A Deeper Dive Into Advanced and Future Directions in Treating Patients with Acute Myeloid Leukemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prior Approaches and Future Directions Marna Williams1, Anna Spreafico2, Kapil Vashisht3, Mary Jane Hinrichs4
Author Manuscript Published OnlineFirst on June 16, 2020; DOI: 10.1158/1535-7163.MCT-19-0993 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Patient Selection Strategies to Maximize Therapeutic Index of Antibody Drug Conjugates: Prior Approaches and Future Directions Marna Williams1, Anna Spreafico2, Kapil Vashisht3, Mary Jane Hinrichs4 1Translational Medicine, Oncology, AstraZeneca, Gaithersburg, USA 2Drug Development Program, Princess Margaret Cancer Centre, University Health Network, Toronto, ON, Canada 3AstraZeneca, Gaithersburg, USA. 4Early Development Oncology, Ipsen LLC, USA Corresponding author: Marna Williams Email: [email protected] Postal address: One MedImmune Way, Gaithersburg, MD, 20878 Phone: 301-398-1241 Fax: 240-306-1545 Running title Patient Selection Strategies for Antibody Drug Conjugates Keywords Antibody drug conjugates; therapeutic index; patient selection; biomarkers; cancer Conflicts of interest This study was funded by AstraZeneca. MW, KV and MJH are all current or former employees of AstraZeneca with stock/stock options in AstraZeneca. AS has been Advisory Board Consultant to Merck, Bristol-Myers Squibb, Novartis, Oncorus, Janssen, and has received Grant/Research support from Novartis, Bristol-Myers Squibb, Symphogen AstraZeneca/Medimmune, Merck, Bayer, Surface Oncology, Northern Biologics, Janssen Oncology/Johnson & Johnson, Roche, Regeneron, and Alkermes. Word count: Abstract: 197 Manuscript: 5,268 (excluding abstract) + 683 figure/table legends and footnotes Figures/tables: 5 (as agreed) 1 Downloaded from mct.aacrjournals.org on September 24, 2021. © 2020 American Association for Cancer Research. Author Manuscript Published OnlineFirst on June 16, 2020; DOI: 10.1158/1535-7163.MCT-19-0993 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. -

Predictive QSAR Tools to Aid in Early Process Development of Monoclonal Antibodies
Predictive QSAR tools to aid in early process development of monoclonal antibodies John Micael Andreas Karlberg Published work submitted to Newcastle University for the degree of Doctor of Philosophy in the School of Engineering November 2019 Abstract Monoclonal antibodies (mAbs) have become one of the fastest growing markets for diagnostic and therapeutic treatments over the last 30 years with a global sales revenue around $89 billion reported in 2017. A popular framework widely used in pharmaceutical industries for designing manufacturing processes for mAbs is Quality by Design (QbD) due to providing a structured and systematic approach in investigation and screening process parameters that might influence the product quality. However, due to the large number of product quality attributes (CQAs) and process parameters that exist in an mAb process platform, extensive investigation is needed to characterise their impact on the product quality which makes the process development costly and time consuming. There is thus an urgent need for methods and tools that can be used for early risk-based selection of critical product properties and process factors to reduce the number of potential factors that have to be investigated, thereby aiding in speeding up the process development and reduce costs. In this study, a framework for predictive model development based on Quantitative Structure- Activity Relationship (QSAR) modelling was developed to link structural features and properties of mAbs to Hydrophobic Interaction Chromatography (HIC) retention times and expressed mAb yield from HEK cells. Model development was based on a structured approach for incremental model refinement and evaluation that aided in increasing model performance until becoming acceptable in accordance to the OECD guidelines for QSAR models. -

