Current Understanding of and Emerging Treatment Options for Spinal Muscular Atrophy with Respiratory Distress Type 1 (SMARD1)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Severe Infantile Neuropathy with Diaphragmatic Weakness and Its Relationship to SMARD1
DOI: 10.1093/brain/awg278 Advanced Access publication September 23, 2003 Brain (2003), 126, 2682±2692 Severe infantile neuropathy with diaphragmatic weakness and its relationship to SMARD1 Matthew Pitt,1 Henry Houlden,2 Jean Jacobs,2 Quen Mok,1 Brian Harding,1 Mary Reilly2 and Robert Surtees1 1Great Ormond Street Hospital for Children and Correspondence to: Dr Matthew Pitt, Department of 2The National Hospital for Neurology and Neurosurgery, Clinical Neurophysiology, Great Ormond Street Hospital London, UK for Children NHS Trust, Great Ormond Street, London WC1N 3JH, UK E-mail [email protected] Downloaded from Summary A group of 13 patients with early onset diaphragmatic cord in one patient failed to ®nd any evidence of an palsy in association with a progressive neuropathy is SMA. Four out of the ®ve not tested genetically were presented. All eight of those tested were found to have positive for all diagnostic criteria. None of the cases of mutations in the same gene encoding the immunoglobu- early onset neuropathies or spinal muscular atrophies http://brain.oxfordjournals.org/ lin mu-binding protein 2 (IGHMBP2) in patients with with early respiratory failure reviewed in the literature spinal muscular atrophy (SMA) with respiratory dis- shares the exact characteristics, but many do have very tress type 1. Six out of these eight patients had either close similarities. Their classi®cation varies, but the dis- homozygous or compound heterozygous mutations, and covery of mutations in IGHMBP2 in cases that are vari- two had only a single heterozygous mutation. Detailed ously classi®ed as SMA plus or severe infantile analysis of the clinical picture and the neurophysiologi- neuropathy with respiratory distress points to a need cal and histopathological ®ndings indicated that these for the search for this genetic defect to be widened to patients shared similar characteristics, which were fur- include both groups. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Nizzardo 1..10
RESEARCH ARTICLE GENE THERAPY 2015 © The Authors, some rights reserved; exclusive licensee American Association for the Advancement of Science. Distributed Gene therapy rescues disease phenotype in a under a Creative Commons Attribution NonCommercial License 4.0 (CC BY-NC). spinal muscular atrophy with respiratory 10.1126/sciadv.1500078 distress type 1 (SMARD1) mouse model Monica Nizzardo,1* Chiara Simone,1 Federica Rizzo,1 Sabrina Salani,1 Sara Dametti,1 Paola Rinchetti,1 Roberto Del Bo,1 Kevin Foust,2 Brian K. Kaspar,2,3,4 Nereo Bresolin,1 Giacomo P. Comi,1 Stefania Corti1 Spinal muscular atrophy with respiratory distress type 1 (SMARD1) is an autosomal recessive motor neuron disease affecting children. It is caused by mutations in the IGHMBP2 gene (11q13) and presently has no cure. Recently, adeno-associated virus serotype 9 (AAV9)–mediated gene therapy has been shown to rescue the phenotype of Downloaded from animal models of another lower motor neuron disorder, spinal muscular atrophy 5q, and a clinical trial with this strategy is ongoing. We report rescue of the disease phenotype in a SMARD1 mouse model after therapeutic de- livery via systemic injection of an AAV9 construct encoding the wild-type IGHMBP2 toreplacethedefectivegene. AAV9-IGHMBP2 administration restored protein levels and rescued motor function, neuromuscular physiology, and life span (450% increase), ameliorating pathological features in the central nervous system, muscles, and heart. To test this strategy in a human model, we transferred wild-type IGHMBP2 into human SMARD1-induced pluripotent stem cell–derived motor neurons; these cells exhibited increased survival and axonal length in long-term culture. -

