Congestive Heart Failure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

General Signs and Symptoms of Abdominal Diseases
General signs and symptoms of abdominal diseases Dr. Förhécz Zsolt Semmelweis University 3rd Department of Internal Medicine Faculty of Medicine, 3rd Year 2018/2019 1st Semester • For descriptive purposes, the abdomen is divided by imaginary lines crossing at the umbilicus, forming the right upper, right lower, left upper, and left lower quadrants. • Another system divides the abdomen into nine sections. Terms for three of them are commonly used: epigastric, umbilical, and hypogastric, or suprapubic Common or Concerning Symptoms • Indigestion or anorexia • Nausea, vomiting, or hematemesis • Abdominal pain • Dysphagia and/or odynophagia • Change in bowel function • Constipation or diarrhea • Jaundice “How is your appetite?” • Anorexia, nausea, vomiting in many gastrointestinal disorders; and – also in pregnancy, – diabetic ketoacidosis, – adrenal insufficiency, – hypercalcemia, – uremia, – liver disease, – emotional states, – adverse drug reactions – Induced but without nausea in anorexia/ bulimia. • Anorexia is a loss or lack of appetite. • Some patients may not actually vomit but raise esophageal or gastric contents in the absence of nausea or retching, called regurgitation. – in esophageal narrowing from stricture or cancer; also with incompetent gastroesophageal sphincter • Ask about any vomitus or regurgitated material and inspect it yourself if possible!!!! – What color is it? – What does the vomitus smell like? – How much has there been? – Ask specifically if it contains any blood and try to determine how much? • Fecal odor – in small bowel obstruction – or gastrocolic fistula • Gastric juice is clear or mucoid. Small amounts of yellowish or greenish bile are common and have no special significance. • Brownish or blackish vomitus with a “coffee- grounds” appearance suggests blood altered by gastric acid. -

Heart Failure
Heart Failure Sandra Keavey, DHSc, PAC, DFAAPA Defined Heart failure (HF) is a common clinical syndrome resulting from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood. HF may be caused by disease of the myocardium, pericardium, endocardium, heart valves, vessels, or by metabolic disorders Epidemiology-Magnitude Heart failure disproportionately affects the older population. Approximately 80% of all cases of heart failure in the United States occur in persons aged 65 years and older. In the older population, heart failure accounts for more hospital admissions than any other single condition. Following hospitalization for heart failure, nearly half are readmitted within 6 months. Epidemiology-Prevalence Prevalence. About 5.1 million people in the United States have heart failure. One in 9 deaths in 2009 included heart failure as contributing cause. About half of people who develop heart failure die within 5 years of diagnosis. 25% of all heart failure patients are re-admitted to the hospital within 30 days. 50% of all heart failure patients are re-admitted to the hospital within 6 months. Systolic vs Diastolic There are two common types of heart failure Systolic HF Systolic HF is the most common type of HF Now referred to as HFrEF Heart Failure reduced Ejection Fraction The heart is weak and enlarged. The muscle of the left ventricle loses some of its ability to contract or shorten. Diastolic HF Diastolic HF is not an isolated disorder of diastole; there are widespread abnormalities of both systolic and diastolic function that become more apparent with exercise. -

Identifying COPD by Crackle Characteristics
BMJ Open Resp Res: first published as 10.1136/bmjresp-2020-000852 on 5 March 2021. Downloaded from Respiratory epidemiology Inspiratory crackles—early and late— revisited: identifying COPD by crackle characteristics Hasse Melbye ,1 Juan Carlos Aviles Solis,1 Cristina Jácome,2 Hans Pasterkamp3 To cite: Melbye H, Aviles ABSTRACT Key messages Solis JC, Jácome C, et al. Background The significance of pulmonary crackles, Inspiratory crackles— by their timing during inspiration, was described by Nath early and late—revisited: and Capel in 1974, with early crackles associated with What is the key question? identifying COPD by bronchial obstruction and late crackles with restrictive ► In the diagnosis of chronic obstructive pulmonary crackle characteristics. defects. Crackles are also described as ‘fine’ or disease (COPD), is it more useful to focus on the tim- BMJ Open Resp Res ‘coarse’. We aimed to evaluate the usefulness of crackle ing of crackles than on the crackle type? 2021;8:e000852. doi:10.1136/ bmjresp-2020-000852 characteristics in the diagnosis of chronic obstructive What is the bottom line? pulmonary disease (COPD). ► Pulmonary crackles are divided into two types, ‘fine’ Methods In a population-based study, lung sounds Received 2 December 2020 and ‘coarse’ and coarse inspiratory crackles are re- Revised 2 February 2021 were recorded at six auscultation sites and classified in garded to be typical of COPD. In bronchial obstruc- Accepted 5 February 2021 participants aged 40 years or older. Inspiratory crackles tion crackles tend to appear early in inspiration, and were classified as ‘early’ or ‘late and into the types’ this characteristic of the crackle might be easier for ‘coarse’ and ‘fine’ by two observers. -

