Project Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Moses Hayim Luzzatto's Quest for Providence
City University of New York (CUNY) CUNY Academic Works All Dissertations, Theses, and Capstone Projects Dissertations, Theses, and Capstone Projects 10-2014 'Like Iron to a Magnet': Moses Hayim Luzzatto's Quest for Providence David Sclar Graduate Center, City University of New York How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/gc_etds/380 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] “Like Iron to a Magnet”: Moses Hayim Luzzatto’s Quest for Providence By David Sclar A Dissertation Submitted to the Graduate Faculty in History in Partial Fulfillment of the Requirement for the Degree of Doctor of Philosophy The City University of New York 2014 © 2014 David Sclar All Rights Reserved This Manuscript has been read and accepted by the Graduate Faculty in History in satisfaction of the Dissertation requirement for the degree of Doctor of Philosophy Prof. Jane S. Gerber _______________ ____________________________________ Date Chair of the Examining Committee Prof. Helena Rosenblatt _______________ ____________________________________ Date Executive Officer Prof. Francesca Bregoli _______________________________________ Prof. Elisheva Carlebach ________________________________________ Prof. Robert Seltzer ________________________________________ Prof. David Sorkin ________________________________________ Supervisory Committee iii Abstract “Like Iron to a Magnet”: Moses Hayim Luzzatto’s Quest for Providence by David Sclar Advisor: Prof. Jane S. Gerber This dissertation is a biographical study of Moses Hayim Luzzatto (1707–1746 or 1747). It presents the social and religious context in which Luzzatto was variously celebrated as the leader of a kabbalistic-messianic confraternity in Padua, condemned as a deviant threat by rabbis in Venice and central and eastern Europe, and accepted by the Portuguese Jewish community after relocating to Amsterdam. -

Bris Or Brit Milah (Ritual Circumcision) According to Jewish Law, a Healthy Baby Boy Is Circumcised on the Eighth Day After His Birth
Bris or Brit milah (ritual circumcision) According to Jewish law, a healthy baby boy is circumcised on the eighth day after his birth. The brit milah, the ritual ceremony of removing the foreskin which covers the glans of the penis, is a simple surgical procedure that can take place in the home or synagogue and marks the identification of a baby boy as a Jew. The ceremony is traditionally conducted by a mohel, a highly trained and skilled individual, although a rabbi in conjunction with a physician may perform the brit milah. The brit milah is a joyous occasion for the parents, relatives and friends who celebrate in this momentous event. At the brit milah, it is customary to appoint a kvater (a man) and a kvaterin (a woman), the equivalent of Jewish godparents, whose ritual role is to bring the child into the room for the circumcision. Another honor bestowed on a family member is the sandak, who is most often the baby’s paternal grandfather or great-grandfather. This individual traditionally holds the baby during the circumcision ceremony. The service involves a kiddush (prayer over wine), the circumcision, blessings, a dvar torah (a small teaching of the Torah) and the presentation of the Jewish name selected for the baby. During the brit milah, a chair is set aside for Elijah the prophet. Following the ceremony, a seudat mitzvah (celebratory meal) is available for the guests. Please take note: Formal invitations for a bris are not sent out. Typically, guests are notified by phone or email. The baby’s name is not given before the bris. -