Refined Genetic Mapping of Autosomal Recessive Chronic Distal Spinal Muscular Atrophy to Chromosome 11Q13.3 and Evidence of Link
European Journal of Human Genetics (2004) 12, 483–488 & 2004 Nature Publishing Group All rights reserved 1018-4813/04 $30.00 www.nature.com/ejhg ARTICLE Refined genetic mapping of autosomal recessive chronic distal spinal muscular atrophy to chromosome 11q13.3 and evidence of linkage disequilibrium in European families Louis Viollet*,1, Mohammed Zarhrate1, Isabelle Maystadt1, Brigitte Estournet-Mathiaut2, Annie Barois2, Isabelle Desguerre3, Miche`le Mayer4, Brigitte Chabrol5, Bruno LeHeup6, Veronica Cusin7, Thierry Billette de Villemeur8, Dominique Bonneau9, Pascale Saugier-Veber10, Anne Touzery-de Villepin11, Anne Delaubier12, Jocelyne Kaplan1, Marc Jeanpierre13, Joshue´ Feingold1 and Arnold Munnich1 1Unite´ de Recherches sur les Handicaps Ge´ne´tiques de l’Enfant, INSERM U393. Hoˆpital Necker Enfants Malades, 149 rue de Se`vres, 75743 Paris Cedex 15, France; 2Service de Neurope´diatrie, Re´animation et Re´e´ducation Neuro-respiratoire, Hoˆpital Raymond Poincare´, 92380 Garches, France; 3Service de Neurope´diatrie, Hoˆpital Necker Enfants Malades, 149 rue de Se`vres, 75743 Paris Cedex 15, France; 4Service de Neurope´diatrie, Hoˆpital Saint Vincent de Paul, 82 boulevard Denfert Rochereau, 75674 Paris Cedex 14, France; 5Service de Neurope´diatrie, Hoˆpital Timone Enfants, 264 rue Saint Pierre 13385 Marseille Cedex, France; 6Secteur de De´veloppement et Ge´ne´tique, CHR de Nancy, Hoˆpitaux de Brabois, Rue du Morvan, 54511 Vandoeuvre Cedex, France; 7Service de Ge´ne´tique de Dijon, Hoˆpital d’Enfants, 2 blvd du Mare´chal de Lattre de Tassigny, -

Supplementary Tables S1-S3
Supplementary Table S1: Real time RT-PCR primers COX-2 Forward 5’- CCACTTCAAGGGAGTCTGGA -3’ Reverse 5’- AAGGGCCCTGGTGTAGTAGG -3’ Wnt5a Forward 5’- TGAATAACCCTGTTCAGATGTCA -3’ Reverse 5’- TGTACTGCATGTGGTCCTGA -3’ Spp1 Forward 5'- GACCCATCTCAGAAGCAGAA -3' Reverse 5'- TTCGTCAGATTCATCCGAGT -3' CUGBP2 Forward 5’- ATGCAACAGCTCAACACTGC -3’ Reverse 5’- CAGCGTTGCCAGATTCTGTA -3’ Supplementary Table S2: Genes synergistically regulated by oncogenic Ras and TGF-β AU-rich probe_id Gene Name Gene Symbol element Fold change RasV12 + TGF-β RasV12 TGF-β 1368519_at serine (or cysteine) peptidase inhibitor, clade E, member 1 Serpine1 ARE 42.22 5.53 75.28 1373000_at sushi-repeat-containing protein, X-linked 2 (predicted) Srpx2 19.24 25.59 73.63 1383486_at Transcribed locus --- ARE 5.93 27.94 52.85 1367581_a_at secreted phosphoprotein 1 Spp1 2.46 19.28 49.76 1368359_a_at VGF nerve growth factor inducible Vgf 3.11 4.61 48.10 1392618_at Transcribed locus --- ARE 3.48 24.30 45.76 1398302_at prolactin-like protein F Prlpf ARE 1.39 3.29 45.23 1392264_s_at serine (or cysteine) peptidase inhibitor, clade E, member 1 Serpine1 ARE 24.92 3.67 40.09 1391022_at laminin, beta 3 Lamb3 2.13 3.31 38.15 1384605_at Transcribed locus --- 2.94 14.57 37.91 1367973_at chemokine (C-C motif) ligand 2 Ccl2 ARE 5.47 17.28 37.90 1369249_at progressive ankylosis homolog (mouse) Ank ARE 3.12 8.33 33.58 1398479_at ryanodine receptor 3 Ryr3 ARE 1.42 9.28 29.65 1371194_at tumor necrosis factor alpha induced protein 6 Tnfaip6 ARE 2.95 7.90 29.24 1386344_at Progressive ankylosis homolog (mouse) -

Genetics of Distal Hereditary Motor Neuropathies
