Projects in Swansea University
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Historical Portsmouth Number List
Historical Portsmouth Number List The RYA Portsmouth Yardstick Scheme is provided to enable clubs to allow boats of different classes to race against each other fairly. The RYA actively encourages clubs to adjust handicaps where classes are either under or over performing compared to the number being used. The Portsmouth Yardstick list combines the Portsmouth numbers with class configuration and the total number of races returned to the RYA in the annual return. This additional data has been provided to help clubs achieve the stated aims of the Portsmouth Yardstick system and make adjustments to Portsmouth Numbers where necessary. Clubs using the PN list should be aware that the list is based on the average performance of each boat across a variety of clubs and locations. The numbers in the PN list may not reflect the peak performance of each boat. Historical numbers are listed below and have been collated from the RYA's archive of PN lists. It should be remembered that the Portsmouth Yardstick number list has been through a number of changes and the numbers listed below have had conversion factors applied where needed. It should also be remembered that whilst all efforts are taken for PN's not to drift, relative performance of older boats may be quite different to modern classes. The numbers are given as a starting point to help clubs arrive at a fair number and if these numbers are used then they should be reviewed regularly. Users of the PY scheme are reminded that all Portsmouth Numbers published by the RYA should be regarded as a guide only. -

Portsmouth Number List 2019
Portsmouth Number List 2019 The RYA Portsmouth Yardstick Scheme is provided to enable clubs to allow boats of different classes to race against each other fairly. The RYA actively encourages clubs to adjust handicaps where classes are either under or over performing compared to the number being used. The Portsmouth Yardstick list combines the Portsmouth numbers with class configuration and the total number of races returned to the RYA in the annual return. This additional data has been provided to help clubs achieve the stated aims of the Portsmouth Yardstick system and make adjustments to Portsmouth Numbers where necessary. Clubs using the PN list should be aware that the list is based on the typical performance of each boat across a variety of clubs and locations. Experimental numbers are based on fewer returns and are to be used as a guide for clubs to allocate as a starting number before reviewing and adjusting where necessary. The list of experimental Portsmouth Numbers will be periodically reviewed by the RYA and is based on data received via PY Online. Users of the PY scheme are reminded that all Portsmouth Numbers published by the RYA should be regarded as a guide only. The RYA list is not definitive and clubs should adjust where necessary. For further information please visit the RYA website: http://www.rya.org.uk/racing/Pages/portsmouthyardstick.aspx RYA PN LIST - Dinghy No. of Change Class Name Rig Spinnaker Number Races Notes Crew from '18 420 2 S C 1111 0 428 2000 2 S A 1112 3 2242 29ER 2 S A 907 -5 277 505 2 S C 903 0 277 -

Über Die PERSENNINGEN Für PIRATEN
CF-Hersteller-Übersicht – 1 – Künstler maritimer Motive 1-82 CF-ÜBERSICHT der KÜNSTLER maritimer Motive (Bildhauer, Maler, Modellbauer usw.) 209 Tel: 04351 / 89 20 595 Fax: 04351 / 89 20 596 WebSite: http://www.classic-forum.org Email: [email protected] (Stand: 02.11.2014 / Zusammenstellung: Bernd Klabunde, Eckernförde) (jeweils letzte bekannte Adresse) – >>>> Bei diese Aufstellung maritimer Künstler handelt es sich um einen privaten Service; kein Verkauf und keine Lieferung durch mich ! <<<< >>>> Diese Aufstellung befindet sich z.Z. noch im Aufbau <<<< Zu den Angaben: Die Künstler usw. stellen eine Auswahl dar, wobei Umfang und Inhalt laufend erweitert werden. Es handelt sich in erster Linie um Hersteller künstlerischer Motive. – Es sind auch ältere, ehemalige (die nicht mehr produzieren) oder schon verstorbene Künstler (NICHT AKTUELL, bzw. VERSTORBEN=graue und kursive Schrift und nicht fett), aufgeführt, damit „niemand einer guten Namen oder alten Adresse nachläuft“, die aber nicht mitgezählt worden sind! [Die Jahreszahlen in den eckigen Klammern hinter den Namen beziehen sich immer auf den letzten Stand der Information; ein „H 2OOO/2OO1“ davor sagt aus, dass es sich um einen aktuellen=lebenden Künstler handelt!] – Die Email-/Web-Adressen beziehen sich auch auf Infos über den Künstler. – Etliche der Künstler beschäftigen sich zudem mit anderen Bereichen ihres jeweiligen Kunstgebietes! – Hinweis: Bei verstorbenen Künstlern weisen die Email-/Web-Adressen auf Informationen über diese. Anmerkung: Die aufgeführten Adressen stellen nur eine Auswahl dar, die dabei keinesfalls qualitativen Charakter hat ! Meine Bitte: Diese Aufstellung lebt von den durch die Leser gelieferten aktuellen Angaben, da ich nicht laufend selbst alle Angaben überprüfen kann. Sollten sich also Angaben zwischenzeitlich verändert haben, so bitte ich um eine entsprechende Nachricht. -

