The Effect of Altering Brain CYP2B Activity on Nicotine Self-Administration Behaviour and Nicotine Levels in the Brain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

624.Full.Pdf
1521-009X/44/5/624–633$25.00 http://dx.doi.org/10.1124/dmd.115.068932 DRUG METABOLISM AND DISPOSITION Drug Metab Dispos 44:624–633, May 2016 Copyright ª 2016 by The American Society for Pharmacology and Experimental Therapeutics Development of a Rat Plasma and Brain Extracellular Fluid Pharmacokinetic Model for Bupropion and Hydroxybupropion Based on Microdialysis Sampling, and Application to Predict Human Brain Concentrations Thomas I.F.H. Cremers, Gunnar Flik, Joost H.A. Folgering, Hans Rollema, and Robert E. Stratford, Jr. Brains On-Line BV, Groningen, The Netherlands (T.I.F.H.C., G.F. J.H.A.F.); Rollema Biomedical Consulting, Mystic, Connecticut (H.R.); and Division of Pharmaceutical Sciences, Mylan School of Pharmacy, Duquesne University, Pittsburgh, Pennsylvania (R.E.S.) Received December 11, 2015; accepted February 24, 2016 Downloaded from ABSTRACT Administration of bupropion [(6)-2-(tert-butylamino)-1-(3-chlorophenyl) concentration ratio at early time points was observed with propan-1-one] and its preformed active metabolite, hydroxybupropion bupropion; this was modeled as a time-dependent uptake clear- [(6)-1-(3-chlorophenyl)-2-[(1-hydroxy-2-methyl-2-propanyl)amino]- ance of the drug across the blood–brain barrier. Translation of the 1-propanone], to rats with measurement of unbound concentrations model was used to predict bupropion and hydroxybupropion dmd.aspetjournals.org by quantitative microdialysis sampling of plasma and brain extra- exposure in human brain extracellular fluid after twice-daily cellular fluid was used to develop a compartmental pharmacoki- administration of 150 mg bupropion. Predicted concentrations netics model to describe the blood–brain barrier transport of both indicate that preferential inhibition of the dopamine and norepi- substances. -

Monoamine Reuptake Inhibitors in Parkinson's Disease
Hindawi Publishing Corporation Parkinson’s Disease Volume 2015, Article ID 609428, 71 pages http://dx.doi.org/10.1155/2015/609428 Review Article Monoamine Reuptake Inhibitors in Parkinson’s Disease Philippe Huot,1,2,3 Susan H. Fox,1,2 and Jonathan M. Brotchie1 1 Toronto Western Research Institute, Toronto Western Hospital, University Health Network, 399 Bathurst Street, Toronto, ON, Canada M5T 2S8 2Division of Neurology, Movement Disorder Clinic, Toronto Western Hospital, University Health Network, University of Toronto, 399BathurstStreet,Toronto,ON,CanadaM5T2S8 3Department of Pharmacology and Division of Neurology, Faculty of Medicine, UniversitedeMontr´ eal´ and Centre Hospitalier de l’UniversitedeMontr´ eal,´ Montreal,´ QC, Canada Correspondence should be addressed to Jonathan M. Brotchie; [email protected] Received 19 September 2014; Accepted 26 December 2014 Academic Editor: Maral M. Mouradian Copyright © 2015 Philippe Huot et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The motor manifestations of Parkinson’s disease (PD) are secondary to a dopamine deficiency in the striatum. However, the degenerative process in PD is not limited to the dopaminergic system and also affects serotonergic and noradrenergic neurons. Because they can increase monoamine levels throughout the brain, monoamine reuptake inhibitors (MAUIs) represent potential therapeutic agents in PD. However, they are seldom used in clinical practice other than as antidepressants and wake-promoting agents. This review article summarises all of the available literature on use of 50 MAUIs in PD. The compounds are divided according to their relative potency for each of the monoamine transporters. -

Antidepressants, Other Review 04/14/2009
Antidepressants, Other Review 04/14/2009 Copyright © 2004 - 2009 by Provider Synergies, L.L.C. All rights reserved. Printed in the United States of America. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage and retrieval system without the express written consent of Provider Synergies, L.L.C. All requests for permission should be mailed to: Attention: Copyright Administrator Intellectual Property Department Provider Synergies, L.L.C. 5181 Natorp Blvd., Suite 205 Mason, Ohio 45040 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be -

