ECG Review 2020 Eric Hockstad, MD Medical Director of Cardiac Cath Labs University of Kansas Medical System ECG Basics ECG Basics PR Interval / Segment ECG Basics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The QT Interval: How Long Is Too Long?
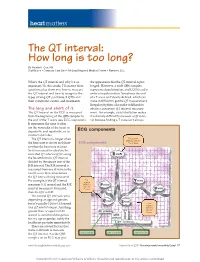
heart matters The QT interval: How long is too long? By Natalie K. Cox, RN Staff Nurse • Coronary Care Unit • McLeod Regional Medical Center • Florence, S.C. What’s the QT interval and why’s it so the appearance that the QT interval is pro- important? In this article, I’ll answer these longed. However, a wide QRS complex questions plus show you how to measure represents depolarization, and LQTS is a dis- the QT interval and how to recognize the order of repolarization. Sometimes the end types of long QT syndrome (LQTS) and of a T wave isn’t clearly defi ned, which can their symptoms, causes, and treatments. make it diffi cult to get the QT measurement. Irregular rhythms also make it diffi cult to The long and short of it obtain a consistent QT interval measure- The QT interval on the ECG is measured ment. For example, atrial fi brillation makes from the beginning of the QRS complex to it extremely diffi cult to measure a QT inter- the end of the T wave (see ECG components). val because fi nding a T wave isn’t always It represents the time it takes for the ventricles of the heart to depolarize and repolarize, or to ECG components contract and relax. The QT interval is longer when First positive deflection after the the heart rate is slower and short- ECG components P or Q wave er when the heart rate is faster. So it’s necessary to calculate the corrected QT interval (QTc) using the Bazett formula: QT interval divided by the square root of the R-R interval. -
Some Observations on the Atrial Sound*
15 Oktober 1960 S.A. TYDSKRIF VIR GENEESKUNDE 887 SOME OBSERVATIONS ON THE ATRIAL SOUND* JOHN R BARLOW, M.R, RCH., M.R.C.P., Department of Medicine, University of The WiTwaTersralld. Johallllesburg The atrial sound, also known as the fourth heart sound Emotional factors probably play a large part in this; the or. presystolic gallop, has been defined' as an audible P-G interval may quickly horten again on the introduction ibration occurring more than 0·07 second after the of an intravenous needle or imilar procedure. beginning of the P wave of the simultaneous electrocardio 3. EffeCT of respiration. Whereas re piration produce gram (ECG) but preceding the onset of the QRS complex. no effect on the P-G interval in patients with hyperten ion It has been shown' that, unrelated to any alteration in the or ischaemia. the atrial sound of cor pulmonale both in P-R interval, the position of the atrial sound varies in creases in intensity and occurs earlier in the cardiac cycle relation to the first heart sound and to the simultaneous during inspiration as compared with expiration (Fig. 4). ECG. 4. EffeCT of various procedures. Jt has already been Jt is the purpose of this paper to demonstrate this mentioned that the intravenous administration of hypo variation in the timing of the atrial sound and to discuss tensive drugs will increase the P-G interval in hypertensive some of the clinical implications resulting from this varia patients. The inhalation of amyl nitrite has a similar effect bility. in hypertension (Fig. 5), though a change in the P-G METHODS AND OBSERVATIO S interval is seldom seen in cases with ischaemic heart disease following inhalation of this drug. -

Chronotropic and Dromotropic Responses to Localized Glutamate Microinjections in the Rat $ Nucleus Ambiguus