Maud Matters
Wherry Maud Trust August 2018 Maud Matters Newsletter No.6 Your trustees are happy with Wherry Maud Trust's progress and glad that this year we have even more members who take an active part in sailing on Maud, maintaining her and showing her off to the wider public. We should all celebrate the fact that this year there are eight wherry- rigged vessels afloat. Each plays an important role in the Broadland wherry scene and your membership and support enables Maud to play her part. INSIDE THIS ISSUE Grants Awarded ...................... 2 MESSAGE FROM OUR PATRON Maud at Heritage Open Days .. 3 RICHARD JEWSON JP—LORD LIEUTENANT OF NORFOLK HAS WRITTEN AS FOLLOWS: Maud’s Winter Maintenance... 3 Maud’s Trips + Other Events .. 4 “It has been interesting for me this year to see how Wherry Maud Trust is Upcoming WMT Events .......... 7 growing and using new ways to bring "our" wherry to the attention of the Associate membership ............ 7 public and of course to generate Meet the Skippers ................... 8 funds for her upkeep. Crew Matters ........................... 8 In May I was pleased to attend the Other Historic Vessels ............ 9 Wherry Maud Trust art exhibition at Volunteering ........................... 12 Ranworth. It showcased the work of Social Media ............................ 13 local artists and was the Trust's first Other Events Upcoming.......... 13 large-scale funding event . The suc- Contact Us ............................... 14 cess of the event was due to the many volunteers who helped over the two days. Volunteers were serving light refreshments, meeting and greeting the public and explaining the purpose of the event and the im- portance of Maud in the Broads scene. -