Shalom San Diego 2014 Guide to the Jewish Community Shalom San Diego 2014 Guide to the Jewish Community
OF SAN DIEGO COUNTY Shalom San Diego 2014 Guide to the Jewish Community Shalom San Diego 2014 Guide to the Jewish Community The Jewish Federation of San Diego County is pleased to present “Shalom San Diego, Guide to the Jewish Community.” Now available as an electronic file (Adobe PDF), it gives you the flexibility to print specific pages and the option to email a copy to family and friends. Whether you’re a longtime resident, new to the area, or just considering a move to San Diego County, we hope you’ll use this informative guide to our community. We look forward to you joining in our many activities! Get the latest information about what is happening at Federation and in the community: • Visit our website at jewishinsandiego.org • Subscribe for weekly updates at jewishinsandiego.org/federationnews.aspx • Like us on Facebook at facebook.com/jewishinsandiego Table of Contents Page Agencies & Organizations 8 Camps 13 College Organizations & Programs 14 Congregations/Synagogues 15 Disabilities & Inclusion 18 Hospice Care 19 Interfaith 19 Jewish Publications 19 Judaica Stores 19 Kosher Caterers & Restaurants 19 Men’s Organizations 20 Mikvaot 20 Mohalim 21 Mortuary/Cemeteries 21 Older Adult Programs & Centers 22 Schools 23 Singles 26 Social Services 26 Women’s Organizations 27 Young Adult Programs 27 Young Family Programs 28 Youth Organizations 29 Updated: March 2014 INDEX A Culture of Peace,...............................................................................................8 Chabad without Borders: Chula Vista & Tijuana.....................................16 -
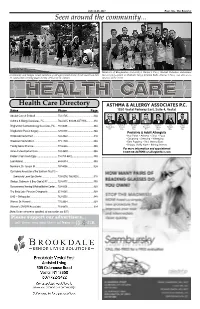
Seen Around the Community
July 14-20, 2017 Page 31A - The Reporter Seen around the community... Members of Binghamton University’s Harpur’s Ferry Student Volunteer Ambulance Community and Temple Israel members of all ages joined in the Torah march on July Service participated in Chabad’s Mega Challah Bake. Harpur’s Ferry was also a co- 22, with some carrying plush Torahs. (Photo by G. Heller) sponsor of the event. Health Care Directory ASTHMA & ALLERGY ASSOCIATES P.C. 1550 Vestal Parkway East, Suite 4, Vestal Name Phone Page Absolut Care at Endicott ...................................754-2705 ........................................32A Asthma & Allergy Associates, PC .....................766-0235, 800-88-ASTHMA ...........31A Elliot Mariah M. Rizwan Joseph Stella M. Julie Shaan Binghamton Gastroenterology Associates, PC ..... 772-0639 .............................................33A Rubinstein, Pieretti, Khan, Flanagan, Castro, McNairn, Waqar, M.D M.D. M.D. M.D. M.D. M.D. M.D. Binghamton Plastic Surgery .............................729-0101 ........................................34A Pediatric & Adult Allergists Brookdale Vestal East ......................................722-3422 ........................................31A • Hay Fever • Asthma • Sinus • Food • Coughing • Sneezing • Wheezing Brookdale Vestal West .....................................771-1700 ........................................33A • Ears Popping • Red, Watery Eyes Family Dental Practice ......................................772-6636 ........................................35A • Drippy, Stuy -

Resource Guide 2013-2014
RESOURCE GUIDE 2013-2014 RESOURCE GUIDE A Guide to Your Jewish Community 2013-2014 INSIDE! Calendar 5774 Announcing On Sale - SEASON Now SUBSCRIBE AND SAVE! SEPTEMBER FEBRUARY Melissa Etheridge Cedar Lake Contemporary Ballet Saturday, September 7, 2013 at 8pm Centennial Hall Thursday, February 6, 2014 at 7:30pm Centennial Hall Orquesta Buena Vista Social Club Bahia Orchestra Project Saturday, September 14, 2013 at 8pm Centennial Hall with Jean-Yves Thibaudet, piano Centennial Hall Friday, February 7, 2014 at 8pm OCTOBER Red Baraat Chris Thile, mandolin Crowder Hall Friday, October 4, 2013 at 8pm Rialto Theatre Saturday, February 8, 2014 at 8pm Arturo Sandoval, trumpet Christine Goerke, soprano Crowder Hall Saturday, October 19, 2013 at 8pm Fox Theatre Thursday, February 13, 2014 at 7:30pm Lang Lang, piano Inon Barnatan, piano Crowder Hall Tuesday, October 22, 2013 at 7:30pm Centennial Hall Thursday, February 20, 2014 at 7:30pm UA Dance: “Premium Blend” Eller Dance Theatre Quartet for the End of Time Thursday, February 27, 2014 at 7:30pm Crowder Hall 7 performances – October 24 – November 2, 2013 MARCH NOVEMBER Tribute to Ella Fitzgerald Jon Batiste and Stay Human Saturday, March 1, 2014 at 8pm Fox Theatre 4 performances – November 7 – 9, 2013 Club Congress Danú DIAVOLO Tuesday, March 4, 2014 at 7:30pm Fox Theatre Saturday, November 9, 2013 at 8pm Centennial Hall Michael Feinstein: The Boston Pops Esplanade Orchestra Centennial Hall “The Gershwins and Me” Centennial Hall Friday, November 15, 2013 at 8pm Sunday, March 9, 2014 at 7pm Unión -