Advances and Limitations of Antibody Drug Conjugates for Cancer
biomedicines Review Advances and Limitations of Antibody Drug Conjugates for Cancer Candice Maria Mckertish and Veysel Kayser * Sydney School of Pharmacy, Faculty of Medicine and Health, The University of Sydney, Sydney, NSW 2006, Australia; [email protected] * Correspondence: [email protected]; Tel.: +61-2-9351-3391 Abstract: The popularity of antibody drug conjugates (ADCs) has increased in recent years, mainly due to their unrivalled efficacy and specificity over chemotherapy agents. The success of the ADC is partly based on the stability and successful cleavage of selective linkers for the delivery of the payload. The current research focuses on overcoming intrinsic shortcomings that impact the successful devel- opment of ADCs. This review summarizes marketed and recently approved ADCs, compares the features of various linker designs and payloads commonly used for ADC conjugation, and outlines cancer specific ADCs that are currently in late-stage clinical trials for the treatment of cancer. In addition, it addresses the issues surrounding drug resistance and strategies to overcome resistance, the impact of a narrow therapeutic index on treatment outcomes, the impact of drug–antibody ratio (DAR) and hydrophobicity on ADC clearance and protein aggregation. Keywords: antibody drug conjugates; drug resistance; linkers; payloads; therapeutic index; target specific; ADC clearance; protein aggregation Citation: Mckertish, C.M.; Kayser, V. Advances and Limitations of Antibody Drug Conjugates for 1. Introduction Cancer. Biomedicines 2021, 9, 872. Conventional cancer therapy often entails a low therapeutic window and non-specificity https://doi.org/10.3390/ of chemotherapeutic agents that consequently affects normal cells with high mitotic rates biomedicines9080872 and provokes an array of adverse effects, and in some cases leads to drug resistance [1]. -

Patient Resource Free
PATIENT RESOURCE FREE Third Edition CancerUnderstanding Immunotherapy Published in partnership with CONTENT REVIEWED BY A DISTINGUISHED PRP MEDICAL PATIENT ADVISORY RESOURCE BOARD PUBLISHING® Understanding TABLE OF CONTENTS Cancer Immunotherapy Third Edition IN THIS GUIDE 1 Immunotherapy Today 2 The Immune System 4 Immunotherapy Strategies 6 Melanoma Survivor Story: Jane McNee Chief Executive Officer Mark A. Uhlig I didn’t look sick, so I didn’t want to act sick. Publisher Linette Atwood Having and treating cancer is only one part of your life. Co-Editor-in-Chief Charles M. Balch, MD, FACS Jane McNee, melanoma survivor Co-Editor-in-Chief Howard L. Kaufman, MD, FACS Senior Vice President Debby Easum 7 The Road to Immunotherapy Vice President, Operations Leann Sandifar 8 Cancer Types Managing Editor Lori Alexander, MTPW, ELS, MWC™ 14 Side Effects Senior Editors Dana Campbell Colleen Scherer 15 Glossary Graphic Designer Michael St. George 16 About Clinical Trials Medical Illustrator Todd Smith 16 Cancer Immunotherapy Clinical Trials by Disease Production Manager Jennifer Hiltunen 35 Support & Financial Resources Vice Presidents, Amy Galey Business Development Kathy Hungerford 37 Notes Stephanie Myers Kenney Account Executive Melissa Amaya