Left Flank Pain As the Sole Manifestation of Acute Pancreatitis: a Report of a Case with an Initial Misdiagnosis Emerg Med J: First Published As on 23 May 2005
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

General Signs and Symptoms of Abdominal Diseases
General signs and symptoms of abdominal diseases Dr. Förhécz Zsolt Semmelweis University 3rd Department of Internal Medicine Faculty of Medicine, 3rd Year 2018/2019 1st Semester • For descriptive purposes, the abdomen is divided by imaginary lines crossing at the umbilicus, forming the right upper, right lower, left upper, and left lower quadrants. • Another system divides the abdomen into nine sections. Terms for three of them are commonly used: epigastric, umbilical, and hypogastric, or suprapubic Common or Concerning Symptoms • Indigestion or anorexia • Nausea, vomiting, or hematemesis • Abdominal pain • Dysphagia and/or odynophagia • Change in bowel function • Constipation or diarrhea • Jaundice “How is your appetite?” • Anorexia, nausea, vomiting in many gastrointestinal disorders; and – also in pregnancy, – diabetic ketoacidosis, – adrenal insufficiency, – hypercalcemia, – uremia, – liver disease, – emotional states, – adverse drug reactions – Induced but without nausea in anorexia/ bulimia. • Anorexia is a loss or lack of appetite. • Some patients may not actually vomit but raise esophageal or gastric contents in the absence of nausea or retching, called regurgitation. – in esophageal narrowing from stricture or cancer; also with incompetent gastroesophageal sphincter • Ask about any vomitus or regurgitated material and inspect it yourself if possible!!!! – What color is it? – What does the vomitus smell like? – How much has there been? – Ask specifically if it contains any blood and try to determine how much? • Fecal odor – in small bowel obstruction – or gastrocolic fistula • Gastric juice is clear or mucoid. Small amounts of yellowish or greenish bile are common and have no special significance. • Brownish or blackish vomitus with a “coffee- grounds” appearance suggests blood altered by gastric acid. -

WHO Guidance on Management of Snakebites
GUIDELINES FOR THE MANAGEMENT OF SNAKEBITES 2nd Edition GUIDELINES FOR THE MANAGEMENT OF SNAKEBITES 2nd Edition 1. 2. 3. 4. ISBN 978-92-9022- © World Health Organization 2016 2nd Edition All rights reserved. Requests for publications, or for permission to reproduce or translate WHO publications, whether for sale or for noncommercial distribution, can be obtained from Publishing and Sales, World Health Organization, Regional Office for South-East Asia, Indraprastha Estate, Mahatma Gandhi Marg, New Delhi-110 002, India (fax: +91-11-23370197; e-mail: publications@ searo.who.int). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use. -

Grey Turner's and Cullen's Signs Induced by Spontaneous Hemorrhage of the Abdominal Wall After Coughing
CASE REPORT pISSN 2288-6575 • eISSN 2288-6796 https://doi.org/10.4174/astr.2017.93.2.115 Annals of Surgical Treatment and Research Grey Turner’s and Cullen’s signs induced by spontaneous hemorrhage of the abdominal wall after coughing Zhe Fan, Yingyi Zhang Department of General Surgery, The Third People’s Hospital of Dalian, Dalian Medical University, Dalian, China Grey Turner’s and Cullen’s signs are rare clinical signs, which most appear in patients with severe acute pancreatitis. The present patient complained of abdominal pain after coughing. However, contrast-enhanced CT revealed a hemorrhage of the abdominal wall. Therefore, spontaneous hemorrhage of the abdominal wall was diagnosed. The patient recovered through immobilization and hemostasis therapy. This case report and literature review aims to remind clinicians of manifestations and treatment of spontaneous hemorrhage. [Ann Surg Treat Res 2017;93(2):115-117] Key Words: Grey Turner’s sign, Cullen’s sign, Spontaneous hemorrhage INTRODUCTION right thigh were noted (Fig. 2). All of the laboratory tests were normal, except that hemoglobin was decreased to 10.5 Grey Turner’s and Cullen’s signs generally suggest a large g/L. Contrastenhanced CT of the abdomen revealed a huge retroperitoneal hematoma, such as hemorrhagic pancreatitis. hematoma in the right lateral abdominal wall (Fig. 3). Therefore, The current case was unusual because of a spontaneous hemo Grey Turner’s and Cullen’s signs induced by spontaneous rrhage of the abdominal wall after coughing leading to Grey hemorrhage of the abdominal wall after cough were diagnosed. Turner’s and Cullen’s signs. -