2020 DFS Annual Report
Division of Forensic Science 2020 Annual Report Revised June 29th, 2021 State of Delaware Department of Safety and Homeland Security 200 South Adams Street Wilmington, DE 19801 John Evans, Director Melissa Newell, Deputy Director Dr. Gary Collins, Chief Medical Examiner Jessica Smith, Chief Forensic Toxicologist Amrita Lal-Paterson, DNA Technical Leader Ashley Wang, Forensic Chemistry Unit Leader Johna Esposito, Quality Assurance Manager Table of Contents The Division of Forensic Science ................................................................................................................. 3 Divisional Initiatives, Collaboration, and Information Sharing .................................................................... 4 Overview ................................................................................................................................................... 4 DFSRP- Delaware Forensic Science Reporting System ........................................................................... 5 National Violent Death Reporting System ................................................................................................ 6 Centers for Disease Control Biorepository Program ................................................................................ 6 Delaware Drug Monitoring Initiative........................................................................................................ 7 Disaster Preparation ................................................................................................................................. -

Pharmacokinetic and Pharmacodynamic Interactions Between Antiepileptics and Antidepressants Domenico Italiano University of Messina, Italy
University of Kentucky UKnowledge Psychiatry Faculty Publications Psychiatry 11-2014 Pharmacokinetic and Pharmacodynamic Interactions between Antiepileptics and Antidepressants Domenico Italiano University of Messina, Italy Edoardo Spina University of Messina, Italy Jose de Leon University of Kentucky, [email protected] Right click to open a feedback form in a new tab to let us know how this document benefits oy u. Follow this and additional works at: https://uknowledge.uky.edu/psychiatry_facpub Part of the Psychiatry and Psychology Commons Repository Citation Italiano, Domenico; Spina, Edoardo; and de Leon, Jose, "Pharmacokinetic and Pharmacodynamic Interactions between Antiepileptics and Antidepressants" (2014). Psychiatry Faculty Publications. 40. https://uknowledge.uky.edu/psychiatry_facpub/40 This Article is brought to you for free and open access by the Psychiatry at UKnowledge. It has been accepted for inclusion in Psychiatry Faculty Publications by an authorized administrator of UKnowledge. For more information, please contact [email protected]. Pharmacokinetic and Pharmacodynamic Interactions between Antiepileptics and Antidepressants Notes/Citation Information Published in Expert Opinion on Drug Metabolism & Toxicology, v. 10, Issue 11, p. 1457-1489. © 2014 Taylor & Francis Group This is an Accepted Manuscript of an article published by Taylor & Francis Group in Expert Opinion on Drug Metabolism & Toxicology in Nov. 2014, available online: http://www.tandfonline.com/10.1517/ 17425255.2014.956081 Digital Object Identifier (DOI) http://dx.doi.org/10.1517/17425255.2014.956081 This article is available at UKnowledge: https://uknowledge.uky.edu/psychiatry_facpub/40 1 This is an Accepted Manuscript of an article published by Taylor & Francis Group in Expert Opinion on Drug Metabolism & Toxicology in Nov. -

(12) United States Patent (10) Patent No.: US 7,763,612 B2 Morgan Et Al
USOO7763612B2 (12) United States Patent (10) Patent No.: US 7,763,612 B2 Morgan et al. (45) Date of Patent: Jul. 27, 2010 (54) THERAPEUTIC Bundgaard, Hans, “Novel chemical approaches in prodrug design'. AMINEARYLSULFONAMIDE CONUGATE Drugs of the Future, 1991, p. 443-458, vol. 16(5). COMPOUNDS Cooper, Barrett, R., et al., “Animal Models Used in Prediction of Antidepressant Effects in Man”. J. Clin. Psychiatry, 1983, p. 63-66, vol. 44:5(Sec. 2). (75) Inventors: Philip F. Morgan, Cary, NC (US); Crooks, P. et al., “Synthetic Strategies for the Preparation of James L. Kelley, Raleigh, NC (US) "Gemini” Codrugs of Naltrexone, and Heterocodrugs of &beta Naltrexol with Hydroxybupropion for Transdermal Delivery', 2005 (73) Assignee: Algebra, Inc., Cary, NC (US) AAPS Annual Meeting and Exposition Nov. 5, 2005-Nov. 10, 2005, Abstract. (*) Notice: Subject to any disclaimer, the term of this Folkmann, Michael, et al., “Acyloxymethyl Carbonochloridates. patent is extended or adjusted under 35 New Intermediates in Prodrug Synthesis”. Synthesis, Dec. 1990, p. U.S.C. 154(b) by 852 days. 1159-1166. Greene, Theodora, et al., Protective Groups in Organic Synthesis, (21) Appl. No.: 11/619,291 1991, p. 240. Greene, Theodora, et al., Protective Groups in Organic Synthesis, (22) Filed: Jan. 3, 2007 1991, p. 232. Greene, Theodora, et al., Protective Groups in Organic Synthesis, (65) Prior Publication Data 1991, p. 228. Kelley, James L., et al., “(2S,3S,5R)-2-(3,5-Difluoropenyl)-3,5- US 2007/O155729 A1 Jul. 5, 2007 dimethyl-2-morpholinol: A Novel Antidepressant Agent and Selec tive Inhibitor of Norepinephrine Uptake”. J. -