Age-Related Pulmonary Crackles (Rales) in Asymptomatic Cardiovascular Patients
Age-Related Pulmonary Crackles (Rales) in Asymptomatic Cardiovascular Patients 1 Hajime Kataoka, MD ABSTRACT 2 Osamu Matsuno, MD PURPOSE The presence of age-related pulmonary crackles (rales) might interfere 1Division of Internal Medicine, with a physician’s clinical management of patients with suspected heart failure. Nishida Hospital, Oita, Japan We examined the characteristics of pulmonary crackles among patients with stage A cardiovascular disease (American College of Cardiology/American Heart 2Division of Respiratory Disease, Oita University Hospital, Oita, Japan Association heart failure staging criteria), stratifi ed by decade, because little is known about these issues in such patients at high risk for congestive heart failure who have no structural heart disease or acute heart failure symptoms. METHODS After exclusion of comorbid pulmonary and other critical diseases, 274 participants, in whom the heart was structurally (based on Doppler echocar- diography) and functionally (B-type natriuretic peptide <80 pg/mL) normal and the lung (X-ray evaluation) was normal, were eligible for the analysis. RESULTS There was a signifi cant difference in the prevalence of crackles among patients in the low (45-64 years; n = 97; 11%; 95% CI, 5%-18%), medium (65-79 years; n = 121; 34%; 95% CI, 27%-40%), and high (80-95 years; n = 56; 70%; 95% CI, 58%-82%) age-groups (P <.001). The risk for audible crackles increased approximately threefold every 10 years after 45 years of age. During a mean fol- low-up of 11 ± 2.3 months (n = 255), the short-term (≤3 months) reproducibility of crackles was 87%. The occurrence of cardiopulmonary disease during follow-up included cardiovascular disease in 5 patients and pulmonary disease in 6. -

Assessing and Managing Lung Disease and Sleep Disordered Breathing in Children with Cerebral Palsy Paediatric Respiratory Review
Paediatric Respiratory Reviews 10 (2009) 18–24 Contents lists available at ScienceDirect Paediatric Respiratory Reviews CME Article Assessing and managing lung disease and sleep disordered breathing in children with cerebral palsy Dominic A. Fitzgerald 1,3,*, Jennifer Follett 2, Peter P. Van Asperen 1,3 1 Department of Respiratory Medicine, University of Sydney, Sydney, New South Wales, Australia 2 Department of Physiotherapy, The Children’s Hospital at Westmead, University of Sydney, Sydney, New South Wales, Australia 3 The Children’s Hospital at Westmead Clinical School, Discipline of Paediatrics & Child Health, University of Sydney, Sydney, New South Wales, Australia EDUCATIONAL AIMS To appreciate the insidious evolution of suppurative lung disease in children with cerebral palsy (CP). To be familiar with the management of excessive oral secretions in children with CP. To understand the range of sleep problems that are more commonly seen in children with CP. To gain an understanding of the use of non-invasive respiratory support for the management of airway clearance and sleep disordered breathing in children with CP. ARTICLE INFO SUMMARY Keywords: The major morbidity and mortality associated with cerebral palsy (CP) relates to respiratory compromise. Cerebral palsy This manifests through repeated pulmonary aspiration, airway colonization with pathogenic bacteria, Pulmonary aspiration the evolution of bronchiectasis and sleep disordered breathing. An accurate assessment involving a Suppurative lung disease multidisciplinary approach and relatively simple interventions for these conditions can lead to Physiotherapy significant improvements in the quality of life of children with CP as well as their parents and carers. This Airway clearance techniques Obstructive sleep apnoea review highlights the more common problems and potential therapies with regard to suppurative lung Sleep disordered breathing disease and sleep disordered breathing in children with CP. -
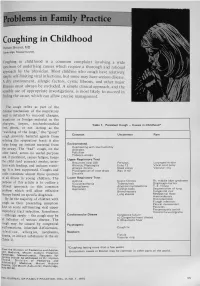
Problems in Family Practice
problems in Family Practice Coughing in Childhood Hyman Sh ran d , M D Cambridge, M assachusetts Coughing in childhood is a common complaint involving a wide spectrum of underlying causes which require a thorough and rational approach by the physician. Most children who cough have relatively simple self-limiting viral infections, but some may have serious disease. A dry environment, allergic factors, cystic fibrosis, and other major illnesses must always be excluded. A simple clinical approach, and the sensible use of appropriate investigations, is most likely to succeed in finding the cause, which can allow precise management. The cough reflex as part of the defense mechanism of the respiratory tract is initiated by mucosal changes, secretions or foreign material in the pharynx, larynx, tracheobronchial Table 1. Persistent Cough — Causes in Childhood* tree, pleura, or ear. Acting as the “watchdog of the lungs,” the “good” cough prevents harmful agents from Common Uncommon Rare entering the respiratory tract; it also helps bring up irritant material from Environmental Overheating with low humidity the airway. The “bad” cough, on the Allergens other hand, serves no useful purpose Pollution Tobacco smoke and, if persistent, causes fatigue, keeps Upper Respiratory Tract the child (and parents) awake, inter Recurrent viral URI Pertussis Laryngeal stridor feres with feeding, and induces vomit Rhinitis, Pharyngitis Echo 12 Vocal cord palsy Allergic rhinitis Nasal polyp Vascular ring ing. It is best suppressed. Coughs and Prolonged use of nose drops Wax in ear colds constitute almost three quarters Sinusitis of all illness in young children. The Lower Respiratory Tract Asthma Cystic fibrosis Rt. -