The Flank Incision and Exposure of the Kidney 2
THE FLANK INCISION AND EXPOSURE OF THE KIDNEY 2 Good flank exposure of the kid- perpendicular to the operating ney can be achieved by many sur- table and thus allows the operat- gical approaches. In general, the ing table to be rolled from side to kidney lies higher than expected side for improved exposure of the from the radiologic studies, with anterior or posterior kidney. the left kidney slightly higher Although the anterior superior than the right kidney. Except for iliac spine is positioned at the flex- lower pole renal biopsy, most op- ion of the table, when the table is erations require good exposure of fully flexed, the final position of the renal pelvis and the renal the body will cause the entire pedicle and thus call for either a pelvis to be slightly below the supra–twelfth-rib incision or a apex of the flexion and the ribs to twelfth-rib rib resection. In the fol- be slightly above, which creates lowing discussion of these two tension in the area of the lower approaches, important anatomic considerations for all flank expo- Flank Position sures are highlighted. FIG. 2-1. The flexion of the oper- Tension placed on Anterior Superior iliac spine ating table should be in line with ribs and skin in line with flexion of table the anterior superior iliac spine of the pelvis. This spine is a constant landmark that the surgeon can palpate in both thin and obese patients. After the patient is positioned on the side, the kidney rest can be elevated and the operating table flexed. -

Retroperitoneal Hemorrhage – a Review of the Eponymous Cutaneous Signs
Journal of Pakistan Association of Dermatologists. 2020; 30(3): 501-506. Review Article Retroperitoneal hemorrhage – A review of the eponymous cutaneous signs Sajad Ahmad Salati Department of Surgery, Unaizah College of Medicine, Qassim University, Saudi Arabia. Abstract Physical diagnosis by eliciting clinical signs still plays an important role in the management of diseases .In case of retroperitoneal bleeding due to any cause, there are five important eponymous cutaneous signs mentioned in literature. These include Cullen’s sign, Turner’s sign, Fox’s sign, Bryant’s sign and Stabler’s sign. These signs are briefly reviewed in this article. Key words Retroperitoneal hemorrhage, Cullen’s sign, Turner’s sign, Fox’s sign, Bryant’s sign, Stabler’s sign. Introduction Web of Science, Semantic Scholar and Reseachgate after search on keywords: In recent years, there have been revolutionary retroperitoneal hemorrhage, skin sign, advances in imaging and diagnostic facilities. eponymous sign and diagnostic sign. The search But in spite of these changes, there are certain was extended across to the cross references. time tested objective physical findings that Only the articles published in English were retain their relevance and importance in eliciting included and no time limits were set. diagnosis or in narrowing the differential diagnosis. The eponymous cutaneous signs of Clinical presentation retroperitoneal hemorrhage are such clinical signs which aid in diagnosis and management of 1. Cullen's sign (Figure 1A) denotes patients besides highlighting the rich history of ecchymosis around the umbilical area as seen dermatology. These eponyms are based on the after retroperitoneal hemorrhage . This sign is physician who first described the clinical accredited to Thomas Stephen Cullen (1868- findings. -