Bupropion's Bioinequivalence
Bupropion’s Bioinequivalence: Patient Variability, Absorption, and Metabolism by Jamie Nicole Connarn A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Pharmaceutical Sciences) in the University of Michigan 2015 Doctoral Committee: Professor Duxin Sun, Chair Professor Gordon L. Amidon Professor Vicki L. Ellingrod Professor David E. Smith ©Jamie N. Connarn 2015 Dedication To my family for all their love, prayers, and support; especially my Mom. ii Acknowledgements First and foremost, I would like to thank my advisor, Dr. Duxin Sun for all the remarkable opportunities that he gave me during my graduate career as well as the full support and training. Without all his support, knowledge, and dedication to producing successful graduate students, this would not be possible. I would like to thank my committee members; Dr. David Smith, Dr. Gordon Amidon, and Dr. Vicki Ellingrod for all their insightful expertise in guiding my research smoothly. I would also like to thank Dr. Jason Gestwicki, who was a huge help on my Heat Shock Protein studies. In addition, I would like to thank Dr. Rose Feng, Dr. Simon Zhou, and Dr. Yan Li for collaborative projects and all the assistances with my PK analysis. I am grateful for all my lab mates and staff; Hayley Paholak, Joe Burnett, Becky Reed, Xiaoqing Ren, Kanokwan Sansanaphongpricha, Albert Lin, Mari Gasparyan, Alex Yu, Ila Myers, Nathan Truchan, Huixia Luo, Dr. Hongwei Chen, Dr. Ruijuan Luo, Dr. Ting Zhao, Dr. Bo Wen, Dr. Siwei Li, Dr. Xiaoqin Li, Dr. Yasuhiro Tsume, Marisa Gies, and Gail Benninghoff. In addition, I would like to thank those who were a part of our large clinical team; Marisa Kelly, Gloria Harrington, Stephanie Flowers, Kirsten Weiss, Xinyuan (Susie) Zhang, and Andrew Babiskin I would like to express how grateful I am for all of my friends I have met here; Xiaomei Chen, Amy Doty, Morgan Giles, Kelly Hansen, Eric Lachacz, Maya Lipert, Max Mazzara, Allison Maytas, Max Stefan, Charlie Steffens, Arjang Talattof, Karthik Pisupati, Maria Posada, and too many more. -
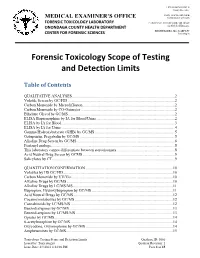
Forensic Toxicology Scope of Testing and Detection Limits
J. RYAN MCMAHON II County Executive INDU GUPTA, MD, MPH MEDICAL EXAMINER’S OFFICE Commissioner of Health FORENSIC TOXICOLOGY LABORATORY CAROLYN H. REVERCOMB, MD, DABP ONONDAGA COUNTY HEALTH DEPARTMENT Chief Medical Examiner KRISTIE BARBA, MS, D-ABFT-FT CENTER FOR FORENSIC SCIENCES Toxicologist Forensic Toxicology Scope of Testing and Detection Limits Table of Contents QUALITATIVE ANALYSES.........................................................................................................2 Volatile Screen by GC/FID .............................................................................................................2 Carbon Monoxide by Microdiffusion..............................................................................................2 Carbon Monoxide by CO-Oximeter ................................................................................................2 Ethylene Glycol by GC/MS.............................................................................................................2 ELISA Buprenorphine by IA for Blood/Urine ................................................................................2 ELISA by IA for Blood ...................................................................................................................3 ELISA by IA for Urine....................................................................................................................4 Gamma Hydroxybutyrate (GHB) by GC/MS..................................................................................5 Gabapentin, -

