 Revision July 1992 Revision January 1996 Revision January 2001 Revision May 2004 Revision January 2013 Revision October 2015 Revision February 2016 Revision May 2018 Revision February 2019 Revised 2/2019 Page 2 UNIVERSITY OF ALASKA DIVING CONTROL BOARD MEMBERS Brenda Konar (Dive Safety Officer) Joel Markis Professor Assistant Professor of Fisheries Technology University of Alaska Fairbanks Career Education Fairbanks, Alaska University of Alaska Southeast Phone: 907-474-5028 Sitka, Alaska E-mail: [email protected] Phone: 907-747-7760 E-mail: [email protected] Sherry Tamone (Chair) Tracey Martinson Professor of Biology University of Alaska Southeast Industrial Hygienist/Radiation Safety Officer Juneau, Alaska Environ. -
2008 June;38(2)
9^k^c\VcY=neZgWVg^XBZY^X^cZKdajbZ(-Cd#'?jcZ'%%- EJGEDH:HD;I=:HD8>:I>:H IdegdbdiZVcY[VX^a^iViZi]ZhijYnd[VaaVheZXihd[jcYZglViZgVcY]neZgWVg^XbZY^X^cZ Idegdk^YZ^c[dgbVi^dcdcjcYZglViZgVcY]neZgWVg^XbZY^X^cZ IdejWa^h]V_djgcVaVcYidXdckZcZbZbWZghd[ZVX]HdX^ZinVccjVaanViVhX^Zci^ÄXXdc[ZgZcXZ HDJI=E68>;>8JC9:GL6I:G :JGDE:6CJC9:GL6I:G6C9 B:9>8>C:HD8>:IN 76GDB:9>86AHD8>:IN D;;>8:=DA9:GH D;;>8:=DA9:GH EgZh^YZci EgZh^YZci 9gB^`Z7ZccZii 1B#7ZccZii5jchl#ZYj#Vj3 Egd[#6a[7gjWV`` 1Va[#d#WgjWV``5cicj#cd3 EVhiçEgZh^YZci K^XZEgZh^YZci 9g8]g^h6Xdii 1XVXdii5deijhcZi#Xdb#Vj3 9gEZiZg<Zgbdceg 1eZiZg#\ZgbdcegZ5b^a#WZ3 HZXgZiVgn >bbZY^ViZEVhiEgZh^YZci 9gHVgV]AdX`aZn 1hejbhhZXgZiVgn5\bV^a#Xdb3 9gCdZb^7^iiZgbVc 1cdZb^W5im#iZX]c^dc#VX#^a3 IgZVhjgZg EVhiEgZh^YZci 9g<jnL^aa^Vbh 1hejbh5[VhibV^a#cZi3 9gGVb^gd8Va^"8dgaZd 1^gdXVa^5YVcZjgdeZ#dg\3 :YjXVi^dcD[ÄXZg =dcdgVgnHZXgZiVgn 9g9Vk^YHbVgi 1YVk^Y#hbVgi5Y]]h#iVh#\dk#Vj3 9g?dZg\HX]bjio 1_dZg\#hX]bjio5]^c#X]3 EjWa^XD[ÄXZg BZbWZgViAVg\Z'%%, 9gKVcZhhV=VaaZg 1kVcZhhV#]VaaZg5XYbX#Xdb#Vj3 9gE]^a7gnhdc 1e]^a#Wgnhdc5YYgX#dg\3 8]V^gbVc6CO=B< BZbWZgViAVg\Z'%%+ 9g9Vk^YHbVgi 1YVk^Y#hbVgi5Y]]h#iVh#\dk#Vj3 Egd[#BV^YZ8^bh^i 1bX^bh^i5^hiVcWja#ZYj#ig3 8dbb^iiZZBZbWZgh BZbWZgViAVg\Z'%%* 9g<aZc=Vl`^ch 1]Vl`ZnZ5hl^[iYha#Xdb#Vj3 9g6gb^c@ZbbZg 1Vgb^c5`ZbbZgh#YZ3 9gHVgV]H]Vg`Zn 1hVgV]#h]Vg`Zn5YZ[ZcXZ#\dk#Vj3 9gHXdiiHfj^gZh 1hXdii#hfj^gZh5YZ[ZcXZ#\dk#Vj3 69B>C>HIG6I>DC 69B>C>HIG6I>DC BZbWZgh]^e =dcdgVgnIgZVhjgZgBZbWZgh]^eHZXgZiVgn HiZkZ<dWaZ 1hejbhVYb5W^\edcY#cZi#Vj3 EVig^X^VLddY^c\ &+7jghZab6kZcjZ!=V^cVjai!>a[dgY B:B7:GH=>E :hhZm!><+(:=!Jc^iZY@^c\Ydb -

Public Safety Scuba Diving
Industry Guide 47 A Guide to Public Safety Diving N.C. Department of Labor Occupational Safety and Health Division N.C. Department of Labor 1101 Mail Service Center Raleigh, NC 27699-1101 Cherie Berry Commissioner of Labor N.C. Department of Labor Occupational Safety and Health Program Cherie Berry Commissioner of Labor OSHA State Plan Designee Kevin Beauregard Deputy Commissioner for Safety and Health Scott Mabry Assistant Deputy Commissioner for Safety and Health Tom Savage Standards Officer Author Acknowledgments A Guide to Public Safety Diving has been prepared with materials and information from the General Industry Standards, 29 CFR 1910, Subpart T—Commercial Diving Operations, and OSHA Instruction CPL 02-00-151 (U.S. Department of Labor, Occupational Safety and Health Administration). This guide also contains information from sources such as U.S. Navy Diving Manual, National Association of Search and Rescue, California Department Fish and Game Diving Safety Manual, and the National Fire Protection Association, NFPA 1670—Standard on Operations and Technical Search and Rescue. Through an existing alliance established between the N.C. Department of Labor’s Occupational Safety and Health Divi- sion and the North Carolina Public Safety Divers’ Association (PSDA), a collaborative effort was established to make this guide possible. The PSDA board of directors provided expertise involving public safety diving in sharing best practices and technical knowledge. A special thanks to Chuck Elgin, North Carolina Underwater Response Team, for his dedication and hard work assisting in the development of this publication. This guide is intended to be consistent with all existing OSHA standards; therefore, if an area is considered by the reader to be inconsistent with a standard, then the OSHA standard should be followed. -