Abdominal Pain
10 Abdominal Pain Adrian Miranda Acute abdominal pain is usually a self-limiting, benign condition that irritation, and lateralizes to one of four quadrants. Because of the is commonly caused by gastroenteritis, constipation, or a viral illness. relative localization of the noxious stimulation to the underlying The challenge is to identify children who require immediate evaluation peritoneum and the more anatomically specific and unilateral inner- for potentially life-threatening conditions. Chronic abdominal pain is vation (peripheral-nonautonomic nerves) of the peritoneum, it is also a common complaint in pediatric practices, as it comprises 2-4% usually easier to identify the precise anatomic location that is produc- of pediatric visits. At least 20% of children seek attention for chronic ing parietal pain (Fig. 10.2). abdominal pain by the age of 15 years. Up to 28% of children complain of abdominal pain at least once per week and only 2% seek medical ACUTE ABDOMINAL PAIN attention. The primary care physician, pediatrician, emergency physi- cian, and surgeon must be able to distinguish serious and potentially The clinician evaluating the child with abdominal pain of acute onset life-threatening diseases from more benign problems (Table 10.1). must decide quickly whether the child has a “surgical abdomen” (a Abdominal pain may be a single acute event (Tables 10.2 and 10.3), a serious medical problem necessitating treatment and admission to the recurring acute problem (as in abdominal migraine), or a chronic hospital) or a process that can be managed on an outpatient basis. problem (Table 10.4). The differential diagnosis is lengthy, differs from Even though surgical diagnoses are fewer than 10% of all causes of that in adults, and varies by age group. -

Left Flank Pain As the Sole Manifestation of Acute Pancreatitis
452 CASE REPORTS Emerg Med J: first published as 10.1136/emj.2003.013847 on 23 May 2005. Downloaded from Left flank pain as the sole manifestation of acute pancreatitis: a report of a case with an initial misdiagnosis J-H Chen, C-H Chern, J-D Chen, C-K How, L-M Wang, C-H Lee ............................................................................................................................... Emerg Med J 2005;22:452–453 On further review of the patient’s case 2 hours after the Acute pancreatitis is not an uncommon disease in an ultrasound examination, a decision was made to obtain a emergency department (ED). It manifests as upper abdominal computed tomography (CT) scan due to concern over the pain, sometimes with radiation of pain to the back and flank limitation of ultrasound studies in some clinical conditions. region. Isolated left flank pain being the sole manifestation of The CT showed abnormal fluid collection over the peri-renal acute pancreatitis is very rare and not previously identified in space and pancreatic tail as well as necrotic changes and the literature. In this report, we present a case of acute swelling of the pancreatic tail (fig 1). Serum pancreatic pancreatitis presenting solely with left flank pain. Having enzymes revealed a normal amylase (90 u/L) and a slightly negative findings on an ultrasound initially, she was elevated lipase level (336 u/L). The patient was diagnosed to misdiagnosed as having possible ‘‘acute pyelonephritis or have acute pancreatitis and admitted for supportive treat- other renal diseases’’. A second radiographic evaluation ment and monitoring. During her admission she was also with computed tomography showed pancreatitis in the tail noted to have hyperlipidemia (triglyceride 980 mg/dL and with abnormal fluid collected extending to the left peri-renal cholesterol 319 mg/dL). -

Natural History of Oregon Coast Mammals Chris Maser Bruce R
Forest Servile United States Depa~ment of the interior Bureau of Land Management General Technical Report PNW-133 September 1981 ser is a ~ildiife biologist, U.S. ~epa~rn e Interior, Bureau of La gement (stationed at Sciences Laboratory, Corvallis, Oregon. Science Center, ~ewpo Sciences Laborato~, Corvallis, Oregon. T. se is a soil scientist, U.S. wa t of culture, Forest Service, Pacific rthwest Forest and ange ~xperim Station, lnst~tute of orthern Forestry, Fairbanks, Alaska. Natural History of Oregon Coast Mammals Chris Maser Bruce R. Mate Jerry F. Franklin C. T. Dyrness Pacific Northwest Forest and Range Experiment Station U.S. Department of Agriculture Forest Service General Technical Report PNW-133 September 1981 Published in cooperation with the Bureau of Land Management U.S. Department of the Interior Abstract Maser, Chris, Bruce R. Mate, Jerry F. Franklin, and C. T. Dyrness. 1981. Natural history of Oregon coast mammals. USDA For. Serv. Gen. Tech. Rep. PNW-133, 496 p. Pac. Northwest For. and Range Exp. Stn., Portland, Oreg. The book presents detailed information on the biology, habitats, and life histories of the 96 species of mammals of the Oregon coast. Soils, geology, and vegetation are described and related to wildlife habitats for the 65 terrestrial and 31 marine species. The book is not simply an identification guide to the Oregon coast mammals but is a dynamic portrayal of their habits and habitats. Life histories are based on fieldwork and available literature. An extensive bibliography is included. Personal anecdotes of the authors provide entertaining reading. The book should be of use to students, educators, land-use planners, resource managers, wildlife biologists, and naturalists. -