Portsmouth Number List 2016
Portsmouth Number List 2016 The RYA Portsmouth Yardstick Scheme is provided to enable clubs to allow boats of different classes to race against each other fairly. The RYA actively encourages clubs to adjust handicaps where classes are either under or over performing compared to the number being used. The Portsmouth Yardstick list combines the Portsmouth numbers with class configuration and the total number of races returned to the RYA in the annual return. This additional data has been provided to help clubs achieve the stated aims of the Portsmouth Yardstick system and make adjustments to Portsmouth Numbers where necessary. Clubs using the PN list should be aware that the list is based on the typical performance of each boat across a variety of clubs and locations. Experimental numbers are based on fewer returns and are to be used as a guide for clubs to allocate as a starting number before reviewing and adjusting where necessary. The list of experimental Portsmouth Numbers will be periodically reviewed by the RYA and is based on data received from the PY Online website (www.pys.org.uk). Users of the PY scheme are reminded that all Portsmouth Numbers published by the RYA should be regarded as a guide only. The RYA list is not definitive and clubs should adjust where necessary. For further information please visit the RYA website: http://www.rya.org.uk/racing/Pages/portsmouthyardstick.aspx RYA PN LIST - Dinghy Change Class Name No. of Crew Rig Spinnaker Number Races Notes from '15 420 2 S C 1105 0 278 2000 2 S A 1101 1 1967 29ER 2 S A -
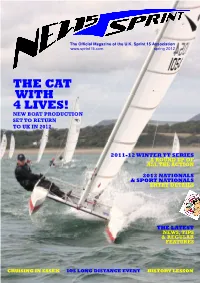
Mag. Spring 2012 V1
The Official Magazine of the U.K. Sprint 15 Association www.sprint15.com spring 2012 THE CAT WITH 4 LIVES! NEW BOAT PRODUCTION SET TO RETURN TO UK IN 2012 2011-12 WINTER TT SERIES A ROUND UP OF ALL THE ACTION 2012 NATIONALS & SPORT NATIONALS ENTRY DETAILS THE LATEST NEWS, TIPS & REGULAR FEATURES CRUISING IN ESSEX IOS LONG DISTANCE EVENT HISTORY LESSON COMMENTS IN THIS ISSUE from the ED YOUR CHAIRMAN WRITES...... 3 As another new summer season beckons, I feel there is a great deal to be optimistic about for 2012 and beyond. NATIONAL CHAMPIONSHIPS The BIG NEWS which you’ll read about in this issue is on the arrangements that are already well in hand to bring 2012 Windsport Sport Nationals:NOR & Entry Details 27-28 production of new boats back to the UK. And if our new boat is anything like the new Dart 18’s rolling off Rob White’s 2012 Windsport Nationals at Brightlingsea:NOR & Entry 29-31 production line, we’re in for a real treat. I looked at one of Details the new 18’s on the stand at the Ally Pally Dinghy Show and WINDSPORT SUMMER 2011 TT SERIES it was nothing short of superb. The substantial investment and commitment by Ian Fraser and Windsport to make all 2011 Northern Championship (Carsington TT) 8 this possible should be seen as a huge vote of confidence for our class future. We, the members, need to seal that 2011 Inland Championship (Grafham TT) 10 future and I believe it is within our powers to do so. -

FOI Response 090-15 16. Data.Xlsx
Project Title Project Lead Lay Summary Date Issued to IGRP Outcome Date of IGRP approval Health Care Utilisation, Care Pathways and Ann John, Associate Professor Public 19/10/2015 Approved 23/12/2015 Educational Status in Children and Young People with Mental Health, Swansea University Mental health issues are of growing concern and a source of controversy in children and young people (CYP) in the United Kingdom (U.K). They have been found to contribute to adverse life outcomes (such as poor Adolescent Mental Health (AMH) problems with a educational achievement) and serious disruptions to CYP's lives and those of their families . It is estimated from Office of National Statistics population survey data that, at any one time, four in 100 of CYP, have a focus on Self harm, Eating Disorders and Anxiety and clinically diagnosable or relevant emotional disorder (anxiety or depression). Some disorders such as anxiety may start when children are as young as 11 years. Earlier age of onset appears to be associated with Depression) greater severity and poorer long term outcomes . Concerns are heightened by the persistence of childhood or adolescent mental health issues into adulthood where up to a fifth of the adult population may be affected by a common mental disorder at any one time. Many of these conditions are managed in primary care and there are issues about the transition of care between primary and hospital care and appropriate settings to deliver care to children. There are also issues relating to those that do make contact but are lost to services from childhood to adulthood and between primary care and hospital care. -