brain research 1542 (2014) 93–103 Available online at www.sciencedirect.com www.elsevier.com/locate/brainres Research Report Chronotropic and dromotropic responses to localized glutamate microinjections in the rat $ nucleus ambiguus Karla N. Sampaio1,He´lder Mauad2, K. Michael Spyer, Timothy W. Fordn Division of Biosciences, Faculty of Life Sciences, University College London, Gower Street, London WC1E 6BT, UK article info abstract Article history: The cardioinhibitory effects of cardiac vagal motoneurons (CVMs) are mediated by Accepted 18 October 2013 activation of postganglionic neurons in the epicardial ganglia which have been shown to Available online 24 October 2013 exert functionally selective effects on heart rate and atrioventricular conduction in the rat. Here we investigate whether CVMs producing these responses may occupy different Keywords: rostrocaudal positions within the nucleus ambiguus. Excitation of CVMs was attempted Autonomic nervous system by microinjections of glutamate into the nucleus ambiguus of an arterially perfused Vagus nerve preparation in a grid extending over 2 mm in the rostrocaudal plane using the obex as a Nucleus ambiguus reference point. Microinjections were paired, one made during pacing to measure changes Heart rate in atrioventricular conduction (P-R interval) independent of changes in heart rate and the Glutamate other looking for changes in heart period (P-P interval) un-paced. Although evidence of a differential distribution was found in 7 cases, in the majority (13/20), sites producing maximal effects on both variables coincided. Maximal changes in atrioventricular conduc- tion resulted from more rostral sites in 6 cases and from a more caudal site in only one. Overall, the ratio of the change in atrioventricular conduction to the change in heart rate for a given site was significantly greater 1 mm rostral to the obex than at either end of the test grid. -
Cardiovascular System 9
Chapter Cardiovascular System 9 Learning Outcomes On completion of this chapter, you will be able to: 1. State the description and primary functions of the organs/structures of the car- diovascular system. 2. Explain the circulation of blood through the chambers of the heart. 3. Identify and locate the commonly used sites for taking a pulse. 4. Explain blood pressure. 5. Recognize terminology included in the ICD-10-CM. 6. Analyze, build, spell, and pronounce medical words. 7. Comprehend the drugs highlighted in this chapter. 8. Describe diagnostic and laboratory tests related to the cardiovascular system. 9. Identify and define selected abbreviations. 10. Apply your acquired knowledge of medical terms by successfully completing the Practical Application exercise. 255 Anatomy and Physiology The cardiovascular (CV) system, also called the circulatory system, circulates blood to all parts of the body by the action of the heart. This process provides the body’s cells with oxygen and nutritive ele- ments and removes waste materials and carbon dioxide. The heart, a muscular pump, is the central organ of the system. It beats approximately 100,000 times each day, pumping roughly 8,000 liters of blood, enough to fill about 8,500 quart-sized milk cartons. Arteries, veins, and capillaries comprise the network of vessels that transport blood (fluid consisting of blood cells and plasma) throughout the body. Blood flows through the heart, to the lungs, back to the heart, and on to the various body parts. Table 9.1 provides an at-a-glance look at the cardiovascular system. Figure 9.1 shows a schematic overview of the cardiovascular system. -

Cardiology-EKG Michael Bradley
Cardiology/EKG Board Review Michael J. Bradley D.O. DME/Program Director Family Medicine Residency Objectives • Review general method for EKG interpretation • Review specific points of “data gathering” and “diagnoses” on EKG • Review treatment considerations • Review clinical cases/EKG’s • Board exam considerations EKG EKG – 12 Leads • Anterior Leads - V1, V2, V3, V4 • Inferior Leads – II, III, aVF • Left Lateral Leads – I, aVL, V5, V6 • Right Leads – aVR, V1 11 Step Method for Reading EKG’s • “Data Gathering” – steps 1-4 – 1. Standardization – make sure paper and paper speed is standardized – 2. Heart Rate – 3. Intervals – PR, QT, QRS width – 4. Axis – normal vs. deviation 11 Step Method for Reading EKG’s • “Diagnoses” – 5. Rhythm – 6. Atrioventricular (AV) Block Disturbances – 7. Bundle Branch Block or Hemiblock of – 8. Preexcitation Conduction – 9. Enlargement and Hypertrophy – 10. Coronary Artery Disease – 11. Utter Confusion • The Only EKG Book You’ll Ever Need Malcolm S. Thaler, MD Heart Rate • Regular Rhythms Heart Rate • Irregular Rhythms Intervals • Measure length of PR interval, QT interval, width of P wave, QRS complex QTc • QTc = QT interval corrected for heart rate – Uses Bazett’s Formula or Fridericia’s Formula • Long QT syndrome – inherited or acquired (>75 meds); torsades de ponites/VF; syncope, seizures, sudden death Axis Rhythm • 4 Questions – 1. Are normal P waves present? – 2. Are QRS complexes narrow or wide (≤ or ≥ 0.12)? – 3. What is relationship between P waves and QRS complexes? – 4. Is rhythm regular or irregular? -
