Host Cell Death in Legionella Pneumophila Pathogenesis and Immunity Wenhan Zhu Purdue University
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
University of Cincinnati
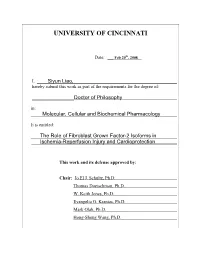
UNIVERSITY OF CINCINNATI Date: ___ Feb 20th, 2008 I, Siyun Liao, hereby submit this work as part of the requirements for the degree of: ________________Doctor of Philosophy in: Molecular, Cellular and Biochemical Pharmacology It is entitled: ____The Role of Fibroblast Grown Factor-2 Isoforms in ___Ischemia-Reperfusion Injury and Cardioprotection This work and its defense approved by: Chair: Jo El J. Schultz, Ph.D. Thomas Doetschman, Ph.D. W. Keith Jones, Ph.D. Evangelia G. Kranias, Ph.D. Mark Olah, Ph.D. Hong-Sheng Wang, Ph.D. THE ROLE OF FIBROBLAST GROWTH FACTOR-2 ISOFORMS IN ISCHEMIA- REPERFUSION INJURY AND CARDIOPROTECTION A dissertation submitted to the Division of Graduate Studies of the University of Cincinnati In partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY In the Department of Pharmacology and Cell Biophysics 2007 by Siyun Liao B.S. China Pharmaceutical University, 2000 Committee Chair: Dr. Jo El J. Schultz ii Abstract Cardiovascular disease (CVD) remains the leading cause of death in the United States and in the developing world, with ischemic heart disease the second most common form of CVD. Experimental and clinical studies have demonstrated that a number of interventions, including brief periods of ischemia or hypoxia and certain endogenous molecules such as growth factors, opioids, adenosine or pharmacological agents are capable of protecting the heart against post- ischemic cardiac dysfunction, arrhythmias and myocardial infarction. One of these growth factors, fibroblast growth factor-2 (FGF2), has been implicated to be a cardioprotective molecule. FGF2 consists of multiple protein isoforms (low molecular weight, LMW, and high molecular weight, HMW) produced by alternative translation from the Fgf2 gene and these protein isoforms are localized to different cellular compartments indicating unique biological activity. -