Pharmacokinetic and Pharmacodynamic of Bupropion: Integrative Overview of Relevant Clinical and Forensic Aspects
Drug Metabolism Reviews ISSN: 0360-2532 (Print) 1097-9883 (Online) Journal homepage: https://www.tandfonline.com/loi/idmr20 Pharmacokinetic and pharmacodynamic of bupropion: integrative overview of relevant clinical and forensic aspects Rafaela Costa, Nuno G. Oliveira & Ricardo Jorge Dinis-Oliveira To cite this article: Rafaela Costa, Nuno G. Oliveira & Ricardo Jorge Dinis-Oliveira (2019): Pharmacokinetic and pharmacodynamic of bupropion: integrative overview of relevant clinical and forensic aspects, Drug Metabolism Reviews, DOI: 10.1080/03602532.2019.1620763 To link to this article: https://doi.org/10.1080/03602532.2019.1620763 Accepted author version posted online: 24 May 2019. Published online: 14 Jun 2019. Submit your article to this journal Article views: 35 View Crossmark data Full Terms & Conditions of access and use can be found at https://www.tandfonline.com/action/journalInformation?journalCode=idmr20 DRUG METABOLISM REVIEWS https://doi.org/10.1080/03602532.2019.1620763 REVIEW ARTICLE Pharmacokinetic and pharmacodynamic of bupropion: integrative overview of relevant clinical and forensic aspects Rafaela Costaa, Nuno G. Oliveirab and Ricardo Jorge Dinis-Oliveiraa,c,d aDepartment of Public Health and Forensic Sciences, and Medical Education, Faculty of Medicine, University of Porto, Porto, Portugal; bResearch Institute for Medicines (iMed.ULisboa), Faculty of Pharmacy, University of Lisbon, Lisbon, Portugal; cUCIBIO, REQUIMTE, Laboratory of Toxicology, Department of Biological Sciences, Faculty of Pharmacy, University of Porto, Porto, Portugal; dIINFACTS – Institute of Research and Advanced Training in Health Sciences and Technologies, Department of Sciences, University Institute of Health Sciences (IUCS), CESPU, CRL, Gandra, Portugal ABSTRACT ARTICLE HISTORY Bupropion is an atypical antidepressant of the aminoketone group, structurally related to cathi- Received 15 February 2019 none, associated with a wide interindividual variability. -

Ronald J. Lukas
CURRICULUM VITAE Ronald J. Lukas Division of Neurobiology Barrow Neurological Institute Ronald J. Lukas 350 West Thomas Road Phoenix, AZ 85013 Phone: 602-406-3399 [email protected] EDUCATION Stanford University School of Medicine postdoctoral 1979-80 Neurobiology University of California, Berkeley postdoctoral 1976-79 Chemical Biodynamics State U. New York Downstate Medical Center Ph.D. 1972-76 Biophysics Columbia University predoctoral 1971-72 Physics State U. New York College at Cortland B.S. 1967-71 Physics RESEARCH/PROFESSIONAL EXPERIENCE 1980-- Staff Scientist/Assistant/Associate Professor (1980-1990), Senior Staff Scientist/Professor (1990-2018), Vice Chairman (1987-1994), Institutional Professor (2019--), Division of Neurobiology; Director (1980-2007)/Co-Director (2008--), Laboratory of Neurochemistry; Barrow Neurological Institute, Phoenix, Arizona 1981-- Research Assistant Professor (1981-1990), Research Associate Professor (1990-1994), Research Professor (1995--), Department of Pharmacology, University of Arizona College of Medicine; Affiliate Faculty (1988-1990), Principal Faculty (1990--), Graduate Program in Neuroscience, University of Arizona;Tucson, Arizona 1989-- Adjunct Professor (1989--), Department of Chemistry and Biochemistry/School of Molecular Science; Member, Arizona State University-Barrow Neurological Institute Program in Neuroscience; Arizona State University, Tempe, Arizona 2007-2018 Vice President-Research, St. Joseph’s Hospital and Medical Center and Barrow Neurological Institute, Phoenix, Arizona 1985-2007 -