The ECG Made Very Easy Indeed: a Beginner’S Guide
Part 1 The ECG made very easy indeed: a beginner’s guide The ECG made very easy indeed 1 What is an ECG? 1 The heart is a pump driven by intrinsic electrical When do you need an ECG? 1 impulses which make the heart beat. An ECG is a paper recording of that electrical activity. The ECG records where How to record an ECG 2 electrical impulses start and how they flow through the How to interpret an ECG: the basics 2 heart. It does not measure how well the heart is pumping. The electrical activity of the heart starts in the ‘inter- The ECG waves and what they mean 2 nal pacemaker’, which is called the sinoatrial node. This Interpretation starts here! 4 is in the right atrium. The normal rhythm is called ‘sinus rhythm’ (properly it should be called sinoatrial rhythm, Rhythms you must be able to recognize 8 but it isn’t). The way electrical impulses flow through the Patterns you must be able to recognize 10 heart is called conduction. Abnormalities in the electrical activity of the heart can The normal ECG and its variants 13 result in abnormal conduction or rhythms where the heart ECG red flags 14 may go too quickly, too slowly, or beat irregularly. Changes to the normal flow of electricity through the heart can be shown on an ECG and may indicate damaged This guide has been written for those who are just starting heart muscle. Heart muscle can be damaged by many to use ECGs in their clinical practice. -

Significance of ST-Segment Depression During Supraventricular Tachycardia
Significance of ST-segment depression during supraventricular tachycardia. Clues offered by its return to normal at the end of the episode Gianaugusto Slavich, Daisy Pavoni, Luigi Badano, Malgorzata Popiel* Cardiology Unit, S. Maria della Misericordia Hospital, Udine, *I Division of Cardiology, Department of Medicine, University of Poznan, Poland Key words: The finding of transient ST-segment depression during episodes of supraventricular tachycardia ST-segment depression; is common but its ischemic significance is usually uncertain. Several authors came to the conclusion Supraventricular that in the absence of positive myocardial scintigraphy these alterations are not associated with a tachyarrhythmias. coronary flow-limiting stenosis. Our report tends to confirm this view but we suggest to observe the evolution of ST-segment changes at the very end of the episodes; these mechanisms have not been ad- equately addressed in previous studies and could provide useful clues to the ischemic or non-ischemic origin of ST-segment abnormalities. (Ital Heart J 2002; 3 (3): 206-210) © 2002 CEPI Srl The finding of transient ST-segment de- Description of cases pression during episodes of supraventricu- Received June 20, 2001; lar tachycardia is rather common but its is- Case 1. A 63-year-old male, with a nega- revision received January 17, 2002; accepted chemic significance is usually uncertain. tive cardiovascular history, no coronary January 19, 2002. Two clinical cases prompted us to ad- risk factors and practicing frequent and in- dress this issue and to review the pertinent tense recreational activity, presented with Address: literature. Our report suggests that the ob- complaints of recurrent sudden-onset pal- Dr. -

Long QT Syndrome: from Channels to Cardiac Arrhythmias