Tpa PROMOTES POSTNATAL CORTICAL NEURON SURVIVAL I
tPA PROMOTES POSTNATAL CORTICAL NEURON SURVIVAL i Tissue plasminogen activator (tPA) promotes postnatal cortical neuron survival in vitro via JAK2- and mTOR-dependent mechanisms by Julia A. Grummisch A thesis submitted to the Faculty of Graduate and Postdoctoral Affairs in partial fulfillment of the requirements for the degree of Master of Science in Neuroscience Carleton University Ottawa, Ontario © 2015 Julia A. Grummisch tPA PROMOTES POSTNATAL CORTICAL NEURON SURVIVAL ii Abstract Tissue plasminogen activator (tPA) is the only approved drug for ischemic stroke in Canada but is limited in its clinical efficacy due to its short therapeutic window. This study sought to determine the effect of tPA on postnatal primary cortical neuron viability and aimed to identify the relevant cellular signalling mechanisms underlying the tPA-mediated effects in vitro. The data revealed that tPA significantly increased the propensity for cell survival within a time latency window of up to 3 hours. tPA-induced neuroprotective effects were significantly dependent upon the mTOR and JAK/STAT signalling pathways, while the MEK and PKA signalling pathways were found to play a less critical role. Immunocytochemical staining showed a marked increase in p-S6 expression following treatment with tPA, substantiating the vital role of mTOR activation in tPA-mediated neuroprotection. These results suggest the possibility of targeting the defined mechanisms to expand the therapeutic window of tPA in stroke recovery. tPA PROMOTES POSTNATAL CORTICAL NEURON SURVIVAL iii Acknowledgments My sincerest thanks goes to everyone who has helped me along this educational journey. I would like to appreciate my thesis supervisor, Dr. Patrice Smith, as well as the members of my thesis committee, Drs. -
Role of the Prefrontal Cortex in the Neonatal Ventral Hippocampus Lesion, an Animal Model of Schizophrenia
Lu Q, Black SM. J Neurol Neuromed (2016) 1(4): 5-10 Neuromedicine www.jneurology.com www.jneurology.com Journal of Neurology & Neuromedicine Mini Review Open Access Neonatal Hypoxic-Ischemic Brain Injury: Apoptotic and Non- Apoptotic Cell Death Qing Lu, Stephen M. Black Department of Medicine, University of Arizona, AZ USA ABSTRACT Article Info Article Notes The neuronal cell death associated with perinatal asphyxia, or hypoxic- Received: June 04, 2016 ischemic (HI) brain injury, plays an important role in neonatal mortality and Accepted: July 05, 2016 neurodevelopment retardation. The types of cell death associated with HI in the brain have been classified as being either apoptotic or necrotic. Here *Correspondence: we describe the recent discoveries of multiple non-apoptotic cell death Dr. Stephen M Black, PhD Division of Translational and Regenerative Medicine, pathways: necroptosis; ferroptosis; and autosis (autophagy). These new cell Department of Medicine, death pathways expand our understanding of the mechanisms underlying the The University of Arizona, Tucson, AZ, 85719, USA cell death associated with perinatal asphyxia. By targeting specific regulators Email: [email protected] of these pathways, new therapies may be developed that could protect the neonatal brain from the HI mediated injury. © 2016 Black SM. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License Introduction The neuronal cell death associated with neonatal hypoxic- ischemic (HI) brain injury is one of the major causes of neonatal mortality and neurodevelopment retardation. The mortality of and lifelong disabilities, such as cerebral palsy, seizures, visual impairment,HI brain injury mental is retardation,30-40%. -
Interrogating the Relevance of Mitochondrial Apoptosis for Vertebrate Development and Postnatal Tissue Homeostasis
Downloaded from genesdev.cshlp.org on September 28, 2021 - Published by Cold Spring Harbor Laboratory Press REVIEW Interrogating the relevance of mitochondrial apoptosis for vertebrate development and postnatal tissue homeostasis Selma Tuzlak,1 Thomas Kaufmann,2 and Andreas Villunger1,3 1Division of Developmental Immunology, Biocenter, Medical University Innsbruck, A6020 Innsbruck, Austria; 2Institute of Pharmacology, University of Bern, Inselspital, CH3010 Bern, Switzerland; 3Tyrolean Cancer Research Institute, A6020 Innsbruck, Austria “Programmed cell death or ‘apoptosis’ is critical for organ- 1986). After realizing that the presumed oncogenic poten- ogenesis during embryonic development and tissue ho- tial of this gene lies within its anti-apoptotic property meostasis in the adult. Its deregulation can contribute (Vaux et al. 1988), a number of related proteins were iden- to a broad range of human pathologies, including neurode- tified in protein–protein interaction screens, by sequence generation, cancer, or autoimmunity…” These or similar similarity, and/or by structural homology in humans as phrases have become generic opening statements in many well as different vertebrate model organisms and viral reviews and textbooks describing the physiological rele- pathogens. Some of these proteins exert inherent prosur- vance of apoptotic cell death. However, while the role in vival function by blocking apoptosis, and some of them disease has been documented beyond doubt, facilitating may even be converted into killers by limited proteolysis innovative drug discovery, we wonder whether the former or upon alternative splicing of the encoding RNA or act ex- is really true. What goes wrong in vertebrate development clusively as inducers of cell death (Tait and Green 2013; or in adult tissue when the main route to apoptotic cell Czabotar et al. -

Modulation of Apoptosis in Acute Ischemic Stroke As Treatment Challenges
Current Immunology Reviews, 2012, 8, 39-49 39 Modulation of Apoptosis in Acute Ischemic Stroke as Treatment Challenges Joaquin Jordan1, Laura Moreno-Parrado1,2, David Anton-Martinez1,3, Kurt A. Jellinger4 and Maria F. Galindo*,5 1Grupo de Neurofarmacología, Dpto Ciencias Médicas, Fac de Medicina, Universidad de Castilla La Mancha, Avenida Almansa, 14, Albacete 02006, Spain 2Sección de Microbiologia, Complejo Hospitalario Universitario de Albacete, Albacete, Spain 3Sección de Bioquímica, Complejo Hospitalario Universitario de Albacete, Albacete, Spain 4Institute of Clinical Neurobiology, Kenyongasse 18; A-1070 Vienna, Austria 5Unidad de Neuropsicofarmacología Translacional, Complejo Hospitalario Universitario de Albacete, Albacete, Spain Abstract: Stroke is a major cause of death and disability throughout the world. Its pathophysiology is complex and includes excitotoxity, inflammatory pathways, oxidative damage, ionic imbalances, apoptosis and other cell death mechanisms, angiogenesis, and neuroprotection. The ultimate result of the complex ischemic cascade is neuronal death with irreversible loss of neuronal functions. New developments in stroke pathophysiology have induced significant advances in acute stroke management. Among the extracellular signals, inflammation, microglia and cytokines as major consequences of hypoxia may be targets for future therapies. Among the intracellular signals, calcium-induced cell death and oxidative stress as most important factors of ischemic cell death and for dysfunctions of the blood-brain barrier -