Rebreathers Open Inspiration Fully Closed Rebreather What Is It Like? Text & Photos by Peter Symes Diving Rebreathers Why Bother?
WWW.AQUALUNG.COM Dräger Ray semiclosed rebreather. Behind, an Rebreathers open Inspiration fully closed rebreather What is it like? WWW.AMBIENTPRESSUREDIVING.COM Text & photos by Peter Symes Diving Rebreathers Why bother? Rebreathers look cool, glitzy, tech- they provide for a much differ- nical and heralded as the future of ent and richer diving experience, which, in the first place, is why we go in diving, right? We read a lot about the water ourselves rather than watch- their impressive performances con- ing dive movies on Animal Planet from cerning duration of dives, gas econ- the comfort of our reclining chair at home. omy, extended no deco limits and However, as we all know, there is no such thing as a free lunch in diving either. There is what not. But isn’t it a bit like watch- a trade-off, and you will have to consider if it the underwater realm so you can have an ing Jeremy Clarkson from BBC’s car is still worth your while despite this. enriching experience by witnessing, first program, Top Gear, whiz around in It is not merely a matter of comparing hand, this magic realm. So, as far as I am fancy Ferraris and Aston Martins with technical matters, performance and param- concerned, if someone invented human eters when pitting rebreathers against the gills and a thin hide to cover and keep me a goofy, happy grin on his face and open circuits (regulators and tanks). It is warm, my twin-set would surely be left to rust reeling off a string of excited super- easy to be blinded by dazzling numbers and in the attic for good. -

Diving Safety Manual Revision 3.2
Diving Safety Manual Revision 3.2 Original Document: June 22, 1983 Revision 1: January 1, 1991 Revision 2: May 15, 2002 Revision 3: September 1, 2010 Revision 3.1: September 15, 2014 Revision 3.2: February 8, 2018 WOODS HOLE OCEANOGRAPHIC INSTITUTION i WHOI Diving Safety Manual DIVING SAFETY MANUAL, REVISION 3.2 Revision 3.2 of the Woods Hole Oceanographic Institution Diving Safety Manual has been reviewed and is approved for implementation. It replaces and supersedes all previous versions and diving-related Institution Memoranda. Dr. George P. Lohmann Edward F. O’Brien Chair, Diving Control Board Diving Safety Officer MS#23 MS#28 [email protected] [email protected] Ronald Reif David Fisichella Institution Safety Officer Diving Control Board MS#48 MS#17 [email protected] [email protected] Dr. Laurence P. Madin John D. Sisson Diving Control Board Diving Control Board MS#39 MS#18 [email protected] [email protected] Christopher Land Dr. Steve Elgar Diving Control Board Diving Control Board MS# 33 MS #11 [email protected] [email protected] Martin McCafferty EMT-P, DMT, EMD-A Diving Control Board DAN Medical Information Specialist [email protected] ii WHOI Diving Safety Manual WOODS HOLE OCEANOGRAPHIC INSTITUTION DIVING SAFETY MANUAL REVISION 3.2, September 5, 2017 INTRODUCTION Scuba diving was first used at the Institution in the summer of 1952. At first, formal instruction and proper information was unavailable, but in early 1953 training was obtained at the Naval Submarine Escape Training Tank in New London, Connecticut and also with the Navy Underwater Demolition Team in St. -

Using Underwater Pulse Oximetry in Freediving to Extreme Depths to Study Risk of Hypoxic Blackout and Diving Response Phases