Office Address 8455 Lenexa Drive CO-EDITORS-IN-CHIEF Overland Park, KS 66214 For Additional Information [email protected] Charles M. Balch, MD, FACS Advisory Board Visit our website at Professor of Surgery, The University of Texas PatientResource.com to read bios of MD Anderson Cancer Center our Medical and Patient Advisory Board. Editor-in-Chief, Patient Resource LLC Editor-in-Chief, Annals of Surgical Oncology Past President, Society of Surgical Oncology For Additional Copies: To order additional copies of Patient Resource Cancer Guide: Understanding Cancer Immunotherapy, Howard L. -

IMGN779, a Novel CD33-Targeting Antibody-Drug Conjugate with DNA Alkylating Activity, Exhibits Potent Antitumor Activity in Models of AML
Author Manuscript Published OnlineFirst on March 27, 2018; DOI: 10.1158/1535-7163.MCT-17-1077 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. IMGN779, a Novel CD33-Targeting Antibody-Drug Conjugate with DNA Alkylating Activity, Exhibits Potent Antitumor Activity in Models of AML Yelena Kovtun1*, Paul Noordhuis2*, Kathleen R. Whiteman1, Krystal Watkins1, Gregory E. Jones1, Lauren Harvey1, Katharine C. Lai1, Scott Portwood3, Sharlene Adams1, Callum M. Sloss1, Gerrit Jan Schuurhuis2, Gert Ossenkoppele2, Eunice S. Wang3, and Jan Pinkas1 1ImmunoGen, Inc., Waltham, Massachusetts. 2Department of Hematology, VU University Medical Center, Amsterdam, The Netherlands. 3Department of Medicine, Roswell Park Cancer Institute, Buffalo, New York *These authors contributed equally to the work Running Title: Preclinical activity of IMGN779 in AML Corresponding author: Yelena Kovtun, ImmunoGen Inc., 830 Winter St, Waltham, MA 02451. Phone: (781) 895-0716; Fax: (781) 895-0611; Email: [email protected] Potential conflict of interests: E.S. Wang received financial support from, and has served on an advisory board for, Immunogen Inc. There are no other competing interests to declare. 1 Downloaded from mct.aacrjournals.org on September 24, 2021. © 2018 American Association for Cancer Research. Author Manuscript Published OnlineFirst on March 27, 2018; DOI: 10.1158/1535-7163.MCT-17-1077 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Abstract The myeloid differentiation antigen CD33 has long been exploited as a target for antibody-based therapeutic approaches in acute myeloid leukemia (AML). Validation of this strategy was provided with the approval of the CD33-targeting antibody-drug conjugate (ADC) gemtuzumab ozogamicin in 2000; the clinical utility of this agent has however been hampered by safety concerns. -

2017 Immuno-Oncology Medicines in Development
2017 Immuno-Oncology Medicines in Development Adoptive Cell Therapies Drug Name Organization Indication Development Phase ACTR087 + rituximab Unum Therapeutics B-cell lymphoma Phase I (antibody-coupled T-cell receptor Cambridge, MA www.unumrx.com immunotherapy + rituximab) AFP TCR Adaptimmune liver Phase I (T-cell receptor cell therapy) Philadelphia, PA www.adaptimmune.com anti-BCMA CAR-T cell therapy Juno Therapeutics multiple myeloma Phase I Seattle, WA www.junotherapeutics.com Memorial Sloan Kettering New York, NY anti-CD19 "armored" CAR-T Juno Therapeutics recurrent/relapsed chronic Phase I cell therapy Seattle, WA lymphocytic leukemia (CLL) www.junotherapeutics.com Memorial Sloan Kettering New York, NY anti-CD19 CAR-T cell therapy Intrexon B-cell malignancies Phase I Germantown, MD www.dna.com ZIOPHARM Oncology www.ziopharm.com Boston, MA anti-CD19 CAR-T cell therapy Kite Pharma hematological malignancies Phase I (second generation) Santa Monica, CA www.kitepharma.com National