Phd Dissertation-Aparna Raghavan
A Dissertation entitled Neuroprotective Potential of Withania Somnifera in Cerebral Ischemia by Aparna Raghavan Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Doctor of Philosophy Degree in Medicinal Chemistry Dr. Zahoor Shah, Committee Chair Dr. Hermann von Grafenstein, Committee Member Dr. James T. Slama, Committee Member Dr. Youssef Sari, Committee Member Dr. Patricia R. Komuniecki, Dean College of Graduate Studies The University of Toledo December 2014 Copyright 2014, Aparna Raghavan This document is copyrighted material. Under copyright law, no parts of this document may be reproduced without the expressed permission of the author. An Abstract of Neuroprotective Potential of Withania Somnifera in Cerebral Ischemia by Aparna Raghavan Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Doctor of Philosophy Degree in Medicinal Chemistry The University of Toledo December 2014 Withania somnifera (WS), popularly known as ‘Ashwagandha’ has been used for centuries in the treatment of neurological disorders, although its effects on cerebral ischemia are not well understood. We used a combination of in vitro and in vivo methods to examine the neuroprotective properties of an aqueous extract of WS in cerebral ischemia. In a mouse model of permanent middle cerebral artery occlusion (pMCAO), WS (200mg/kg) improved functional recovery and significantly reduced the infarct volume in both pre-treatment and post-treatment paradigms. Upon investigating the protective mechanism/s induced by WS, we found that it upregulated the expression of hemeoxygenase 1 (HO1) and attenuated the expression of the pro-apoptotic proteins poly(ADP-ribose) polymerase-1 (PARP-1) and apoptosis inducing factor (AIF), via the PARP-1-AIF pathway. -

Apoptosis-Inducing Factor Is a Major Contributor to Neuronal Loss Induced by Neonatal Cerebral Hypoxia-Ischemia
Cell Death and Differentiation (2007) 14, 775–784 & 2007 Nature Publishing Group All rights reserved 1350-9047/07 $30.00 www.nature.com/cdd Apoptosis-inducing factor is a major contributor to neuronal loss induced by neonatal cerebral hypoxia-ischemia C Zhu1,2, X Wang1,2, Z Huang1,2, L Qiu1,2,FXu1,2, N Vahsen3, M Nilsson1, PS Eriksson1, H Hagberg1,4, C Culmsee5, N Plesnila6, G Kroemer3 and K Blomgren1,7 Nine-day-old harlequin (Hq) mice carrying the hypomorphic apoptosis-inducing factor (AIF)Hq mutation expressed 60% less AIF, 18% less respiratory chain complex I and 30% less catalase than their wild-type (Wt) littermates. Compared with Wt, the infarct volume after hypoxia-ischemia (HI) was reduced by 53 and 43% in male (YXHq) and female (XHqXHq) mice, respectively (Po0.001). The Hq mutation did not inhibit HI-induced mitochondrial release of cytochrome c or activation of calpain and caspase-3. The broad-spectrum caspase inhibitor quinoline-Val-Asp(OMe)-CH2-PH (Q-VD-OPh) decreased the activation of all detectable caspases after HI, both in Wt and Hq mice. Q-VD-OPh reduced the infarct volume equally in Hq and in Wt mice, and the combination of Hq mutation and Q-VD-OPh treatment showed an additive neuroprotective effect. Oxidative stress leading to nitrosylation and lipid peroxidation was more pronounced in ischemic brain areas from Hq than Wt mice. The antioxidant edaravone decreased oxidative stress in damaged brains, more pronounced in the Hq mice, and further reduced brain injury in Hq but not in Wt mice. -