GENETICSOFDISTALHEREDITARY MOTOR NEUROPATHIES By alexander peter drew A thesis submitted for the Degree of Doctor of Philosophy Supervised by Professor Garth A. Nicholson Dr. Ian P. Blair Faculty of Medicine University of Sydney 2012 statement No part of the work described in this thesis has been submitted in fulfilment of the requirements for any other academic degree or qualification. Except where due acknowledgement has been made, all experimental work was performed by the author. Alexander Peter Drew CONTENTS acknowledgements ............................. i summary .................................... ii list of figures ................................ v list of tables ................................ viii acronyms and abbreviations ..................... xi publications ................................. xiv 1 literature review ........................... 1 1.1 Molecular genetics and mechanisms of disease in Distal Hereditary Motor Neuropathies . .1 1.1.1 Small heat shock protein family . .2 1.1.2 Dynactin 1 (DCTN1).....................9 1.1.3 Immunoglobulin mu binding protein 2 gene (IGHMBP2) 11 1.1.4 Senataxin (SETX)....................... 14 1.1.5 Glycyl-tRNA synthase (GARS)............... 16 1.1.6 Berardinelli-Seip congenital lipodystrophy 2 (SEIPIN) gene (BSCL2)......................... 18 1.1.7 ATPase, Cu2+-transporting, alpha polypeptide gene (ATP7A) 20 1.1.8 Pleckstrin homology domain-containing protein, G5 gene (PLEKHG5)........................... 21 1.1.9 Transient receptor potential cation channel, V4 gene (TRPV4) 22 1.1.10 DYNC1H1 ........................... 23 1.1.11 Clinical variability in dHMN . 24 1.1.12 Common disease mechanisms in dHMN . 29 2 general materials and methods ................. 32 2.1 General materials and reagents . 32 2.1.1 Reagents and Enzymes . 32 2.1.2 Equipment . 33 2.1.3 Plasticware . 33 2.2 Study participants . 34 2.3 DNA methods . -
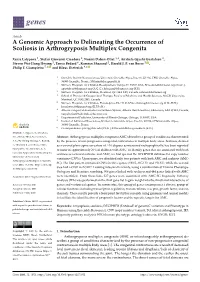
A Genomic Approach to Delineating the Occurrence of Scoliosis in Arthrogryposis Multiplex Congenita
G C A T T A C G G C A T genes Article A Genomic Approach to Delineating the Occurrence of Scoliosis in Arthrogryposis Multiplex Congenita Xenia Latypova 1, Stefan Giovanni Creadore 2, Noémi Dahan-Oliel 3,4, Anxhela Gjyshi Gustafson 2, Steven Wei-Hung Hwang 5, Tanya Bedard 6, Kamran Shazand 2, Harold J. P. van Bosse 5 , Philip F. Giampietro 7,* and Klaus Dieterich 8,* 1 Grenoble Institut Neurosciences, Université Grenoble Alpes, Inserm, U1216, CHU Grenoble Alpes, 38000 Grenoble, France; [email protected] 2 Shriners Hospitals for Children Headquarters, Tampa, FL 33607, USA; [email protected] (S.G.C.); [email protected] (A.G.G.); [email protected] (K.S.) 3 Shriners Hospitals for Children, Montreal, QC H4A 0A9, Canada; [email protected] 4 School of Physical & Occupational Therapy, Faculty of Medicine and Health Sciences, McGill University, Montreal, QC H3G 2M1, Canada 5 Shriners Hospitals for Children, Philadelphia, PA 19140, USA; [email protected] (S.W.-H.H.); [email protected] (H.J.P.v.B.) 6 Alberta Congenital Anomalies Surveillance System, Alberta Health Services, Edmonton, AB T5J 3E4, Canada; [email protected] 7 Department of Pediatrics, University of Illinois-Chicago, Chicago, IL 60607, USA 8 Institut of Advanced Biosciences, Université Grenoble Alpes, Inserm, U1209, CHU Grenoble Alpes, 38000 Grenoble, France * Correspondence: [email protected] (P.F.G.); [email protected] (K.D.) Citation: Latypova, X.; Creadore, S.G.; Dahan-Oliel, N.; Gustafson, Abstract: Arthrogryposis multiplex congenita (AMC) describes a group of conditions characterized A.G.; Wei-Hung Hwang, S.; Bedard, by the presence of non-progressive congenital contractures in multiple body areas. -

A Yeast-Based Model for Hereditary Motor and Sensory Neuropathies: a Simple System for Complex, Heterogeneous Diseases