ACR Appropriateness Criteria: Suspected Retroperitoneal Bleed
New 2021 American College of Radiology ACR Appropriateness Criteria® Suspected Retroperitoneal Bleed Variant 1: Clinically suspected retroperitoneal bleed. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CT abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢ CT abdomen and pelvis without and with IV Usually Appropriate contrast ☢☢☢☢ CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢☢ Aortography abdomen and pelvis May Be Appropriate (Disagreement) ☢☢☢☢ CT abdomen and pelvis without IV contrast May Be Appropriate ☢☢☢ US abdomen and pelvis Usually Not Appropriate O Radiography abdomen and pelvis Usually Not Appropriate ☢☢☢ MRA abdomen and pelvis with IV contrast Usually Not Appropriate O MRA abdomen and pelvis without and with Usually Not Appropriate IV contrast O MRA abdomen and pelvis without IV contrast Usually Not Appropriate O MRI abdomen and pelvis without and with IV Usually Not Appropriate contrast O MRI abdomen and pelvis without IV contrast Usually Not Appropriate O RBC scan abdomen and pelvis Usually Not Appropriate ☢☢☢ ACR Appropriateness Criteria® 1 Suspected Retroperitoneal Bleed SUSPECTED RETROPERITONEAL BLEED Expert Panel on Vascular Imaging: Nupur Verma, MDa; Michael L. Steigner, MDb; Ayaz Aghayev, MDc; Ezana M. Azene, MD, PhDd; Suzanne T. Chong, MD, MSe; Benoit Desjardins, MD, PhDf; Riham H. El Khouli, MD, PhDg; Nicholas E. Harrison, MDh; Sandeep S. Hedgire, MDi; Sanjeeva P. Kalva, MDj; Yoo Jin Lee, MDk; David M. Mauro, MDl; Hiren J. Mehta, MDm; Mark Meissner, MDn; Anil K. Pillai, MDo; Nimarta Singh, MD, MPHp; Pal S. Suranyi, MD, PhDq; Eric E. Williamson, MDr; Karin E. Dill, MD.s Summary of Literature Review Introduction/Background Retroperitoneal bleeding is a hemorrhage into the retroperitoneal space, the space located posterior to the parietal peritoneum and anterior to the transversalis fascia. -
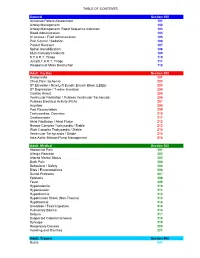
UNC Aircare Protocol Manuel
TABLE OF CONTENTS General Section 100 Universal Patient Assessment 101 Airway Management 102 Airway Management: Rapid Sequence Induction 103 Blood Administration 104 IV Access / Fluid Administration 105 Pain Control / Sedation 106 Patient Restraint 107 Spinal Immobilization 108 Multi-Casualty Incidents 109 S.T.A.R.T. Triage 110 JumpS.T.A.R.T. Triage 111 Weapons of Mass Destruction 112 Adult: Cardiac Section 200 Bradycardia 201 Chest Pain: Ischemia 202 ST Elevation / New Left Bundle Branch Block (LBBB) 203 ST Depression / T-wave Inversion 204 Cardiac Arrest 205 Ventricular Fibrillation / Pulsless Ventricular Tacharcida 206 Pulsless Electrical Activity (PEA) 207 Asystole 208 Post Resuscitation 209 Tachycardias: Overview 210 Cardioversion 211 Atrial Fibrillation / Atrial Flutter 212 Narrow Complex Tachycardia / Stable 213 Wide Complex Tachycardia / Stable 214 Ventricular Tachycardia / Stable 215 Intra-Aortic Balloon Pump Management 216 Adult: Medical Section 300 Abdominal Pain 301 Allergic Reaction 302 Altered Mental Status 303 Back Pain 304 Behavioral / Safety 305 Bites / Envenomations 306 Dental Problems 307 Epistaxis 308 Fever 309 Hyperkalemia 310 Hypertension 311 Hyperthermia 312 Hypotension Shock (Non-Trauma) 313 Hypothermia 314 Overdose / Toxic Ingestion 315 Pulmonary Edema 316 Seizure 317 Suspected Ceberal Ischemia 318 Syncope 319 Respiratory Distress 320 Vomiting and Diarrhea 321 Adult: Trauma Section 400 Burns 401 TABLE OF CONTENTS Drowning / Near Drowning 402 Electrical Injuries 403 Extremity Trauma 404 Head Trauma / Traumatic -