Death and Survival of Cardiomyocytes in Acute Ischemia
REVIEW ISSN 1738-5520 Korean Circulation J 2006;36:165-177 ⓒ 2006, The Korean Society of Circulation Death and Survival of Cardiomyocytes in Acute Ischemia Soo-Hoon Lee, MD1 and Young-Dae Kim, MD2 1Department of Internal Medicine, Ulsan Hospital, Ulsan and 2Department of Internal Medicine, Dong-A University School of Medicine, Cardiovascular Research Institute, Busan, Korea ABSTRACT Ischemia is the most common and important cause of injury to cardiomyocytes. Acute ischemia causes profound derangement of the cellular energetics and metabolism, and this ultimately leads to cell death. Experimental studies have demonstrated the presence of an endogenous protective mechanism that can diminish or delay cell death from ischemic insult; this is known as ischemic preconditioning. In this review, we summarize the recent knowledge of the cellular biology of acute ischemic injury and also signaling mechanisms of cardioprotection that are involved in preconditioning. Further, we briefly discuss the clinical implications. (Korean Circulation J 2006;36:165-177) KEY WORDS:Ischemia;Myocytes, cardiac;Cell death;Ischemic preconditioning. Introduction myocytes, which can promote the survival of cells under ischemic conditions. This review will not cover reper- Ischemia is by far the commonest form of injury fusion injury per se. inflicted upon the myocardium. The clinical presenta- tion of myocardial ischemia encompasses a broad spec- Cellular Injury in Acute Ischemic Stress trum of anginal syndromes, myocardial infarction and congestive heart failure. Because of the widespread and The mammalian heart is an obligatory aerobic organ; increasing prevalence of coronary atherosclerosis, isch- it consumes more oxygen per minute than any other emic heart disease is currently the single most impor- organ in the body.3) It cannot produce enough energy tant identifiable cause of cardiovascular morbidity and under anaerobic condition to maintain its essential mortality throughout the world.1) cellular processes. -

Mitochondria, Oxidative Metabolism and Cell Death in Stroke
Biochimica et Biophysica Acta 1802 (2010) 80–91 Contents lists available at ScienceDirect Biochimica et Biophysica Acta journal homepage: www.elsevier.com/locate/bbadis Review Mitochondria, oxidative metabolism and cell death in stroke Neil R. Sims ⁎, Hakan Muyderman Centre for Neuroscience and Discipline of Medical Biochemistry, Flinders Medical Science and Technology, School of Medicine, Flinders University, Adelaide, South Australia, Australia article info abstract Article history: Stroke most commonly results from occlusion of a major artery in the brain and typically leads to the death Received 19 July 2009 of all cells within the affected tissue. Mitochondria are centrally involved in the development of this tissue Received in revised form 28 August 2009 injury due to modifications of their major role in supplying ATP and to changes in their properties that can Accepted 8 September 2009 contribute to the development of apoptotic and necrotic cell death. In animal models of stroke, the limited Available online 12 September 2009 availability of glucose and oxygen directly impairs oxidative metabolism in severely ischemic regions of the affected tissue and leads to rapid changes in ATP and other energy-related metabolites. In the less-severely Keywords: “ ” Mitochondria ischemic penumbral tissue, more moderate alterations develop in these metabolites, associated with near Stroke normal glucose use but impaired oxidative metabolism. This tissue remains potentially salvageable for at Focal ischemia least the first few hours following stroke onset. Early restoration of blood flow can result in substantial Energy metabolism recovery of energy-related metabolites throughout the affected tissue. However, glucose oxidation is Necrosis markedly decreased due both to lower energy requirements in the post-ischemic tissue and limitations on Apoptosis the mitochondrial oxidation of pyruvate. -