Medical Terminology Abbreviations Medical Terminology Abbreviations
34 MEDICAL TERMINOLOGY ABBREVIATIONS MEDICAL TERMINOLOGY ABBREVIATIONS The following list contains some of the most common abbreviations found in medical records. Please note that in medical terminology, the capitalization of letters bears significance as to the meaning of certain terms, and is often used to distinguish terms with similar acronyms. @—at A & P—anatomy and physiology ab—abortion abd—abdominal ABG—arterial blood gas a.c.—before meals ac & cl—acetest and clinitest ACLS—advanced cardiac life support AD—right ear ADL—activities of daily living ad lib—as desired adm—admission afeb—afebrile, no fever AFB—acid-fast bacillus AKA—above the knee alb—albumin alt dieb—alternate days (every other day) am—morning AMA—against medical advice amal—amalgam amb—ambulate, walk AMI—acute myocardial infarction amt—amount ANS—automatic nervous system ant—anterior AOx3—alert and oriented to person, time, and place Ap—apical AP—apical pulse approx—approximately aq—aqueous ARDS—acute respiratory distress syndrome AS—left ear ASA—aspirin asap (ASAP)—as soon as possible as tol—as tolerated ATD—admission, transfer, discharge AU—both ears Ax—axillary BE—barium enema bid—twice a day bil, bilateral—both sides BK—below knee BKA—below the knee amputation bl—blood bl wk—blood work BLS—basic life support BM—bowel movement BOW—bag of waters B/P—blood pressure bpm—beats per minute BR—bed rest MEDICAL TERMINOLOGY ABBREVIATIONS 35 BRP—bathroom privileges BS—breath sounds BSI—body substance isolation BSO—bilateral salpingo-oophorectomy BUN—blood, urea, nitrogen -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Signs and Symptoms
Signs and Symptoms Some abnormal heart rhythms can happen without the person knowing it, while some may cause a feeling of the heart “racing,” lightheadedness, or dizziness. At some point in life, many adults Rapid Heartbeat – Tachycardia have had short-lived heart rhythm When the heart beats too quickly changes that are not serious. (usually above 100 beats per minute), the lower chambers, or Certain heart rhythms, especially ventricles, do not have enough time those that last long enough to af - to fill with blood, so they cannot ef - fect the heart’s function, can be fectively pump blood to the rest of serious or even deadly. the body. When this happens, some Palpitation or Skipped Beat people have symptoms such as: Although it may seem as if the Skipping a beat Slow Heartbeat – Bradycardia heart missed a beat, it has really had an early heartbeat — an extra If the heartbeat is too slow (usually Beating out of rhythm below 60 beats per minute), not beat that happens before the heart Palpitations has a chance to fill with blood. enough blood carrying oxygen Fast or racing heartbeat Therefore the squeeze is empty flows through the body. The symptoms of a slow heartbeat are: and results in a pause. Shortness of breath Fatigue (feeling tired) Fluttering Chest pain A fluttering sensation (like butter - Dizziness Dizziness flies in the chest) is usually due to Lightheadedness extra or “skipped beats” that occur Lightheadedness Fainting or near fainting one right after the other, or may be Fainting or near fainting caused by other kinds of abnormal heart rhythms. -