September RSA Newsletter
Roach Sailing Association www.paglesham.org.uk/rsa September 2008 Newsletter In this issue Chairman’s Report Racing Update Laying Up Supper Paglesham Gentlemen’s cruise 2008 Bosun’s Corner PHILOMELLE in France 2008 West System Dances with Whales Racing Update The Laying Up Supper will be at the Brandy Hole Chairman’s Report Yacht Club this year on Sat 22nd November Rodney Choppin The club is at Hullbridge. Turn down Ferry Road as if Still to come…… you were crossing the river There is a Budgens store on the corner by the mini roundabout. Take the last turning to the right down Pooles Lane and the club is at the end of this road, next to Brandy Hole Yacht station (which is a separate enterprise). We suggest meeting at 7-.7.30pm The rate for the meal of £15 per person and details of the menu are as follows: -o0o- Melon – A1 Prawn Cocktail – A2 Vegetable Soup - A3 -o0o- Vegetarian Lasagne - B1 Roast Lamb - B2 All the John’s! Fitting out 2008 Poached Haddock - B3 -o0o- I would like to take this opportunity to introduce new Apple and Raisin Crumble - C1 members this year: Peach Melba – C2 Cheese and biscuits – C3 -o0o- Laying Up Supper Tea or Coffee RSA September 2008 Newsletter 1 -o0o- Donations can also be paid direct to PVT and sent to the Treasurer, David Whittingham, Cobblers Row, Richard has kindly again agreed to take the Paglesham (but please note that direct payments to reservations for this and cheques should be sent to him PVT cannot attract gift aid). -

Solar Sails for Planetary Defense & High-Energy Missions
Solar Sails for Planetary Defense & High-Energy Missions Jan Thimo Grundmann, Waldemar Bauer, Kai Borchers, Etienne Dumont, Christian D. Grimm, Tra-Mi Ho, Rico Jahnke, Aaron D. Koch, Caroline Lange, Volker Maiwald, Jan-Gerd Meß, Eugen Mikulz, Dominik Quantius, Siebo Reershemius, Thomas Renger, Kaname Sasaki, Patric Seefeldt, Peter Spietz, Tom Spröwitz, Maciej Sznajder, Norbert Tóth DLR German Aerospace Center, Institute of Space Systems, Robert-Hooke-Strasse 7, 28359 Bremen, Germany [email protected], +49-421-24420-1107 [email protected], [email protected], [email protected], [email protected], [email protected], [email protected], [email protected], [email protected], [email protected], Jan- [email protected], [email protected], [email protected], [email protected], [email protected], [email protected], [email protected], [email protected], [email protected], [email protected], [email protected] Matteo Ceriotti, Colin McInnes, Jens Biele Alessandro Peloni, Christian Krause University of Glasgow DLR German Aerospace Center Glasgow, Scotland G12 8QQ Space Operations and Astronaut United Kingdom Training – MUSC [email protected], 51147 Cologne, Germany [email protected], [email protected] [email protected] [email protected] Bernd Dachwald David Herčík Faculty of Aerospace Engineering Institute for Geophysics and FH Aachen Univ. of Applied Sciences Extraterrestrial Physics Hohenstaufenallee 6 Technical University Braunschweig 52064 Aachen, Germany Braunschweig, Germany [email protected] [email protected] Roy Lichtenheldt, Friederike Wolff Alexander Koncz, Ivanka Pelivan, DLR German Aerospace Center Nicole Schmitz Robotics and Mechatronics Center DLR German Aerospace Center Institute of System Dynamics and Institute of Planetary Research Control Rutherfordstr. -

