Forkhead Box F1 (FOXF1) Is an Essential Effector of the PAX3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Produktinformation
Produktinformation Diagnostik & molekulare Diagnostik Laborgeräte & Service Zellkultur & Verbrauchsmaterial Forschungsprodukte & Biochemikalien Weitere Information auf den folgenden Seiten! See the following pages for more information! Lieferung & Zahlungsart Lieferung: frei Haus Bestellung auf Rechnung SZABO-SCANDIC Lieferung: € 10,- HandelsgmbH & Co KG Erstbestellung Vorauskassa Quellenstraße 110, A-1100 Wien T. +43(0)1 489 3961-0 Zuschläge F. +43(0)1 489 3961-7 [email protected] • Mindermengenzuschlag www.szabo-scandic.com • Trockeneiszuschlag • Gefahrgutzuschlag linkedin.com/company/szaboscandic • Expressversand facebook.com/szaboscandic SANTA CRUZ BIOTECHNOLOGY, INC. MAGE-D4/MAGE-D4B CRISPR/Cas9 KO Plasmid (h): sc-418394 BACKGROUND APPLICATIONS The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and MAGE-D4/MAGE-D4B CRISPR/Cas9 KO Plasmid (h) is recommended for the CRISPR-associated protein (Cas9) system is an adaptive immune response disruption of gene expression in human cells. defense mechanism used by archea and bacteria for the degradation of foreign genetic material (4,6). This mechanism can be repurposed for other 20 nt non-coding RNA sequence: guides Cas9 functions, including genomic engineering for mammalian systems, such as to a specific target location in the genomic DNA gene knockout (KO) (1,2,3,5). CRISPR/Cas9 KO Plasmid products enable the U6 promoter: drives gRNA scaffold: helps Cas9 identification and cleavage of specific genes by utilizing guide RNA (gRNA) expression of gRNA bind to target DNA sequences derived from the Genome-scale CRISPR Knock-Out (GeCKO) v2 library developed in the Zhang Laboratory at the Broad Institute (3,5). Termination signal Green Fluorescent Protein: to visually REFERENCES verify transfection CRISPR/Cas9 Knockout Plasmid CBh (chicken β-Actin 1. -

Genome-Wide Transcriptional Sequencing Identifies Novel Mutations in Metabolic Genes in Human Hepatocellular Carcinoma DAOUD M
CANCER GENOMICS & PROTEOMICS 11 : 1-12 (2014) Genome-wide Transcriptional Sequencing Identifies Novel Mutations in Metabolic Genes in Human Hepatocellular Carcinoma DAOUD M. MEERZAMAN 1,2 , CHUNHUA YAN 1, QING-RONG CHEN 1, MICHAEL N. EDMONSON 1, CARL F. SCHAEFER 1, ROBERT J. CLIFFORD 2, BARBARA K. DUNN 3, LI DONG 2, RICHARD P. FINNEY 1, CONSTANCE M. CULTRARO 2, YING HU1, ZHIHUI YANG 2, CU V. NGUYEN 1, JENNY M. KELLEY 2, SHUANG CAI 2, HONGEN ZHANG 2, JINGHUI ZHANG 1,4 , REBECCA WILSON 2, LAUREN MESSMER 2, YOUNG-HWA CHUNG 5, JEONG A. KIM 5, NEUNG HWA PARK 6, MYUNG-SOO LYU 6, IL HAN SONG 7, GEORGE KOMATSOULIS 1 and KENNETH H. BUETOW 1,2 1Center for Bioinformatics and Information Technology, National Cancer Institute, Rockville, MD, U.S.A.; 2Laboratory of Population Genetics, National Cancer Institute, National Cancer Institute, Bethesda, MD, U.S.A.; 3Basic Prevention Science Research Group, Division of Cancer Prevention, National Cancer Institute, Bethesda, MD, U.S.A; 4Department of Biotechnology/Computational Biology, St. Jude Children’s Research Hospital, Memphis, TN, U.S.A.; 5Department of Internal Medicine, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea; 6Department of Internal Medicine, University of Ulsan College of Medicine, Ulsan University Hospital, Ulsan, Korea; 7Department of Internal Medicine, College of Medicine, Dankook University, Cheon-An, Korea Abstract . We report on next-generation transcriptome Worldwide, liver cancer is the fifth most common cancer and sequencing results of three human hepatocellular carcinoma the third most common cause of cancer-related mortality (1). tumor/tumor-adjacent pairs. -