Chest Pain in a Patient with Cystic Fibrosis
Copyright ©ERS Journals Ltd 1998 Eur Respir J 1998; 12: 245–247 European Respiratory Journal DOI: 10.1183/09031936.98.12010245 ISSN 0903 - 1936 Printed in UK - all rights reserved CASE FOR DIAGNOSIS Chest pain in a patient with cystic fibrosis D.P. Dunagan*, S.L. Aquino+, M.S. Schechter**, B.K. Rubin**, J.W. Georgitis** Case history A 38 yr old female with a history of cystic fibrosis (CF) presented to an outside emergency department with dysp- noea and right-sided chest pain of approximately 12 h duration. Her history was significant for recurrent pneu- mothoraces and a recent respiratory exacerbation of CF requiring prolonged antibiotic therapy for Pseudomonas aeruginosa. She described the pain as relatively acute in onset, sharp, increased with deep inspiration, without out- ward radiation, and progressive in intensity. There was no history of travel, worsening cough, fever, chills or increase in her chronic expectoration of blood-streaked sputum. An outside chest radiograph was interpreted as demonstrating a "rounded" right lower lobe pneumonia and she was transferred to our institution for further evaluation. Fig. 2. – Computed tomography scan of the chest. Open arrow: multi- On examination, she was thin, afebrile and in minimal ple cysts; closed white arrow: 3.8×5 cm round mass, respiratory distress. There were decreased breath sounds throughout all lung fields, symmetric chest wall excursion with inspiration and bilateral basilar crackles. Subjective right lateral chest discomfort was reported with deep ins- piratory manoeuvres. The remaining physical examination was normal except for clubbing of the upper extremities. Laboratory data revealed an elevated white blood cell count of 19.2×109 cells·L-1 with a normal differential. -

Arrhythmia What Is It?
Arrhythmia What is it? Most of us have felt our heart race or skip a beat. It’s fairly normal every once and a while. But for some people, it’s a sign of arrhythmia – a disorder of your heart rate or rhythm – that needs to be checked out by a specialist. If you have an arrhythmia (there are multiple types), your heart either beats: • too fast • too slow or • with an irregular pattern Did You Know? This change in your heart rhythm is usually caused by a “glitch” Our heart beats an average of in your heart’s electrical activity, which tells the heart when to 70 to 80 times a minute and contract and pump blood to the body. Your heart doesn’t beat over 100,000 times a day! It’s with the regularity of a Swiss watch, and many factors can cause no wonder millions of people an irregularity. notice palpitations such as skipping a beat, fluttering or a Some of these factors include: racing heart. • having had a heart attack • having heart failure • blood chemistry imbalances • abnormal hormone levels • alcohol, caffeine and other substances or medicines • a variety of inherited abnormalities 8 Tips for Staying Heart Healthy with Arrhythmias Living with an arrhythmia varies tremendously from one person to the next. It will depend on the type of arrhythmia you have, how serious it is and the recommended treatment. Some people can take a single medication to correct their heart’s rhythm; others undergo electrophysiology studies or require a pacemaker or implantable defibrillator. No matter what kind of arrhythmia you have, there are things you can do to keep your heart healthy and ticking as it should. -

Respiratory Failure
Respiratory Failure Phuong Vo, MD,* Virginia S. Kharasch, MD† *Division of Pediatric Pulmonary and Allergy, Boston Medical Center, Boston, MA †Division of Respiratory Diseases, Boston Children’s Hospital, Boston, MA Practice Gap The primary cause of cardiopulmonary arrest in children is unrecognized respiratory failure. Clinicians must recognize respiratory failure in its early stage of presentation and know the appropriate clinical interventions. Objectives After completing this article, readers should be able to: 1. Recognize the clinical parameters of respiratory failure. 2. Describe the respiratory developmental differences between children and adults. 3. List the clinical causes of respiratory failure. 4. Review the pathophysiologic mechanisms of respiratory failure. 5. Evaluate and diagnose respiratory failure. 6. Discuss the various clinical interventions for respiratory failure. WHAT IS RESPIRATORY FAILURE? Respiratory failure is a condition in which the respiratory system fails in oxy- genation or carbon dioxide elimination or both. There are 2 types of impaired gas exchange: (1) hypoxemic respiratory failure, which is a result of lung failure, and (2) hypercapnic respiratory failure, which is a result of respiratory pump failure (Figure 1). (1)(2) In hypoxemic respiratory failure, ventilation-perfusion (V_ =Q)_ mismatch results in the decrease of PaO2) to below 60 mm Hg with normal or low PaCO2. _ = _ (1) In hypercapnic respiratory failure, V Q mismatch results in the increase of AUTHOR DISCLOSURE Drs Vo and Kharasch fi PaCO2 to above 50 mm Hg. Either hypoxemic or hypercapnic respiratory failure have disclosed no nancial relationships can be acute or chronic. Acute respiratory failure develops in minutes to hours, relevant to this article.