ORIGINAL RESEARCH published: 01 April 2021 doi: 10.3389/fphys.2021.651128 Using Underwater Pulse Oximetry in Freediving to Extreme Depths to Study Risk of Hypoxic Blackout and Diving Response Phases Eric Mulder 1* and Erika Schagatay 1,2 1 Environmental Physiology Group, Department of Health Sciences, Mid Sweden University, Östersund, Sweden, 2 Swedish Winter Sports Research Centre, Mid Sweden University, Östersund, Sweden Deep freediving exposes humans to hypoxia and dramatic changes in pressure. The effect of depth on gas exchange may enhance risk of hypoxic blackout (BO) during the last part of the ascent. Our aim was to investigate arterial oxygen saturation (SpO2) and heart rate Edited by: (HR) in shallow and deep freedives, central variables, which have rarely been studied Costantino Balestra, underwater in deep freediving. Four male elite competitive freedivers volunteered to wear Haute École Bruxelles-Brabant (HE2B), Belgium a newly developed underwater pulse oximeter for continuous monitoring of SpO2 and HR Reviewed by: during self-initiated training in the sea. Two probes were placed on the temples, connected Neal William Pollock, to a recording unit on the back of the freediver. Divers performed one “shallow” and one Laval University, Canada Kay Tetzlaff, “deep” constant weight dive with fins. Plethysmograms were recorded at 30 Hz, and University Hospital of Tübingen, SpO2 and HR were extracted. Mean ± SD depth of shallow dives was 19 ± 3 m, and Germany 73 ± 12 m for deep dives. Duration was 82 ± 36 s in shallow and 150 ± 27 s in deep Claus-Martin Muth, Universitaetsklinikum Ulm, Germany dives. All divers desaturated more during deeper dives (nadir 55 ± 10%) compared to *Correspondence: shallow dives (nadir 80 ± 22%) with a lowest SpO2 of 44% in one deep dive. -
Supervised Dive
EFFECTIVE 1 March 2009 MINIMUM COURSE CONTENT FOR Supervised Diver Certifi cation As Approved By ©2009, Recreational Scuba Training Council, Inc. (RSTC) Recreational Scuba Training Council, Inc. RSTC Coordinator P.O. Box 11083 Jacksonville, FL 32239 USA Recreational Scuba Training Council (RSTC) Minimum Course Content for Supervised Diver Certifi cation 1. Scope and Purpose This standard provides minimum course content requirements for instruction leading to super- vised diver certifi cation in recreational diving with scuba (self-contained underwater breathing appa- ratus). The intent of the standard is to prepare a non diver to the point that he can enjoy scuba diving in open water under controlled conditions—that is, under the supervision of a diving professional (instructor or certifi ed assistant – see defi nitions) and to a limited depth. These requirements do not defi ne full, autonomous certifi cation and should not be confused with Open Water Scuba Certifi cation. (See Recreational Scuba Training Council Minimum Course Content for Open Water Scuba Certifi ca- tion.) The Supervised Diver Certifi cation Standards are a subset of the Open Water Scuba Certifi cation standards. Moreover, as part of the supervised diver course content, supervised divers are informed of the limitations of the certifi cation and urged to continue their training to obtain open water diver certifi - cation. Within the scope of supervised diver training, the requirements of this standard are meant to be com- prehensive, but general in nature. That is, the standard presents all the subject areas essential for su- pervised diver certifi cation, but it does not give a detailed listing of the skills and information encom- passed by each area. -

2021 WA Dive