International Journal of Molecular Sciences Review A Yeast-Based Model for Hereditary Motor and Sensory Neuropathies: A Simple System for Complex, Heterogeneous Diseases Weronika Rzepnikowska 1, Joanna Kaminska 2 , Dagmara Kabzi ´nska 1 , Katarzyna Bini˛eda 1 and Andrzej Kocha ´nski 1,* 1 Neuromuscular Unit, Mossakowski Medical Research Centre Polish Academy of Sciences, 02-106 Warsaw, Poland; [email protected] (W.R.); [email protected] (D.K.); [email protected] (K.B.) 2 Institute of Biochemistry and Biophysics Polish Academy of Sciences, 02-106 Warsaw, Poland; [email protected] * Correspondence: [email protected] Received: 19 May 2020; Accepted: 15 June 2020; Published: 16 June 2020 Abstract: Charcot–Marie–Tooth (CMT) disease encompasses a group of rare disorders that are characterized by similar clinical manifestations and a high genetic heterogeneity. Such excessive diversity presents many problems. Firstly, it makes a proper genetic diagnosis much more difficult and, even when using the most advanced tools, does not guarantee that the cause of the disease will be revealed. Secondly, the molecular mechanisms underlying the observed symptoms are extremely diverse and are probably different for most of the disease subtypes. Finally, there is no possibility of finding one efficient cure for all, or even the majority of CMT diseases. Every subtype of CMT needs an individual approach backed up by its own research field. Thus, it is little surprise that our knowledge of CMT disease as a whole is selective and therapeutic approaches are limited. There is an urgent need to develop new CMT models to fill the gaps. -
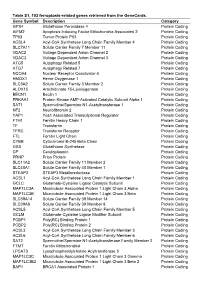
Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein -
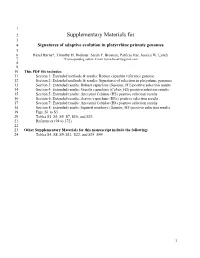
Signatures of Adaptive Evolution in Platyrrhine Primate Genomes 5 6 Hazel Byrne*, Timothy H
1 2 Supplementary Materials for 3 4 Signatures of adaptive evolution in platyrrhine primate genomes 5 6 Hazel Byrne*, Timothy H. Webster, Sarah F. Brosnan, Patrícia Izar, Jessica W. Lynch 7 *Corresponding author. Email [email protected] 8 9 10 This PDF file includes: 11 Section 1: Extended methods & results: Robust capuchin reference genome 12 Section 2: Extended methods & results: Signatures of selection in platyrrhine genomes 13 Section 3: Extended results: Robust capuchins (Sapajus; H1) positive selection results 14 Section 4: Extended results: Gracile capuchins (Cebus; H2) positive selection results 15 Section 5: Extended results: Ancestral Cebinae (H3) positive selection results 16 Section 6: Extended results: Across-capuchins (H3a) positive selection results 17 Section 7: Extended results: Ancestral Cebidae (H4) positive selection results 18 Section 8: Extended results: Squirrel monkeys (Saimiri; H5) positive selection results 19 Figs. S1 to S3 20 Tables S1–S3, S5–S7, S10, and S23 21 References (94 to 172) 22 23 Other Supplementary Materials for this manuscript include the following: 24 Tables S4, S8, S9, S11–S22, and S24–S44 1 25 1) Extended methods & results: Robust capuchin reference genome 26 1.1 Genome assembly: versions and accessions 27 The version of the genome assembly used in this study, Sape_Mango_1.0, was uploaded to a 28 Zenodo repository (see data availability). An assembly (Sape_Mango_1.1) with minor 29 modifications including the removal of two short scaffolds and the addition of the mitochondrial 30 genome assembly was uploaded to NCBI under the accession JAGHVQ. The BioProject and 31 BioSample NCBI accessions for this project and sample (Mango) are PRJNA717806 and 32 SAMN18511585. -

Whole Genome Sequencing Reveals Novel IGHMBP2 Variant Leading to Unique Cryptic Splice‐Site and Charcot‐Marie‐Tooth Phenotype with Early Onset Symptoms