Snakebite Treatment Protocol
TREATMENT PROTOCOL IN VENOMOUS SNAKEBITE A venomous snakebite is diagnosed from the symptoms suggestive of systemic envenomation. Haemostatic abnormalities are prima facie evidence of viperidae bite. All viperidae bites can cause renal failure. Neurotoxic symptoms like ptosis can also be seen in a Russels viper bite. SIGNS & SYMPTOMS SUGGESTING A VIPERIDAE BITE- Local pain, swelling and erythema at the bite site. tender enlargement of lymph nodes draining the bitten part this is secondary to larger molecular weight venom fractions entering into the lymphatics local necrosis and or blistering nausea, vomiting, abdominal pain and abdominal tenderness which suggest a gastro-intestinal or retro-peritoneal bleed. hypotension resulting from hypovolemia or direct vasodilatory effects of venom fractions low back ache or loin pain which suggest of the likelihood of developing renal failure or a retroperitoneal bleed passage of reddish or dark brown colored urine or a reduction in the amount of urine output lateralizing neurological signs indicative of an intracranial bleed muscle pain indicating rhabdomyoloysis bilateral parotid enlargement ( viper head appearance ), conjunctival oedema and subconjunctival haemorrhage dysgeusia with a metallic taste confusional state , ptosis jaundice the victims could bleed internally from any organ or mucosal surface.Hemoptysis, epistaxis,hematuria, hematemesis & melena,chemosis, macular bleed, excessive menstrual bleed, bleeding from the bite site or cannula, bleeding into the muscles, gingival -

Chapter 5 – Gastrointestinal System
CHAPTER 5 – GASTROINTESTINAL SYSTEM First Nations and Inuit Health Branch (FNIHB) Clinical Practice Guidelines for Nurses in Primary Care. The content of this chapter was revised October 2011. Table of Contents ASSESSMENT OF THE GASTROINTESTINAL SYSTEM ......................................5–1 EXAMINATION OF THE ABDOMEN ........................................................................5–2 COMMON PROBLEMS OF THE GASTROINTESTINAL SYSTEM .........................5–4 Anal Fissure .......................................................................................................5–4 Constipation .......................................................................................................5–5 Dehydration (Hypovolemia) ...............................................................................5–8 Diarrhea ...........................................................................................................5–11 Diverticular Disease .........................................................................................5–15 Diverticulitis ......................................................................................................5–15 Diverticulosis ....................................................................................................5–16 Dyspepsia ........................................................................................................5–17 Gallbladder Disease .........................................................................................5–18 Biliary Colic ......................................................................................................5–21