Appendix 2. Significantly Differentially Regulated Genes in Term Compared with Second Trimester Amniotic Fluid Supernatant
Appendix 2. Significantly Differentially Regulated Genes in Term Compared With Second Trimester Amniotic Fluid Supernatant Fold Change in term vs second trimester Amniotic Affymetrix Duplicate Fluid Probe ID probes Symbol Entrez Gene Name 1019.9 217059_at D MUC7 mucin 7, secreted 424.5 211735_x_at D SFTPC surfactant protein C 416.2 206835_at STATH statherin 363.4 214387_x_at D SFTPC surfactant protein C 295.5 205982_x_at D SFTPC surfactant protein C 288.7 1553454_at RPTN repetin solute carrier family 34 (sodium 251.3 204124_at SLC34A2 phosphate), member 2 238.9 206786_at HTN3 histatin 3 161.5 220191_at GKN1 gastrokine 1 152.7 223678_s_at D SFTPA2 surfactant protein A2 130.9 207430_s_at D MSMB microseminoprotein, beta- 99.0 214199_at SFTPD surfactant protein D major histocompatibility complex, class II, 96.5 210982_s_at D HLA-DRA DR alpha 96.5 221133_s_at D CLDN18 claudin 18 94.4 238222_at GKN2 gastrokine 2 93.7 1557961_s_at D LOC100127983 uncharacterized LOC100127983 93.1 229584_at LRRK2 leucine-rich repeat kinase 2 HOXD cluster antisense RNA 1 (non- 88.6 242042_s_at D HOXD-AS1 protein coding) 86.0 205569_at LAMP3 lysosomal-associated membrane protein 3 85.4 232698_at BPIFB2 BPI fold containing family B, member 2 84.4 205979_at SCGB2A1 secretoglobin, family 2A, member 1 84.3 230469_at RTKN2 rhotekin 2 82.2 204130_at HSD11B2 hydroxysteroid (11-beta) dehydrogenase 2 81.9 222242_s_at KLK5 kallikrein-related peptidase 5 77.0 237281_at AKAP14 A kinase (PRKA) anchor protein 14 76.7 1553602_at MUCL1 mucin-like 1 76.3 216359_at D MUC7 mucin 7, -

Genome-Wide Analysis of DNA Methylation, Copy Number Variation, and Gene Expression in Monozygotic Twins Discordant for Primary Biliary Cirrhosis
UC Davis UC Davis Previously Published Works Title Genome-wide analysis of DNA methylation, copy number variation, and gene expression in monozygotic twins discordant for primary biliary cirrhosis. Permalink https://escholarship.org/uc/item/34d4m5nk Journal Frontiers in immunology, 5(MAR) ISSN 1664-3224 Authors Selmi, Carlo Cavaciocchi, Francesca Lleo, Ana et al. Publication Date 2014 DOI 10.3389/fimmu.2014.00128 Peer reviewed eScholarship.org Powered by the California Digital Library University of California ORIGINAL RESEARCH ARTICLE published: 28 March 2014 doi: 10.3389/fimmu.2014.00128 Genome-wide analysis of DNA methylation, copy number variation, and gene expression in monozygotic twins discordant for primary biliary cirrhosis Carlo Selmi 1,2*, Francesca Cavaciocchi 1,3, Ana Lleo4, Cristina Cheroni 5, Raffaele De Francesco5, Simone A. Lombardi 1, Maria De Santis 1,3, Francesca Meda1, Maria Gabriella Raimondo1, Chiara Crotti 1, Marco Folci 1, Luca Zammataro1, Marlyn J. Mayo6, Nancy Bach7, Shinji Shimoda8, Stuart C. Gordon9, Monica Miozzo10,11, Pietro Invernizzi 4, Mauro Podda1, Rossana Scavelli 5, Michelle R. Martin12, Michael F. Seldin13,14, Janine M. LaSalle 12 and M. Eric Gershwin2 1 Division of Rheumatology and Clinical Immunology, Humanitas Clinical and Research Center, Milan, Italy 2 Division of Rheumatology, Allergy, and Clinical Immunology, University of California at Davis, Davis, CA, USA 3 BIOMETRA Department, University of Milan, Milan, Italy 4 Liver Unit and Center for Autoimmune Liver Diseases, Humanitas Clinical and Research Center, Milan, Italy 5 National Institute of Molecular Genetics (INGM), Milan, Italy 6 University of Texas Southwestern, Dallas, TX, USA 7 Mt. Sinai University, NewYork, NY, USA 8 Clinical Research Center, National Nagasaki Medical Center, Nagasaki, Japan 9 Henry Ford Hospital, Detroit, MI, USA 10 Department of Pathophysiology and Transplantation, University of Milan, Milan, Italy 11 Division of Pathology, Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milan, Italy 12 Genome Center and M.I.N.D. -