DIVING 1 - 5 dives Per dive from the first dive 115 6 - 10 dives Per dive from the first dive 110 11 - 20 dives Per dive from the first dive 100 21 dives & upwards Per dive from the first dive 90 Orientation dive Per person 90 Night dive supplement Per dive in addition to the diving rate 20 EXTRA GUIDING FEE Private divemaster Per divemaster - half day / full day 250 / 350 Private instructor Per instructor - half day / full day 350 / 450 ◼ Tank, weights, surface marker buoy and surface alert horns are included in all diving activities ◼ Enriched air nitrox is available at no extra charge. This benefit applies to enriched air certified divers only EQUIPMENT RENTAL Mask, snorkel, fins, deluxe carrying bag Complimentary Full scuba set - includes dive computer, bcd, wetsuit & regulator Per dive 25 Dive computer | BCD jacket | Wetsuit | Regulator | Dive torch Per item per dive 10 Prescription mask Per day 15 PRIVATE DIVING Single dive - 1 / 2 / 3 / 4 persons 1245 / 1365 / 1615 / 1735 Double dives - 1 / 2 / 3 / 4 persons 2490 / 2730 / 3230 / 3470 Discover scuba diving - 1 / 2 / 3 / 4 persons 995 / 1465 / 1935 / 2405 ◼ By speedboat - full equipment, guides | instructor ◼ The use of dive computers, surface marker buoys & surface alert horns is mandatory ◼ Maximum diving depth limit is 30m and decompression diving is strictly prohibited ◼ A 24 hour no diving before flying period must be observed prior to departure PADI PROGRAMS FOR BEGINNERS PADI Bubblemaker - 8 to 10 yrs old Per person 120 PADI Seal team mission Theory + 1 lagoon session (per -
2020 Instructor Manual
INSTRUCTOR MANUAL Product No. 79173 (Rev. 12/19) Version 2020 © PADI 2020 PADI INSTRUCTOR MANUAL PADI® Instructor Manual © PADI 2020 No part of this product may be reproduced, sold or distributed in any form without the written permission of the publisher. ® indicates a trademark is registered in the U.S. and certain other countries. Published by PADI 30151 Tomas Rancho Santa Margarita, CA 92688-2125 USA Printed in USA Product No. 79173 (Rev. 12/19) Version 2020 Scuba diving can never be entirely risk-free. However, by adhering to the standards within this manual whenever training or supervising divers who participate in PADI courses and programs, PADI Members can provide a strong platform from which divers and novices can learn to manage those risks and have fun in the process. How to Use This Manual This manual provides PADI course requirements. Text appearing in boldface print denotes required standards that may not be deviated from while teaching the course. PADI Standards do not, however, supersede local laws or regulations. Keep informed of these wherever you teach. Though all PADI Members use this manual, it is written from the instructor’s perspective, except for course performance requirements. These are written from the student diver’s or program participant’s perspective, stating specifcally what must be demonstrated or performed. As a starting point, become familiar with the items in the Commitment to Excellence section. This includes the PADI Professional’s Creed, PADI Member Code of Practice and Youth Leader’s Commitment. This section outlines your professional commitment to diver safety, responsibility and risk management. -

SDI Diver Standards
part2 SDI Diversdi Standards diver standards SDI Standards and Procedures Part 2: SDI Diver Standards 2 Version 0221 SDI Standards and Procedures Part 2: SDI Diver Standards Contents 1. Course Overview Matrix ..............................11 2. General Course Standards .......................... 13 2.1 Administrative ........................................................................13 2.2 Accidents .................................................................................14 2.3 Definitions ..............................................................................14 2.4 Confined Water Training ......................................................15 2.5 Open Water Training ............................................................15 2.6 Student – Minimum Equipment Requirements ..............16 2.7 Instructor – Minimum Equipment Requirements ..........16 2.8 Temporary Certification Cards ...........................................17 2.9 Upgrading from SDI Junior certification to full SDI certification ...................................................................................17 3. Snorkeling Course ....................................... 18 3.1 Introduction ............................................................................18 3.2 Qualifications of Graduates.................................................18 3.3 Who May Teach ......................................................................18 3.4 Student to Instructor Ratio ..................................................18 3.5 Student -