Received: 7 October 2018 | Revised: 24 February 2019 | Accepted: 6 March 2019 DOI: 10.1002/mgg3.676 CLINICAL REPORT Whole genome sequencing reveals novel IGHMBP2 variant leading to unique cryptic splice‐site and Charcot‐Marie‐Tooth phenotype with early onset symptoms Thomas A. Cassini1,2 | Laura Duncan1 | Lynette C. Rives1 | John H. Newman2 | John A. Phillips1 | Mary E. Koziura1 | Jennifer Brault1 | Rizwan Hamid1 | Joy Cogan1 | Undiagnosed Diseases Network 1Department of Pediatrics, Vanderbilt University Medical Center, Nashville, Abstract Tennessee Background: Rare variants (RV) in immunoglobulin mu‐binding protein 2 2Department of Medicine, Vanderbilt (IGHMBP2) [OMIM 600502] can cause an autosomal recessive type of Charcot‐ University Medical Center, Nashville, Marie‐Tooth (CMT) disease [OMIM 616155], an inherited peripheral neuropathy. Tennessee Over 40 different genes are associated with CMT, with different possible inheritance Correspondence patterns. Thomas A. Cassini, Department of An 11‐year‐old female with motor delays was found to have Medicine, Vanderbilt University Medical Methods and Results: Center, Nashville, TN. distal atrophy, weakness, and areflexia without bulbar or sensory findings. Her clini- Email: [email protected] cal evaluation was unrevealing. Whole exome sequencing (WES) revealed a mater- Funding Information nally inherited IGHMBP2 RV (c.1730T>C) predicted to be pathogenic, but no National Human Genome Research variant on the other allele was identified. Deletion and duplication analysis was nega- Institute, Number: UO1HG007674 tive. She was referred to the Undiagnosed Disease Network (UDN) for further evaluation. Whole genome sequencing (WGS) confirmed the previously identified IGHMBP2 RV and identified a paternally inherited non‐coding IGHMBP2 RV. This was pre- dicted to activate a cryptic splice site perturbing IGHMBP2 splicing. -

Us 2018 / 0305689 A1
US 20180305689A1 ( 19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2018 /0305689 A1 Sætrom et al. ( 43 ) Pub . Date: Oct. 25 , 2018 ( 54 ) SARNA COMPOSITIONS AND METHODS OF plication No . 62 /150 , 895 , filed on Apr. 22 , 2015 , USE provisional application No . 62/ 150 ,904 , filed on Apr. 22 , 2015 , provisional application No. 62 / 150 , 908 , (71 ) Applicant: MINA THERAPEUTICS LIMITED , filed on Apr. 22 , 2015 , provisional application No. LONDON (GB ) 62 / 150 , 900 , filed on Apr. 22 , 2015 . (72 ) Inventors : Pål Sætrom , Trondheim (NO ) ; Endre Publication Classification Bakken Stovner , Trondheim (NO ) (51 ) Int . CI. C12N 15 / 113 (2006 .01 ) (21 ) Appl. No. : 15 /568 , 046 (52 ) U . S . CI. (22 ) PCT Filed : Apr. 21 , 2016 CPC .. .. .. C12N 15 / 113 ( 2013 .01 ) ; C12N 2310 / 34 ( 2013. 01 ) ; C12N 2310 /14 (2013 . 01 ) ; C12N ( 86 ) PCT No .: PCT/ GB2016 /051116 2310 / 11 (2013 .01 ) $ 371 ( c ) ( 1 ) , ( 2 ) Date : Oct . 20 , 2017 (57 ) ABSTRACT The invention relates to oligonucleotides , e . g . , saRNAS Related U . S . Application Data useful in upregulating the expression of a target gene and (60 ) Provisional application No . 62 / 150 ,892 , filed on Apr. therapeutic compositions comprising such oligonucleotides . 22 , 2015 , provisional application No . 62 / 150 ,893 , Methods of using the oligonucleotides and the therapeutic filed on Apr. 22 , 2015 , provisional application No . compositions are also provided . 62 / 150 ,897 , filed on Apr. 22 , 2015 , provisional ap Specification includes a Sequence Listing . SARNA sense strand (Fessenger 3 ' SARNA antisense strand (Guide ) Mathew, Si Target antisense RNA transcript, e . g . NAT Target Coding strand Gene Transcription start site ( T55 ) TY{ { ? ? Targeted Target transcript , e .