Mez.Iz.Ah Be-Peh―Therapeutic Touch Or Hippocratic Vestige?1
15 Meziẓ aḥ be-Peh―Therapeutic Touch or Hippocratic Vestige? 1 By: SHLOMO SPRECHER With the appearance of a news article in the mass-circulation New York Daily News2 implicating meziẓ aḥ be-peh3 in the death of a Brooklyn 1 The author wishes to emphasize that he subscribes fully to the principle that an individual’s halakhic practice should be determined solely by that individual’s posek. Articles of this nature should never be utilized as a basis for changing one’s minhag. This work is intended primarily to provide some historical background. It may also be used by those individuals whose poskim mandate use of a tube instead of direct oral contact for the performance of meziẓ aḥ , but are still seeking additional material to establish the halakhic bona fides of this ruling. Furthermore, the author affirms that the entire article is predicated only on “Da’at Ba’alei Battim.” 2 February 2, 2005, p. 7. 3 I am aware that purists of Hebrew will insist that the correct vocalization should be be-feh. However, since all spoken references I’ve heard, and all the published material I’ve read, use the form “be-peh,” I too will follow their lead. I believe that a credible explanation for this substitution is a desire to avoid the pejorative sense of the correct vocalization. Lest the reader think that Hebrew vocalization is never influenced by such aesthetic considerations, I can supply proof to the contrary. The Barukh she-’Amar prayer found in Tefillat Shahariṭ contains the phrase “be-feh ‘Amo.” Even a novice Hebraist can recognize that the correct formulation should be in the construct state―“be-fi ‘Amo.” Although many have questioned this apparent error, Rabbi Yitzchak Luria’s supposed endorsement of this nusah ̣ has successfully parried any attempts to bring it into conformity with the established rules of Hebrew grammar. -

1. What Is the Covenant God Made with Abraham? 2. What Does 'Brit Milah'
In order to fulfil the covenant with ‘Then God said to Abraham, “As God that was first made by for you, you must keep my covenant… Abraham, Jewish boys are This is my covenant with you and your circumcised eight descendants after you, the covenant Answer in full sentences or copy out the question! days after their birth. you are to keep: Every male among This is known as 1. What is the covenant God made with Abraham? you shall be circumcised… For the 2. What does ‘Brit Milah’ mean? Brit Milah, which generations to come every male 3. What is ‘circumcision’? means ‘the among you who is eight days old 4. What is a mohel and what do they do? LO: To learn what happens after covenant of 5. Why does the circumcision take place on the birth of a Jewish child must be circumcised.”’ the cutting’. Elijah’s chair? 6. What is given to new-born Jewish babies? 7. What is the meaning of ‘Abraham’? 8. When is a baby girl’s Hebrew name announced? 9. What does the Hebrew name help to do? When a Jewish baby is born, he or 10. How is relationship with God shown through she is often given a Hebrew name as Circumcision is a spall operation to Brit Milah? well as another name. In the Torah, remove the flap of skin at the end of the Hebrew names of many people the penis. This can be done by a have a particular meaning or doctor or by a mohel. A mohel is a Jew who is specially trained in Jewish significance. -