Cancer Institute Bethesda, MD Medicines in Development: Immuno-Oncology 1 Adoptive Cell Therapies Drug Name Organization Indication Development Phase anti-CEA CAR-T therapy Sorrento Therapeutics liver metastases Phase I San Diego, CA www.sorrentotherapeutics.com TNK Therapeutics San Diego, CA anti-PSMA CAR-T cell therapy TNK Therapeutics cancer Phase I San Diego, CA www.sorrentotherapeutics.com Sorrento Therapeutics San Diego, CA ATA520 Atara Biotherapeutics multiple myeloma, Phase I (WT1-specific T lymphocyte South San Francisco, CA plasma cell leukemia www.atarabio.com -

Antibody–Drug Conjugates: the Last Decade
pharmaceuticals Review Antibody–Drug Conjugates: The Last Decade Nicolas Joubert 1,* , Alain Beck 2 , Charles Dumontet 3,4 and Caroline Denevault-Sabourin 1 1 GICC EA7501, Equipe IMT, Université de Tours, UFR des Sciences Pharmaceutiques, 31 Avenue Monge, 37200 Tours, France; [email protected] 2 Institut de Recherche Pierre Fabre, Centre d’Immunologie Pierre Fabre, 5 Avenue Napoléon III, 74160 Saint Julien en Genevois, France; [email protected] 3 Cancer Research Center of Lyon (CRCL), INSERM, 1052/CNRS 5286/UCBL, 69000 Lyon, France; [email protected] 4 Hospices Civils de Lyon, 69000 Lyon, France * Correspondence: [email protected] Received: 17 August 2020; Accepted: 10 September 2020; Published: 14 September 2020 Abstract: An armed antibody (antibody–drug conjugate or ADC) is a vectorized chemotherapy, which results from the grafting of a cytotoxic agent onto a monoclonal antibody via a judiciously constructed spacer arm. ADCs have made considerable progress in 10 years. While in 2009 only gemtuzumab ozogamicin (Mylotarg®) was used clinically, in 2020, 9 Food and Drug Administration (FDA)-approved ADCs are available, and more than 80 others are in active clinical studies. This review will focus on FDA-approved and late-stage ADCs, their limitations including their toxicity and associated resistance mechanisms, as well as new emerging strategies to address these issues and attempt to widen their therapeutic window. Finally, we will discuss their combination with conventional chemotherapy or checkpoint inhibitors, and their design for applications beyond oncology, to make ADCs the magic bullet that Paul Ehrlich dreamed of. Keywords: antibody–drug conjugate; ADC; bioconjugation; linker; payload; cancer; resistance; combination therapies 1. -

Tables-Of-Phase-3-Mabs.Pdf
Table 3. Monoclonal antibodies in Phase 2/3 or 3 clinical studies for cancer indications Most advanced Primary sponsoring company INN or code name Molecular format Target(s) phase Phase 3 indications Therapeutic area Janssen Research & Development, LLC JNJ-56022473 Humanized mAb CD123 Phase 2/3 Acute myeloid leukemia Cancer Murine IgG1, Actinium Pharmaceuticals Iomab-B radiolabeled CD45 Phase 3 Acute myeloid leukemia Cancer Humanized IgG1, Seattle Genetics Vadastuximab talirine ADC CD33 Phase 3 Acute myeloid leukemia Cancer TG Therapeutics Ublituximab Chimeric IgG1 CD20 Phase 3 Chronic lymphocytic leukemia Cancer Xencor XMAB-5574, MOR208 Humanized IgG1 CD19 Phase 2/3 Diffuse large B-cell lymphoma Cancer Moxetumomab Murine IgG1 dsFv, AstraZeneca/MedImmune LLC pasudotox immunotoxin CD22 Phase 3 Hairy cell leukemia Cancer Humanized scFv, Viventia Bio Oportuzumab monatox immunotoxin EpCAM Phase 3 Bladder cancer Cancer scFv-targeted liposome containing Merrimack Pharmaceuticals MM-302 doxorubicin HER2 Phase 2/3 Breast cancer Cancer MacroGenics Margetuximab Chimeric IgG1 HER2 Phase 3 Breast cancer Cancer Gastric cancer or gastroesophageal junction Gilead Sciences GS-5745 Humanized IgG4 MMP9 Phase 3 adenocarcinoma; ulcerative colitis (Phase 2/3) Cancer; Immune-mediated disorders Depatuxizumab Humanized IgG1, AbbVie mafodotin ADC EGFR Phase 2/3 Glioblastoma Cancer AstraZeneca/MedImmune LLC Tremelimumab Human IgG2 CTLA4 Phase 3 NSCLC, head & neck cancer, bladder cancer Cancer NSCLC, head & neck cancer, bladder cancer, breast AstraZeneca/MedImmune -