Karla Alejandra Vizcarra Zevallos Análise Da Função De Genes
Karla Alejandra Vizcarra Zevallos Análise da função de genes candidatos à manutenção da inativação do cromossomo X em humanos Dissertação apresentada ao Pro- grama de Pós‐Graduação Inter- unidades em Biotecnologia USP/ Instituto Butantan/ IPT, para obtenção do Título de Mestre em Ciências. São Paulo 2017 Karla Alejandra Vizcarra Zevallos Análise da função de genes candidatos à manutenção da inativação do cromossomo X em humanos Dissertação apresentada ao Pro- grama de Pós‐Graduação Inter- unidades em Biotecnologia do Instituto de Ciências Biomédicas USP/ Instituto Butantan/ IPT, para obtenção do Título de Mestre em Ciências. Área de concentração: Biotecnologia Orientadora: Profa. Dra. Lygia da Veiga Pereira Carramaschi Versão corrigida. A versão original eletrônica encontra-se disponível tanto na Biblioteca do ICB quanto na Biblioteca Digital de Teses e Dissertações da USP (BDTD) São Paulo 2017 UNIVERSIDADE DE SÃO PAULO Programa de Pós-Graduação Interunidades em Biotecnologia Universidade de São Paulo, Instituto Butantan, Instituto de Pesquisas Tecnológicas Candidato(a): Karla Alejandra Vizcarra Zevallos Título da Dissertação: Análise da função de genes candidatos à manutenção da inativação do cromossomo X em humanos Orientador: Profa. Dra. Lygia da Veiga Pereira Carramaschi A Comissão Julgadora dos trabalhos de Defesa da Dissertação de Mestrado, em sessão pública realizada a ........./......../.........., considerou o(a) candidato(a): ( ) Aprovado(a) ( ) Reprovado(a) Examinador(a): Assinatura: .............................................................................. -

Systems Physiology and Nutrition In
SYSTEMS PHYSIOLOGY AND NUTRITION IN DAIRY CATTLE: APPLICATIONS OF OMICS AND BIOINFORMATICS TO BETTER UNDERSTAND THE HEPATIC METABOLOMICS AND TRANSCRIPTOMICS ADAPTATIONS IN TRANSITION DAIRY COWS BY KHURAM SHAHZAD DISSERTATION Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Informatics in the Graduate College of the University of Illinois at Urbana-Champaign, 2017 Urbana, Illinois Doctoral Committee: Associate Professor, Juan J. Loor, Chair Professor Gustavo Caetano-Anolles Associate Professor, Juan Steibel, Michigan State University Assistant Professor Phil Cardoso ABSTRACT Application of systems concepts to better understand physiological and metabolic changes in dairy cows during the transition into lactation could enhance our understanding about the role of nutrients in helping to meet the animal’s requirements for optimal production and health. Four different analyses focused on the liver were conducted to analyze metabolic disorder or thermal stress. The first three analyses dealt with supplementation of methionine to prevent clinical ketosis development in high-genetic merit dairy cows. Four groups of cows were formed retrospectively based on clinical health evaluated at 1 week postpartum: cows that remained healthy (OVE), cows that developed ketosis (K), and healthy cows supplemented with one of two commercial methionine products [Smartamine M (SM), and MetaSmart (MS)]. The liver tissue samples (n = 6/group) were harvested at -10 d before calving, and were used for metabolomics (GC-MS, LC-MS; Metabolon Inc.) and transcriptomics (44K-whole-transcriptome microarray; Agilent) analyses. Therefore, the main goals of the analyses were to 1) uncover metabolome and transcriptome patterns in the prepartum liver that were unique to those cows that became ketotic postpartum, and to 2) uncover unique patterns affected by supplemental methionine. -