A Taste of Torah
Lech Lecha 5776 October 23, 2015 This week’s edition is dedicated in memory of Avraham Moshe ben Yehuda Leib, Mr. Bud Glassman a”h, whose 8th yahrtzeit was Tuesday, 7 Cheshvan/October 20th A Taste of Torah Stories For The Soul Spare the Wealth A Cut Above By Rabbi Mordechai Fleisher For more than sixty years, Rabbi Avram has just miraculously defeated live” is a refernce to Avram’s fear that the Yosef Chaim Sonnenfeld (1848-1932) served as a mohel. He never refused an four mighty kings. The reason for his going Egyptians would murder him to make his invitation to serve as mohel, and his to war in the first place? No, they weren’t wife available. But what is meant by “go face shone with joy when he had the trying to develop a nuclear weapon, well with me?” Rashi explains that Avram privilege of performing a bris milah on but they had just crushed the armies expected that the Egyptians would offer a Jewish child - “to add another Jew to of five other kings, and, in the process, him gifts to win his “sister’s” hand! How the King’s legions,” he would say. captured Avram’s nephew Lot. Avram felt does this jibe with the Avram who refuses responsible to rescue his nephew, and, with any recompense from the King of Sodom? Once, a huge snowstorm hit Jerusalem, leaving close to three feet of Divine intervention, he won a spectacular One approach to this conundrum may snow on the ground. Walking outside victory. be as follows: Rashi makes it clear that posed a real danger, especially for One of the five kings initially defeated when Avram went down to Egypt, he had someone of Rabbi Sonnenfeld’s age – before Avram appeared on the scene was a shortage of funds, and he incurred debts he was already in his 70’s. -

A Guide to the Birth of Your Child at Emanuel Synagogue}
{A GUIDE TO THE BIRTH OF YOUR CHILD AT EMANUEL SYNAGOGUE} Enriching Jewish life 1 WELCOME who have come before and is one of the first steps linking him to the community The birth of a child is a moment for and his people. At the same time as the celebration, both in your family and our circumcision, there is also a naming community. It is the joy in the fulfillment of ceremony when he is given his Hebrew the promise of the next generation. As with name. many moments in our lives, we use a ritual to add meaning and context to celebrate CIRCUMCISION/BRIT MILAH and to sanctify this great occasion. Through Circumcision is a commandment which this guide, we hope to answer some of the derives from the Torah and the story of questions you may have and offer some Abraham where he makes a covenant with suggestions about ways you may choose to God and is commanded to circumcise celebrate the birth of your child. himself, his household and then the generations of boys to follow on the 8th THE BIRTH OF A BOY day after their birth. We conduct the When a boy is born in Judaism we welcome circumcision with a ceremony and blessings him and bring him into the covenant with which acknowledge and celebrate the the ritual of circumcision. This moment and covenantal relationship. ceremony connects him to the generations 2 WHEN DOES THE CIRCUMCISION TAKE offer recommendations. The mohel knows PLACE? how to do all the appropriate rituals for Brit Milah, and your rabbis are happy to be Circumcision ceremonies occur on or present as well. -

Abraham Diamond, the Mohel of Omaha
EDITION 29 • SUMMER / FALL 2019 IN THIS ISSUE Nebraska Jewish Historical Society Upcoming Events 3 www.nebraskajhs.com Genealogy Corner 11 Meet Jeannette Gabriel 13 From Generation to Generation • The Newsletter of the Nebraska Jewish Historical Society This publication is produced through the generosity of the David and Rose Katzman Endowment Fund of the Jewish Federation of Omaha Foundation. Abraham Diamond, The Mohel of Omaha A Butcher by Trade and Owner of Diamond’s Kosher Meat Market By: Richard Fellman If a poll was taken today among the Jews of Omaha and one of the questions asked was “have you ever attended a “Bris?” nearly every man would blink and maybe smile and say “why yes, I was at my own, and I’ve also been to a number of others,” and every woman would answer with a grimace of sorts and say, “ I sure was, at my son’s, or my grandson’s, or my” ….naming some other male…”and I kept my eyes closed the entire time.” We all know what a ‘Bris’ is, and we’ve all been to one. And for those who do not recognize the word “Bris” or “Brit” as it is pronounced in Israel and most synagogues today it is simply a “circumcision” and the ceremony which surrounds the actual minor bit of surgery customarily done on Jewish infant males when they are eight days old The custom is observed by the vast majority of Jews the world over and consists of removing the foreskin from the penis of the infant male. Historically, the actual surgery was performed by a man called a “Mohel” who was usually trained as an apprentice by another mohel. -