Bloomberg Intelligence: ASH Planner
58th Annual Meeting and Exposition (December 3-6, 2016) Bloomberg Intelligence: ASH Planner Start Time End Time Day Location Room Company (s) Drug (s) Presentation Abstract # Manchester Grand Grand Hall Targeting of JAK/STAT Signaling to Reverse Stroma-Induced Cytoprotection Against BCL2 Antagonist 7:45 AM 08:00AM 12/03/16 AbbVie / Roche Venclexta 32 Hyatt San Diego: D Venetoclax in Acute Myeloid Leukemia San Diego A CD47xCD19 Bispecific Antibody That Remodels the Tumor Microenvironment for Improved Killing and 7:45 AM 08:00AM 12/03/16 Room 5AB Novimmune S.A. NA 44 Convention Center: Provokes a Memory Immune Response to Cancer B Cells San Diego 7:45 AM 08:00AM 12/03/16 Room 6AB Juno JCAR014 CD19 CAR-T Cells Are Highly Effective in Ibrutinib-Refractory Chronic Lymphocytic Leukemia 56 Convention Center: San Diego Implications of Concurrent Ibrutinib Therapy on CAR T-Cell Manufacturing and Phenotype and on Clinical 8:15 AM 08:30AM 12/03/16 Room 6AB AbbVie / J&J Imbruvica 58 Convention Center: Outcomes Following CD19-Targeted CAR T-Cell Administration in Adults with Relapsed/Refractory CLL Bristol-Myers San Diego 8:30 AM 08:45AM 12/03/16 Room 6AB Squibb / Ono / Opdivo / Imbruvica Nivolumab Combined with Ibrutinib for CLL and Richter Transformation: A Phase II Trial 59 Convention Center: AbbVie / J&J Manchester Grand Grand Hall Romiplostim in Patients Undergoing Allogeneic Stem Cell Transplantation: Results of a Phase I/II Multicenter 8:30 AM 08:45AM 12/03/16 Amgen romiplostim 65 Hyatt San Diego: B Trial San Diego AstraZeneca / Acalabrutinib -

Loncastuximab Tesirine), a Novel Pyrrolobenzodiazepine-Based Antibody–Drug Conjugate, in Relapsed/ Refractory B-Cell Non-Hodgkin Lymphoma Brad S
Published OnlineFirst November 4, 2019; DOI: 10.1158/1078-0432.CCR-19-0711 Clinical Trials: Targeted Therapy Clinical Cancer Research A Phase I Study of ADCT-402 (Loncastuximab Tesirine), a Novel Pyrrolobenzodiazepine-Based Antibody–Drug Conjugate, in Relapsed/ Refractory B-Cell Non-Hodgkin Lymphoma Brad S. Kahl1, Mehdi Hamadani2, John Radford3, Carmelo Carlo-Stella4, Paolo Caimi5, Erin Reid6, Jay M. Feingold7, Kirit M. Ardeshna8, Melhem Solh9, Leonard T. Heffner10, David Ungar7, Shui He7, Joseph Boni7, Karin Havenith11, and Owen A. O'Connor12 Abstract Purpose: ADCT-402 (loncastuximab tesirine) is an anti- 200 mg/kg. Treatment-emergent adverse events (TEAEs) were body–drug conjugate comprising a CD19-targeting antibody experienced by 87/88 (98.9%) patients. Most common TEAEs and pyrrolobenzodiazepine dimers. A first-in-human study (20% of patients) were hematologic abnormalities, fatigue, evaluated the safety and preliminary clinical activity of lon- edema, liver test abnormalities, nausea, rash, and dyspnea. castuximab tesirine in patients with B-cell non-Hodgkin lym- Grade 3 TEAEs (5% of patients) included hematologic phoma (NHL). abnormalities, liver test abnormalities, fatigue, and dyspnea. Experimental Design: A multicenter, phase I, dose- Overall response rate at doses 120 mg/kg was 59.4% (41 of 69 escalation and dose-expansion study enrolled patients ages patients; 40.6% complete response; 18.8% partial response). 18 years with relapsed/refractory (R/R) B-cell NHL. Patients Median duration of response, progression-free survival, and received loncastuximab tesirine every 3 weeks at doses overall survival (all doses) were 4.8, 5.5, and 11.6 months, assigned by a 3þ3 dose-escalation design. -