Training Objectives for a Diving Medical Physician
The Diving Medical Advisory Committee Training Objectives for a Diving Medicine Physician This guidance includes all the training objectives agreed by the Diving Medical Advisory Committee, the European Diving Technology Committee and the European Committee for Hyperbaric Medicine in 2011. Rev 1 - 2013 INTRODUCTION The purpose of this document is to define more closely the training objectives in diving physiology and medicine that need to be met by doctors already fully accredited or board-certified in a clinical speciality to national standards. It is based on topic headings that were originally prepared for a working group of European Diving Technology Committee (EDTC) and the European Committee of Hyperbaric Medicine (ECHM) as a guide for diving medicine some 20 years ago by J.Desola (Spain), T.Nome (Norway) & D.H.Elliott (U.K.). The training now required for medical examiners of working divers and for specialist diving medicine physicians was based on a EDTC/ECHM standard 1999 and subsequently has been enhanced by the Diving Medical Advisory Committee (DMAC), revised and agreed in principle by DMAC, EDTC and ECHM in 2010 and then ratified by EDTC and ECHM in 2011. The requirements now relate to an assessment of competence, the need for some training in occupational medicine, the need for maintenance of those skills by individual ‘refresher training’. Formal recognition of all this includes the need to involve a national authority for medical education. These objectives have been applied internationally to doctors who provide medical support to working divers. (Most recreational instructors and dive guides are, by their employment, working divers and so the guidance includes the relevant aspects of recreational diving. -
Dive Courses Price List
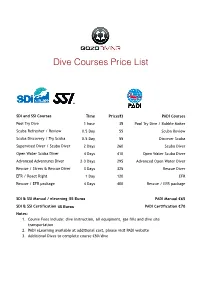
Dive Courses Price List ! ! SDI and SSI Courses Time Price(€) PADI Courses Pool Try Dive 1 hour 35 Pool Try Dive / Bubble Maker Scuba Refresher / Review 0.5 Day 55 Scuba Review Scuba Discovery / Try Scuba 0.5 Day 55 Discover Scuba Supervised Diver / Scuba Diver 2 Days 260 Scuba Diver Open Water Scuba Diver 4 Days 410 Open Water Scuba Diver Advanced Adventures Diver 2-3 Days 295 Advanced Open Water Diver Rescue / Stress & Rescue Diver 3 Days 325 Rescue Diver EFR / React Right 1 Day 120 EFR Rescue / EFR package 4 Days 400 Rescue / EFR package SDI & SSI Manual / elearning €5545 Euros PADI Manual €65 SDI & SSI Certification €4535 Euros PADI Certification €70 Notes: 1. Course Fees include: dive instruction, all equipment, gas fills and dive site transportation 2. PADI eLearning available at additional cost, please visit PADI website 3. Additional Dives to complete course €50/dive ! ! SDI and SSI Specialty Courses Time Price(€) PADI Specialty Courses Sidemount 4 Days 500 Sidemount Computer Nitrox (incl.2 dives) 1 Day 150 Nitrox (incl.2 dives) Deep 2 Days 200 Deep Wreck 3 Days 200 Wreck SDI & SSI Manual / elearning €45 PADI Manual €45 SDI & SSI Certification €35 PADI Certification €70 Notes: 1. Course Fees include: dive instruction, cylinders, weights, gas fills and dive site transportation 2. Equipment rental is at additional cost 3. PADI eLearning available at additional cost, please visit PADI website 4. Other specialties are available on request 5. Additional Dives to complete course - €50/dive ! ! Professional Courses Time Price (€) Professional Courses Divemaster 2 weeks 900 Divemaster Open Water Instructor 8 Days 1,500 n/a Notes: 1.