Islamic and Jewish Dietary Laws Compared - Wikipedia, the Free Encyclopedia
Islamic and Jewish dietary laws compared - Wikipedia, the free encyclopedia Islamic and Jewish dietary laws compared From Wikipedia, the free encyclopedia (Redirected from Comparison of Dhabi•a Halal and kashrut) Jump to: navigation, search Part of a series on the It has been suggested that this article or Islamic Jurisprudence section be merged into Ritual slaughter. – a discipline of Islamic studies (Discuss) Fields ● Economical The Islamic dietary laws (Dhabiha Halaal) and the ● Political Jewish dietary laws (Kashrut) are both quite detailed, ● Marital and contain both points of similarity and discord. ● Criminal They share a common root: a code of laws found in ● Etiquette Leviticus and recapitulated in the Quran. ● Theological ● Hygiene ❍ Islamic cleanliness Contents ■ Ihram ■ Wudu [hide] ■ Ghusl ■ Tayammum ● 1 Substance classification ■ Miswak ■ ❍ 1.1 Similarities Najis ■ Sexual Hygiene ❍ 1.2 Differences ❍ Dietary laws ● 2 Slaughter ■ Dhabi•a – Slaughter ❍ 2.1 Similarities ■ Banned Slaughtering ❍ 2.2 Differences of animals ● 3 Miscellaneous comparisons ■ Comparison to kashrut ❍ 3.1 Similarities ❍ Toilet Etiquette ❍ 3.2 Differences ● Military ● 4 See also ● 5 Notes This box: view • talk • edit [edit] Substance classification http://en.wikipedia.org/wiki/Comparison_of_Dhabi•a_Halal_and_kashrut (1 of 7)2/15/2008 2:27:25 PM Islamic and Jewish dietary laws compared - Wikipedia, the free encyclopedia [edit] Similarities ● Blood and swine are prohibited in kashrut and dhabi•a halal. [1][2] ● Many animals permitted in kashrut are also dhabi•a halal, such as bovines. [3][4] ● Kashrut and dhabi•a halal guidelines both generally forbid the consumption of amphibian citation needed animals such as frogs. [5][ ] ● According to kashrut, almost all insects are not kosher. -

Digging the Well Deep (Zevic Mishor Doctoral Thesis)
Errata Notice (for Doctoral Thesis) Digging the Well Deep: The Jewish “Ultra-Orthodox” Relationship with the Divine Explored through the Lifeworld of the Breslov Chasidic Community in Safed Author of Notice: Dr Zevic Mishor Date of Notice submission: 2nd May 2019 Errata: With the aid of Heaven") to top') בס"ד Title page: Add Hebrew acronym right-hand corner, as per standard practice in the Jewish tradition for written material. Page ix (Table of Photographs): Amend Figure 6 entry to: “The Breslov Magen Avot boys school in Safed” Page 86: Amend Figure 6 caption to “The Breslov Magen Avot boys school in Safed” Page 287: Add thesis closing quotation in Hebrew: ״...כי הכל הבל – לבד הנשמה הטהורה, שהיא עתידה לתן דין וחשבון לפני כסא כבודך״ (ברכות השחר) [English translation: “… for all is vain – except for the pure soul that is destined to give justification and reckoning before the throne of Your glory” (Morning blessings)] Digging the Well Deep The Jewish “Ultra-Orthodox” Relationship with the Divine Explored through the Lifeworld of the Breslov Chasidic Community in Safed A thesis submitted for the degree of Doctor of Philosophy (Anthropology) at The University of Sydney by Zevic Mishor October 2016 Supervisor: Professor Jadran Mimica ii Abstract The Jewish Charedi (“ultra-orthodox”) community is an example of a contemporary social group whose lifeworld is dictated almost entirely by the tenets of its religious beliefs. This thesis seeks to illuminate the physical, psychological, social and metaphysical structures of that Charedi world, using the Breslov Chasidic community in the town of Safed, northern Israel, as its ethnographic anchor.