Bupropion Wikipedia
13/01/2017 Bupropion Wikipedia Bupropion From Wikipedia, the free encyclopedia Bupropion is a medication primarily used as an antidepressant Bupropion and smoking cessation aid.[6][7][8] It is marketed as Wellbutrin and Zyban among other trade names. It is one of the most frequently prescribed antidepressants in the United States and Canada,[9] although in many countries this is an offlabel use.[10] It is an effective antidepressant on its own, but is also popular as an addon medication in cases of incomplete response to first line SSRI antidepressants.[11] Bupropion is taken in tablet form and is available only by prescription in most countries.[9] The most important side effect is an increase in risk for epileptic seizures, which caused the drug to be withdrawn from the market for some time and then caused the recommended dosage to be reduced.[11] In comparison to many other antidepressants, it does not cause as much weight gain or sexual dysfunction.[11] Bupropion acts as an norepinephrinedopamine reuptake inhibitor (NDRI). It is an atypical antidepressant, different from most commonly prescribed antidepressants such as selective 1 : 1 mixture (racemate) serotonin reuptake inhibitors (SSRIs).[10] Clinical data Pronunciation /bjuːˈproʊ.pi.ɒn/ Bupropion is known to affect several different biological bewᐟᐣᐝᐏpeeon targets.[11][12] It often is described as a norepinephrinedopamine Trade names Wellbutrin, Elontril, Zyban reuptake inhibitor (NDRI), and is also a nicotinic antagonist.[12][13] However, bupropion does not appear to have AHFS/Drugs.com Monograph (https://www.drugs. significant dopaminergic actions in humans under normal com/monograph/bupropionhydr clinical circumstances.[12][14] Chemically, bupropion belongs to ochloride.html) the class of aminoketones and is similar in structure to MedlinePlus a695033 (https://medlineplus.go stimulants such as cathinone and amfepramone, and to v/druginfo/meds/a695033.html) [11] phenethylamines in general. -

Bupropion Inhibits Serotonin Type 3AB Heteromeric Channels at Clinically Relevant Concentrations
1521-0111/97/3/171–179$35.00 https://doi.org/10.1124/mol.119.118349 MOLECULAR PHARMACOLOGY Mol Pharmacol 97:171–179, March 2020 Copyright ª 2020 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. Bupropion Inhibits Serotonin Type 3AB Heteromeric Channels at Clinically Relevant Concentrations Antonia G. Stuebler and Michaela Jansen Department of Cell Physiology and Molecular Biophysics and Center for Membrane Protein Research, School of Medicine, Texas Tech University Health Sciences Center, Lubbock, Texas Received September 25, 2019; accepted December 13, 2019 Downloaded from ABSTRACT Bupropion, a Food and Drug Administration–approved antide- bupropion was reversible and time-dependent. Of note, prein- pressant and smoking cessation aid, blocks dopamine and cubation with a low concentration of bupropion that mimics norepinephrine reuptake transporters and noncompetitively therapeutic drug conditions inhibits 5-HT–induced currents in 5- inhibits nicotinic acetylcholine and serotonin (5-HT) type 3A HT3A and 5-HT3AB receptors considerably. In summary, we receptors (5-HT3ARs). 5-HT3 receptors are pentameric ligand- demonstrate that bupropion inhibits heteromeric 5-HT3ABRs as gated ion channels that regulate synaptic activity in the central well as homomeric 5-HT3ARs. This inhibition occurs at clinically molpharm.aspetjournals.org and peripheral nervous system, presynaptically and postsynap- relevant concentrations and may contribute to bupropion’s tically. In the present study, we examined and compared the clinical effects. effect of bupropion and its active metabolite hydroxybupropion SIGNIFICANCE STATEMENT on mouse homomeric 5-HT3A and heteromeric 5-HT3AB recep- tors expressed in Xenopus laevis oocytes using two-electrode Clinical studies indicate that antagonizing serotonin (5-HT) voltage clamp experiments.