OHC Clinical Trials List V4
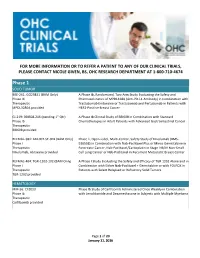
FOR MORE INFORMATION OR TO REFER A PATIENT TO ANY OF OUR CLINICAL TRIALS, PLEASE CONTACT NICOLE GIVEN, BS, OHC RESEARCH DEPARTMENT AT 1-800-710-4674 Phase 1 SOLID TUMOR BRE-261: GO29831 (BAM Only) A Phase Ib, Randomized, Two-Arm Study Evaluating the Safety and Phase Ib Pharmacokinetics of MPDL328A (Anti-PD-L1 Antibody) in Combination with Therapeutic Trastuzumab Emtansine or Trastuzumab and Pertuzumab in Patients with MPDL3280A provided HER2-Positive Breast Cancer GI-219: BBI608-246 (pending 1st Qtr) A Phase Ib Clinical Study of BBI608 in Combination with Standard Phase Ib Chemotherapies in Adult Patients with Advanced Gastrointestinal Cancer Therapeutic BBI608 provided REFMAL-381: ABI-007-ST-001 (BAM Only) Phase 1, Open-Label, Multi-Center, Safety Study of Nivolumab (BMS- Phase I 936558) in Combination with Nab-Paclitaxel Plus or Minus Gemcitabine in Therapeutic Pancreatic Cancer, Nab-Paclitaxel/Carboplatin in Stage IIIB/IV Non-Small Nivolumab, Abraxane provided Cell Lung Cancer or Nab-Paclitaxel in Recurrent Metastatic Breast Cancer REFMAL-404: TGR-1202-102 (BAM Only) A Phase I Study Evaluating the Safety and Efficacy of TGR 1202 Alone and in Phase I Combination with Either Nab-Paclitaxel + Gemcitabine or with FOLFOX in Therapeutic Patients with Select Relapsed or Refractory Solid Tumors TGR-1202 provided HEMATOLOGY MM-56: CFZ013 Phase Ib Study of Carfilzomib Administered Once Weekly in Combination Phase Ib with Lenalidomide and Dexamethasone in Subjects with Multiple Myeloma Therapeutic Carfilzomib provided Page 1 of 20 January 11, -

Orphan Drug Dummy File
Orphan Drug Designations and Approvals List as of 09‐01‐2016 Governs October 1, 2016 ‐ December 31, 2016 Row Contact Generic Name Trade Name Designation Date Designation Num Company/Sponsor 1 1. Prevention of secondary carnitine deficiency in valproic acid toxicity 2. Treatment of secondary carnitine deficiency in Sigma-Tau levocarnitine Carnitor 11/15/1989 valproic acid toxicity Pharmaceuticals, Inc. 2 1. Treatment of graft versus host disease in patients receiving bone marrow transplantation 2. Prevention of graft versus host disease in patients receiving Pediatric thalidomide n/a 9/19/1988 bone marrow transplantation Pharmaceuticals, Inc. 3 A Diagnostic for the management Advanced Imaging Theranost 68 Ga RGD n/a 10/1/2014 of Moyamoya disease (MMD) Projects, LLC (AIP) 4 Cadila heat killed Mycobacterium w Pharmaceuticals immunomodulator Cadi Mw 9/3/2004 Active tuberculosis Limited, Inc. 5 Adjunct to cytokine therapy in the treatment of acute myeloid Histamine Ceplene 12/15/1999 leukemia. EpiCept Corporation 6 Adjunct to surgery in cases of rh-microplasmin, ocriplasmin Jetrea 3/16/2004 pediatric vitrectomy ThromboGenics Inc. 7 Adjunct to the non-operative management of secreting cutaneous fistulas of the stomach, duodenum, small intestine (jejunum and ileum), or Ferring Laboratories, Somatostatin Zecnil 6/20/1988 pancreas. Inc. Page 1 of 377 Orphan Drug Designations and Approvals List as of 09‐01‐2016 Governs October 1, 2016 ‐ December 31, 2016 Row Contact Generic Name Trade Name Designation Date Designation Num Company/Sponsor 8 Adjunct to whole brain radiation therapy for the treatment of brain metastases in patients with Allos Therapeutics, efaproxiral n/a 7/28/2004 breast cancer Inc.