Mechanism of Carbamathione As a Therapeutic Agent For
MECHANISM OF CARBAMATHIONE AS A THERAPEUTIC AGENT FOR STROKE by Jigar Modi A Dissertation Submitted to the Faculty of The Charles E. Schmidt College of Science In Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy Florida Atlantic University Boca Raton, FL December 2017 Copyright by Jigar Modi 2017 ii ACKNOWLEDGEMENTS I want to express my sincerest gratitude to my supervisor, Dr. Jang-Yen Wu, for his great patience, advice, and guidance, as well as giving me extraordinary experiences throughout the work. He provided me unflinching encouragement and support for allowing me the room to work in my own way. Without his mentoring, this dissertation would not have been possible. One simply could not wish for a better or friendlier supervisor. The author wishes to express his sincere thanks and love appreciation to Dr. Jang Yen Wu for his assistance and guidance in preparation of this thesis. Many thanks to my committee members, Dr. Howard Prentice, Dr. Jianning Wei and Dr. Rui Tao, for their contribution on finalizing this thesis. I would like to thank Hongyuan Chou, Dr. Janet Menzie, and Dr. Payam Gharibani for helpfulness on this thesis. At last but not the least, I want to thank my family. My wife Dr. Bhumika Tandel and my sister’s family, Dr. Dipali Mevawala and Dr.Dharmesh Mevawala are always there to encourage and support me. A special thought is devoted to my parents, Nishaben Modi, Pravinchandra Modi and Dr. Binaben Tandel for their unconditional love and endless support. iv ABSTRACT Author: Jigar Modi Title: Mechanism of Carbamathione as a therapeutic agent for Stroke. -

An Antiapoptotic Neuroprotective Role for Neuroglobin
Int. J. Mol. Sci. 2010, 11, 2306-2321; doi:10.3390/ijms11062306 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Review An Antiapoptotic Neuroprotective Role for Neuroglobin Thomas Brittain 1,*, Joanna Skommer 1, Subadhip Raychaudhuri 2 and Nigel Birch 1 1 School of Biological Sciences, University of Auckland, 3 Symonds Street, Auckland, NZ, USA; E-Mails: [email protected] (J.S.); [email protected] (N.B.) 2 Department of Biomedical Engineering, 451 Health Sciences Drive, University of California, Davis, CA, USA; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +64-9-373-75991; Fax: +64-9-373-7414. Received: 10 May 2010; in revised form: 24 May 2010 / Accepted: 24 May 2010 / Published: 27 May 2010 Abstract: Cell death associated with mitochondrial dysfunction is common in acute neurological disorders and in neurodegenerative diseases. Neuronal apoptosis is regulated by multiple proteins, including neuroglobin, a small heme protein of ancient origin. Neuroglobin is found in high concentration in some neurons, and its high expression has been shown to promote survival of neurons in vitro and to protect brain from damage by both stroke and Alzheimer’s disease in vivo. Early studies suggested this protective role might arise from the protein’s capacity to bind oxygen or react with nitric oxide. Recent data, however, suggests that neither of these functions is likely to be of physiological significance. Other studies have shown that neuroglobin reacts very rapidly with cytochrome c released from mitochondria during cell death, thus interfering with the intrinsic pathway of apoptosis. -

The Molecular Intersection Between Axon-Specific Pruning and Neuronal Apoptosis
THE MOLECULAR INTERSECTION BETWEEN AXON-SPECIFIC PRUNING AND NEURONAL APOPTOSIS Corey Leigh Cusack A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Curriculum of Neurobiology Chapel Hill 2014 Approved by: Mohanish Deshmukh Ken D. McCarthy Eva Anton Sally Kornbluth Mark Zylka Robert Nicholas ©2014 Corey Leigh Cusack ALL RIGHTS RESERVED ii ABSTRACT COREY LEIGH CUSACK: The Molecular Intersection between Axon-Specific Pruning and Neuronal Apoptosis (Under the direction of Dr. Mohanish Deshmukh) Neurons can activate pathways to either destroy the whole cell via apoptosis or specifically degenerate only the axon. Axon-specific degeneration, also known as pruning, is required to establish and refine neuronal connections during development and to permit plasticity in the adult nervous system. Aberrant axon degeneration is also observed in several neurodegenerative diseases and can long precede cell body death in neurons. However, despite its biological importance and clinical relevance, the exact mechanism underlying axon degeneration remains unclear. Apoptosis and axon degeneration pathways were widely recognized to be distinct based on the prevalent axotomy-induced model of axon removal called Wallerian degeneration. Five years ago, however, it was discovered that developmental axon pruning induced by axon-specific trophic factor deprivation required the key apoptotic protein Bax as well as a caspase, caspase-6.