Gender-Associated Genomic Differences in Colorectal Cancer: Clinical Insight from Feminization of Male Cancer Cells
Int. J. Mol. Sci. 2014, 15, 17344-17365; doi:10.3390/ijms151017344 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Article Gender-Associated Genomic Differences in Colorectal Cancer: Clinical Insight from Feminization of Male Cancer Cells Rola H. Ali 1, Makia J. Marafie 2, Milad S. Bitar 3, Fahad Al-Dousari 4, Samar Ismael 4, Hussain Bin Haider 1, Waleed Al-Ali 1, Sindhu P. Jacob 1 and Fahd Al-Mulla 1,* 1 Department of Pathology, Faculty of Medicine, Health Sciences Center, Kuwait University, P.O. Box 24923, Safat 13110, Kuwait; E-Mails: [email protected] (R.H.A.); [email protected] (H.B.H.); [email protected] (W.A.-A.); [email protected] (S.P.J.) 2 Kuwait Medical Genetics Center, Ministry of Health, Safat 13001, Kuwait; E-Mail: [email protected] 3 Department of Pharmacology, Faculty of Medicine, Health Sciences Center, Kuwait University, P.O. Box 24923, Safat 13110, Kuwait; E-Mail: [email protected] 4 Department of Forensic Evidence, Ministry of Interior, P.O. Box 12500, Shamiya 71655, Kuwait; E-Mails: [email protected] (F.A.-D); [email protected] (S.I.) * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +965-677-710-40; Fax: +965-253-389-05. External Editor: Bing Yan Received: 27 May 2014; in revised form: 15 September 2014 / Accepted: 16 September 2014 / Published: 29 September 2014 Abstract: Gender-related differences in colorectal cancer (CRC) are not fully understood. Recent studies have shown that CRC arising in females are significantly associated with CpG island methylator phenotype (CIMP-high). -

Characterisation of the Potential of Probiotics Or Their Extracts As Therapy for Skin
Characterisation of the potential of probiotics or their extracts as therapy for skin A thesis submitted to the University of Manchester for the Degree of Doctor of Philosophy in the Faculty of Medical and Human Sciences 2014 Walaa Mohammedsaeed, Master of Science (MSc) School of Medicine Table of Contents Contents Table of Contents .............................................................................................................. 2 Table of Figures ................................................................................................................ 5 List of Tables .................................................................................................................... 8 List of Abbreviations ........................................................................................................ 9 1 Abstract ....................................................................................................................... 11 2 Declaration .................................................................................................................. 12 3 Copyright Statement .................................................................................................... 13 4 Acknowledgements ...................................................................................................... 14 5 The author ................................................................................................................... 15 6 Publications arising from this Thesis ........................................................................... -