Broadreach July 2016
Broadreach July 2016 Broadwater Sailing Club Affiliated to the RYA A large fleet of Miracles in some close racing at the Broadwater Open Meeting held in April Club sailors, John, Barry and Stewart ...neck and neck... Editorial Another summer is well underway and it’s great to see the lake as busy as ever. Spring saw several open meetings which allows the club to welcome guests from all parts of the country and try not to let them leave with all the prizes. So, we have reports from the regular Solo and Miracle events and also from the club’s very first Aero meeting. All these events were blessed with good weather, decent numbers and excellent organisation, which all helps to ensure that sail- ors have a nice time at the club and return the following year. Besides the racing events we have several pieces about our little piece of Middlesex. One article on the factors that affect the depth of our lake (courtesy of Dave Weatherhead), another on mapping the buoys and the creation of a smart new course board by our resident engineer and craftsman, Peter Joseph. Finally, we have a picture and a short piece about HS2 which I’m pleased to say shouldn’t impact us too much when they finally start work on it (assuming it gets approval later this year). Our regular member profile slot is about someone well known to many, especially if you’ve been a member for some time. Wolfgang Ansorge has a fun story to tell, particularly about how his passion for sailing has definitely been passed down to his children (after a shaky start) - something most parents would certainly like to emulate. -
Back Issues 6/10/05 11:45 Am Page 66
MMPG back issues 6/10/05 11:45 am Page 66 DECEMBER 1988 Italian battleship camouflage • PR ‘89 • Radar Decoy Launchers • USS Eastbourne • Andromeda 11 trawler Forrestal visited • U•boat modelled • detail Workshop • forming cones • Woodlark Steam Launch • Ships in bot- D530B gun described tles • Building a towing hulk • RN DECEMBER 1989 Camouflage 43 46 • OPV to 1/72 Vietnam river monitor detaled • scale • US Midwest regionals Workshop – preparing fittings JANUARY 1989 Merch•yr•Afon Launch reviewed • Up Dean’s Marine Helen reviewed • Scope hydraulic control linkages • XSV German Cruiser camouflage • 40mm Loyal Mediator photo feature • Steam USN gun described • 103ft FPB Workshop • pressure pump • detailed • Workshop • running gear and Conservancy plan feature • Sea Dart BACK ISSUES linkages • Minotaur Admiral’s Barge kit review • Modern Italian Navy design • 24 de Mayo described • 4in. JANUARY 1990 AVAILABLE AT £3.25/US Mk IX on CPI mounting • Police launch The 1989 Midland MEE + Converting photographed the Airfix Warspite + Deans Whaleback $6.50 EACH PLUS P&P/S&H FEBRUARY 1989 ASRL Review + R/C Scale event tips + Norderney/Mayfly conversion • D.l.Y. DIY Electronic Steam Whistle + Sea TO ORDER TURN TO PAGE 89 electronic r/c switchers • Tirpitz camou- Griffon Tug plan + Yacht mast and rig- flage described • Simple submarine • gingSOLD + HMS Gorgon modelled OUT + WHERE BACK ISSUES ARE EXHAUSTED, Swift PCF Boats detailed • Guns of the Modern Italian Navy Pt2 + PHOTOCOPIES OF SPECIFIC FEATURES ARE CoastalSOLD Forces • Workshop OUT • bilge Workshop,Resin -

Mainsheet April 2008.Pub
APRIL 2008 www.nssc.org.uk Racing has started for the hardy at Seaford. And I mean ‘hardy’. I can’t remember sailing off the beach in sleet and snow before! Hopefully it will have warmed up a bit by the time you read this. The work party weekends were a great success, with both sites looking much better thanks to the efforts of a pleasingly large number of workers. It made me start thinking just how many members are doing jobs around the place beyond the normal weekend duties. I won’t mention names, but these jobs include (but are by no means limited to): Bosuns’ team, maintenance of the buildings, berthing, disposing of abandoned boats, bar management, instructors, club house cleaning, school boat maintenance, site maintenance, mainsheet publication/distribution, duty rotas, sailing programs, administration, accounts, web site, training, social events, publicity, grass cutting, cadet organisation, people who carry a toolbox in the car just in case something needs fixing, etc. etc. etc.. Thanks to everyone for all the time you put in. It really is appreciated. The Open Day on 19th April needs more help from the members. We are opening up to members of the public to show them some of the attraction of sailing and our club in particular. If you can help during the day taking people for trial sails, displaying your boat, manning a side show for an hour or two or just be around to chat to visitors, your help would be very welcome. Also we need posters displayed beforehand in local shops and car windows.