Long QT syndrome: from channels to cardiac arrhythmias Arthur J. Moss, Robert S. Kass J Clin Invest. 2005;115(8):2018-2024. https://doi.org/10.1172/JCI25537. Review Series Long QT syndrome, a rare genetic disorder associated with life-threatening arrhythmias, has provided a wealth of information about fundamental mechanisms underlying human cardiac electrophysiology that has come about because of truly collaborative interactions between clinical and basic scientists. Our understanding of the mechanisms that control the critical plateau and repolarization phases of the human ventricular action potential has been raised to new levels through these studies, which have clarified the manner in which both potassium and sodium channels regulate this critical period of electrical activity. Find the latest version: https://jci.me/25537/pdf Review series Long QT syndrome: from channels to cardiac arrhythmias Arthur J. Moss1 and Robert S. Kass2 1Heart Research Follow-up Program, Department of Medicine, University of Rochester School of Medicine and Dentistry, Rochester, New York, USA. 2Department of Pharmacology, Columbia University Medical Center, New York, New York, USA. Long QT syndrome, a rare genetic disorder associated with life-threatening arrhythmias, has provided a wealth of information about fundamental mechanisms underlying human cardiac electrophysiology that has come about because of truly collaborative interactions between clinical and basic scientists. Our understanding of the mecha- nisms that control the critical plateau and repolarization phases of the human ventricular action potential has been raised to new levels through these studies, which have clarified the manner in which both potassium and sodium channels regulate this critical period of electrical activity. -

Abnormalities Caused by Left Bundle Branch Block - Print Article - JAAPA
Marquette University e-Publications@Marquette Physician Assistant Studies Faculty Research and Physician Assistant Studies, Department Publications 12-17-2010 Abnormalities Caused by Left undB le Branch Block James F. Ginter Aurora Cardiovascular Services Patrick Loftis Marquette University, [email protected] Published version. Journal of the American Academy of Physician Assistants, Vol. 23, No. 12 (December 2010). Permalink. © 2010, American Academy of Physician Assistants and Haymarket Media Inc. Useded with permission. Abnormalities caused by left bundle branch block - Print Article - JAAPA http://www.jaapa.com/abnormalities-caused-by-left-bundle-branch-block/... << Return to Abnormalities caused by left bundle branch block James F. Ginter, MPAS, PA-C, Patrick Loftis, PA-C, MPAS, RN December 17 2010 One of the keys to achieving maximal cardiac output is simultaneous contraction of the atria followed by simultaneous contraction of the ventricles. The cardiac conduction system (Figure 1) coordinates the polarization and contraction of the heart chambers. As reviewed in the earlier segment of this department on right bundle branch block (RBBB), the process begins with a stimulus from the sinoatrial (SA) node. The stimulus is then slowed in the atrioventricular (AV) node, allowing complete contraction of the atria. From there, the stimulus proceeds to the His bundle and then to the left and right bundle branches. The bundle branches are responsible for delivering the stimulus to the Purkinje fibers of the left and right ventricles at the same speed, which allows simultaneous contraction of the ventricles. Bundle branch blocks are common disorders of the cardiac conduction system. They can affect the right bundle, the left bundle, or one of its branches (fascicular block), or they may occur in combination. -

Nitric Oxide-Mediated Flow-Dependent Dilation Is Impaired in Coronary Arteries in Patients with Coronary Spastic Angina
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector 920 JACC Vol. 30, No. 4 October 1997:920–6 Nitric Oxide-Mediated Flow-Dependent Dilation Is Impaired in Coronary Arteries in Patients With Coronary Spastic Angina KIYOTAKA KUGIYAMA, MD, MASAMICHI OHGUSHI, MD, TAKESHI MOTOYAMA, MD, SEIGO SUGIYAMA, MD, HISAO OGAWA, MD, MICHIHIRO YOSHIMURA, MD, YOSHITO INOBE, MD, OSAMU HIRASHIMA, MD, HIROAKI KAWANO, MD, HIROFUMI SOEJIMA, MD, HIROFUMI YASUE, MD Kumamoto City, Japan Objectives. This study sought to examine whether flow- Results. Flow-dependent dilation of the proximal LAD was dependent dilation is impaired at the site of coronary artery found to be less in spasm arteries than in control arteries. G spasm in patients with coronary spastic angina. Infusion of N -monomethyl-L-arginine (L-NMMA) in the proxi- Background. Physiologic stimuli such as exercise and exposure mal LAD suppressed flow-dependent dilation in control arteries to cold have been shown to cause an increase in coronary blood but had no significant effect on spasm arteries. The dilator flow, leading to flow-dependent dilation of coronary arteries in response to nitroglycerin was not impaired in spasm coronary normal subjects, but cause coronary constriction in patients with arteries. coronary spastic angina. Conclusions. Our results indicate that flow-dependent coronary Methods. A maximal increase in blood flow was induced dilation is impaired in spasm arteries, partly due to a deficiency in selectively in the left anterior descending coronary artery (LAD) endothelial nitric oxide bioactivity, which in turn may contribute by infusion of adenosine through a Doppler flow catheter tip in the to the increase in coronary tone during physiologic stimuli in midportion of the LAD in 10 patients with coronary spastic patients with coronary spastic angina. -

Parasystole in a Mahaim Accessory Pathway
223 Case Report Parasystole in a Mahaim Accessory Pathway Chandramohan Ramasamy MD, Senthil Kumar MD, Raja J Selvaraj MD, DNB Department of Cardiology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India Address for Correspondence: Dr. Raja J Selvaraj, Assistant Professor of Cardiology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry - 605006, India. E-Mail: [email protected] Abstract Automaticity has been described in Mahaim pathways, both spontaneously and during radiofrequency ablation. We describe an unusual case of automatic rhythm from a Mahaim pathway presenting as parasystole. The parasystolic beats were also found to initiate tachycardia, resulting in initial presentation with incessant tachycardia and tachycardia induced cardiomyopathy. Key words: Mahaim tachycardia, Parasystole, Automaticity Introduction Mahaim pathways are atriofascicular accessory pathways with decremental, anterograde only conduction. The most common clinical manifestation related to these pathways is antidromic reentrant tachycardia. Less commonly, the pathway may be a bystander with atrioventricular nodal reentrant tachycardia or atrial tachycardia. Rarely, automaticity has been reported from the pathway, manifesting as ectopic beats during sinus rhythm or as an automatic tachycardia [1,2]. Parasystole is a condition where an ectopic focus is unaffected by the underlying rhythm due to entrance block. Parasystole has been reported from atrial musculature, ventricular musculature -

Your Pulse and Target Heart Rate
Skip to main content ×Close Menu We use cookies to improve your experience on our website. By closing this banner or interacting with our site, you acknowledge and agree to this. Legal Notices MobileClose Menu Find A Doctor Your Visit Pay a Bill Log in to MyGillette Learn more about MyGillette Patient Education Patient Services and Resources Your Rights and Medical Records Understanding Costs, Insurance and the Gillette Assistance Programs Services to Support Your Family Interpreter Services International Patients Parent Resources and Support Prepare for Your Visit Prepare for Clinic Visits and Tests Prepare for Surgery Take a Hospital Tour Transfer Your Medical Records Transportation and Accommodations Ways to Prepare and Comfort Your Child During Your Visit or Hospital Stay Commitment to a Safe and Healing Environment Our Hospital Units Your Hospital Room St. Paul Campus Amenities and Activities Visit or Contact a Patient Conditions & Care All Conditions Cerebral Palsy Neuromuscular Disorders Scoliosis Craniosynostosis Brain Injury All Tests & Treatments Shunt Surgery for Hydrocephalus Gait and Motion Analysis Selective Dorsal Rhizotomy (SDR) Gillette Craniocap© Orthosis Botulinum Toxin and Phenol (Injected Spasticity Medications) All Specialties & Services Orthopedics Rehabilitation Services Craniofacial and Plastic Surgery Neurology Neurosurgery Virtual Visits Pediatric Expert Consults Virtual Rehab Therapy Sleep Medicine Virtual Care Get Involved Advocating for Your Family Community Health United Cerebral Palsy of MN Donors & Supporters