Genetic Screening Approaches to Cancer Driver Characterization and Synthetic Lethal Target Discovery
Genetic Screening Approaches to Cancer Driver Characterization and Synthetic Lethal Target Discovery The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Mengwasser, Kristen Elizabeth. 2018. Genetic Screening Approaches to Cancer Driver Characterization and Synthetic Lethal Target Discovery. Doctoral dissertation, Harvard University, Graduate School of Arts & Sciences. Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:41121232 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA Genetic Screening Approaches to Cancer Driver Characterization and Synthetic Lethal Target Discovery A dissertation presented by Kristen Elizabeth Mengwasser to The Division of Medical Sciences in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the subject of Biological and Biomedical Sciences Harvard University Cambridge, Massachusetts May 2018 © 2018 Kristen Elizabeth Mengwasser All rights reserved. Dissertation Advisor: Dr. Stephen J Elledge Kristen Elizabeth Mengwasser Genetic Screening Approaches to Cancer Driver Characterization and Synthetic Lethal Target Discovery Abstract Advances in genetic screening technology have expanded the toolkit for systematic perturbation of gene function. While the CRISPR-Cas9 system robustly probes genetic loss-of-function in mammalian cells, a barcoded ORFeome library offers the opportunity to systematically study genetic gain-of-function. We employed these two screening tools for three purposes. First, we performed shRNA and CRISPR-based screens for synthetic lethality with BRCA2 deficiency, in two pairs of BRCA2 isogenic cell lines. -
Identification of MLL-AF9 Related Target Genes and Micrornas Involved in Leukemogenesis
Identification of MLL-AF9 related target genes and microRNAs involved in leukemogenesis Dissertation zur Erlangung des Doktorgrades der Naturwissenschaften (Dr. rer. nat.) an der Fakultät für Biologie der Ludwig-Maximilians-Universität München Durchgeführt am Forschungszentrum des Dr. von Haunerschen Kinderspitals der Ludwig-Maximilians-Universität München vorgelegt von Katrin Kristina Fleischmann München, 3. Mai 2012 Erstgutachterin: Frau Prof. Dr. Elisabeth Weiss Zweitgutachter: Herr Prof. Dr. Michael Schleicher Sondergutachter: Herr Prof. Dr. Adelbert Roscher Tag der Abgabe: 03.05.2012 Tag der mündlichen Prüfung: 17.09.2012 What is a scientist after all? It is a curious man looking through a keyhole, the keyhole of nature, trying to know what's going on. Jacques Yves Cousteau Preamble and Acknowledgments How to explain the change from evolutionary ecology to tumor biology? After my diploma thesis in evolutionary ecology and a major in ecology, I was facing some skepticism while being interviewed for PhD positions in the biomedical field. What was my motivation to study biology? Why do I continue to feel this strong enthusiasm for this field? For me, it was always the grand question “How does life work?” that drove me and which may interconnect almost every aspect within natural sciences. Only when we strive to get answers to this grand question we may reach an understanding as to what happens in disease. I am profoundly grateful to my dear colleagues Dr. Julia von Frowein, Dr. Thomas Magg and Dr. Uta Fuchs who supported me to become one of their colleagues at the research center of the Dr. von Haunerschen Kinderspital. Since then, innumerable great and inspiring discussions allied us. -
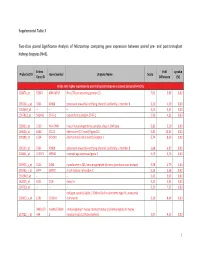
Supplemental Table 3 Two-Class Paired Significance Analysis of Microarrays Comparing Gene Expression Between Paired
Supplemental Table 3 Two‐class paired Significance Analysis of Microarrays comparing gene expression between paired pre‐ and post‐transplant kidneys biopsies (N=8). Entrez Fold q‐value Probe Set ID Gene Symbol Unigene Name Score Gene ID Difference (%) Probe sets higher expressed in post‐transplant biopsies in paired analysis (N=1871) 218870_at 55843 ARHGAP15 Rho GTPase activating protein 15 7,01 3,99 0,00 205304_s_at 3764 KCNJ8 potassium inwardly‐rectifying channel, subfamily J, member 8 6,30 4,50 0,00 1563649_at ‐‐ ‐‐ ‐‐ 6,24 3,51 0,00 1567913_at 541466 CT45‐1 cancer/testis antigen CT45‐1 5,90 4,21 0,00 203932_at 3109 HLA‐DMB major histocompatibility complex, class II, DM beta 5,83 3,20 0,00 204606_at 6366 CCL21 chemokine (C‐C motif) ligand 21 5,82 10,42 0,00 205898_at 1524 CX3CR1 chemokine (C‐X3‐C motif) receptor 1 5,74 8,50 0,00 205303_at 3764 KCNJ8 potassium inwardly‐rectifying channel, subfamily J, member 8 5,68 6,87 0,00 226841_at 219972 MPEG1 macrophage expressed gene 1 5,59 3,76 0,00 203923_s_at 1536 CYBB cytochrome b‐245, beta polypeptide (chronic granulomatous disease) 5,58 4,70 0,00 210135_s_at 6474 SHOX2 short stature homeobox 2 5,53 5,58 0,00 1562642_at ‐‐ ‐‐ ‐‐ 5,42 5,03 0,00 242605_at 1634 DCN decorin 5,23 3,92 0,00 228750_at ‐‐ ‐‐ ‐‐ 5,21 7,22 0,00 collagen, type III, alpha 1 (Ehlers‐Danlos syndrome type IV, autosomal 201852_x_at 1281 COL3A1 dominant) 5,10 8,46 0,00 3493///3 IGHA1///IGHA immunoglobulin heavy constant alpha 1///immunoglobulin heavy 217022_s_at 494 2 constant alpha 2 (A2m marker) 5,07 9,53 0,00 1 202311_s_at -

A CRISPR Screen to Identify Combination Therapies of Cytotoxic
CRISPRi Screens to Identify Combination Therapies for the Improved Treatment of Ovarian Cancer By Erika Daphne Handly B.S. Chemical Engineering Brigham Young University, 2014 Submitted to the Department of Biological Engineering in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biological Engineering at the MASSACHUSETTS INSTITUTE OF TECHNOLOGY February 2021 © 2020 Massachusetts Institute of Technology. All rights reserved. Signature of author………………………………………………………………………………… Erika Handly Department of Biological Engineering February 2021 Certified by………………………………………………………………………………………… Michael Yaffe Director MIT Center for Precision Cancer Medicine Department of Biological Engineering and Biology Thesis Supervisor Accepted by………………………………………………………………………………………... Katharina Ribbeck Professor of Biological Engineering Chair of Graduate Program, Department of Biological Engineering Thesis Committee members Michael T. Hemann, Ph.D. Associate Professor of Biology Massachusetts Institute of Technology Douglas A. Lauffenburger, Ph.D. (Chair) Ford Professor of Biological Engineering, Chemical Engineering, and Biology Massachusetts Institute of Technology Michael B. Yaffe, M.D., Ph.D. (Thesis Supervisor) David H. Koch Professor of Science Prof. of Biology and Biological Engineering Massachusetts Institute of Technology 2 CRISPRi Screens to Identify Combination Therapies for the Improved Treatment of Ovarian Cancer By Erika Daphne Handly B.S. Chemical Engineering Brigham Young University, 2014 Submitted to the Department of Biological Engineering in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biological Engineering ABSTRACT Ovarian cancer is the fifth leading cause of cancer death for women in the United States, with only modest improvements in patient survival in the past few decades. Standard-of-care consists of surgical debulking followed by a combination of platinum and taxane agents, but relapse and resistance frequently occur.